MINISTRY of HEALTH UKRAINE
advertisement

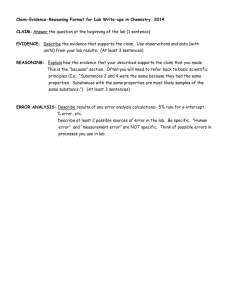
MINISTRY OF HEALTH OF UKRAINE BUKOVYNIAN STATE MEDICAL UNIVERSITY “Approved” on the methodical meeting of the Department of neurology, psychiatry and medical psychology nm. S.M.Savenko “____” ___________ 2009 (Report № __). Chief of the Department _______________________ Professor V.M. Pashkovsky METHODICAL INSTRUCTION for 4-th year students of medical faculty №2 (the speciality “medical affair”) for independent work during preparing to practical class Theme 19: ABUSE OF NON-DEPENDANCE-PRODUCING SUBSTANCES. MODULE 2. SPECIAL (NOSOLOGY) PSYCHIATRY TOPICAL MODULE 4. MENTAL AND BEHAVIOURAL DISODERS DUE TO PSYCHOACTIVE SUBSTANCES USE. Сhernivtsi, 2009 2 1. Actuality of theme: A lot of people use toxic substances in over world. Their amount constantly increases. To the student, future doctor, which begins to obtain knowledge, practical skills and abilities in clinics, it is necessary to master the basic forms of mental and behavioural disorders due to use of non-dependance-producing substances, able them to diagnose, to treatment. 2. Duration of practical classes - 2 hours. 3. EDUCATIONAL PURPOSE 3.1. To know: 1. Medical and social problems using toxic substances. 2. Etiological and pathogenesis factors due to dependence from toxic substances. 3. Mental and behavioural disorders due to abuse tranquilisers. 4. Mental and behavioural disorders due to abuse soporific. 5. Mental and behavioural disorders due to abuse cholinolitic. 6. Mental and behavioural disorders due to abuse products with coffeine. 7. Mental and behavioural disorders due to use inhalant and solvents. 8. Smoking as form of toxicomania. 9. Age peculiarities toxicomanies. 10. Principles and methodic of treatment toxicomanies. 11. Prophylactic of toxicomanies. 12. Expertise of toxicomanies. 3.2.Able: 1. Diagnose poisoning of tranquilisers, soporific, cholinolitic, inhalant. 2. To give urgent help at the extreme states (poisons). 3. Make up medical rehabilitation programs for patients with toxicomanies. 3.3.To capture practical skills: 1. To collect subjective and objective anamnesis. 2. To help about abstinence syndrome. 3. To give urgent help at the poisons toxic substances. 4. INTERSUBJECT INTEGRATION (base level of preparation). Names of previous disciplines 1. Medical chemic. 2. Clinical pharmacology. 3. Internal therapy. Skills are got 1.To know basic chemical features toxic substances. 2. Pharmacology toxic substances. 3. To describe features of diseases of organs and systems due to using toxic substances. 5. ADVICES TO STUDENTS. 5.1. CONTENTS OF THEME. Addictions. The harm that addiction to chemicals has on the body, the physical damage it does isn't the only reason for quitting addiction but also the harm it does to a person's mental health should also be taken into account too, as well as that of partners and relations living in the same house. One of the worlds most widely used legal drugs is nicotine; millions of people all over the world use it on a daily basis and spend billions every year by doing so. People use it for its calming, 3 tranquillising and mildly mood enhancing properties; despite this it is highly addictive and has prolonged withdrawal effects such as causing anxiety, mood swings and cravings for those wishing to give up. Glues and some household products that give off fumes are increasingly becoming a form of abuse particularly in youngsters and teenagers due to them being readily available and inexpensive. Solvents are usually sniffed and inhalation of the fumes produces feelings of inebriation, confusion, stupor and unconsciousness. A high number of young people die each year accidentally due to experimentation with solvents but very few people actually continue using solvents but move onto using other drugs. All sedatives can be misused and abused, but barbiturates and benzodiazepines are responsible for most of the problems with sedative abuse due to their widespread "recreational" or non-medical use. People who have difficulty dealing with stress, anxiety or sleeplessness may overuse or become dependent on sedatives. Heroin users take them either to supplement their drug or to substitute for it. Stimulant users frequently take sedatives to calm excessive jitteriness. Others take sedatives recreationally to relax and forget their worries. Barbiturate overdose is a factor in nearly one-third of all reported drug-related deaths. These include suicides and accidental drug poisonings. Accidental deaths sometimes occur when a drowsy, confused user repeats doses, or when sedatives are taken with alcohol. In the U.S., in 1998, a total of 70,982 sedative exposures were reported to U.S. poison control centers, of which 2310 (3.2%) resulted in major toxicity and 89 (0.1%) resulted in death. About half of all the people admitted to emergency rooms in the U.S. as a result of nonmedical use of sedatives have a legitimate prescription for the drug, but have taken an excessive dose or combined it with alcohol or other drugs. People often say that caffeine makes them feel more capable for intellectual and physical activity and less tired and drowsy. But, expects have shown that caffeine abuse has slowed reaction time to visual and auditory stimuli; it can also lead to diminishing your intellectual and physical performances. The symptoms of caffeine abuse called caffenism, are tiredness, craving, confusion, lethargy, and headaches. Belladonna is one of the most toxic plants found in the Western hemisphere. Children have been poisoned by eating as few as three berries. Ingestion of a leaf of the Belladonna can be fatal to an adult. The root of the plant is generally the most toxic part, though this can vary from one specimen to another. All parts of the plant contain tropane alkaloids. The berries pose the greatest danger to children because they look attractive and have a somewhat sweet taste. Symptoms of belladonna poisoning are the same as those for atropine (the best-known of the tropane alkaloids), and include dilated pupils, tachycardia, hallucinations, blurred vision, loss of balance, a feeling of flight, staggering, a sense of suffocation, paleness followed by a red rash, flushing, husky voice, extremely dry throat, constipation, urinary retention, and confusion. The skin can completely dry out and slough off. Fatal cases have a rapid pulse that turns feeble. The antidote is physostigmine or pilocarpine, the same as for atropine. The reason for most of these symptoms is because of atropine's effect on the parasympathetic nervous system. Atropine competitively inhibits the action of acetylcholine (ACh) at the acetylcholine receptor in the nerve synapse, thereby preventing the parasympathetic nervous system from sending out electrical nerve impulses. Since the parasympathetic nervous system regulates non-volitional/subconcious activities (such as sweating, breathing, and heart rate) when it is prevented from sending out signals, the heartbeat and breathing become extremely irregular. The Belladonna is toxic to many domestic animals and livestock; Belladonna poisoning can lead to colic, depression, weakness, and lack of coordination in horses, with fatalities reported even for small amounts from 1 to 10 pounds (0.5 to 5 kg). A. General Treatment Principles 1. Goals of Treatment 2. Assessment 3. Treatment Settings 4 4. 5. 6. 7. Formulation and Implementation of a Treatment Plan Pharmacological Treatments Psychosocial Treatments Clinical Features Influencing Treatment Treatments for Other Co-occurring Psychiatric Disorders in Patients With Substance Use Disorders Anticonvulsants The anticonvulsants carbamazepine, gabapentin, and valproate have been used to treat alcohol withdrawal and might work especially well in patients with co-occurring psychiatric disorders. Valproate has shown promise in stabilizing mood and reducing drinking in patients with bipolar disorder. Drug-drug interactions can occur between anticonvulsants (e.g., valproate and either lamotrigine or carbamazepine) or with other psychotropic medications, as a result of displacement from plasma protein binding sites and metabolism through UDP-glucuronosyltransferase and the cytochrome P450 2C9 enzyme. Antidepressants Monoamine oxidase inhibitors (MAOIs) may have interactions (e.g., with alcohol, cocaine and other stimulants, meperidine, dextromethorphan). Tricyclic antidepressants and MAOIs may be toxic in overdosage. Simultaneous use of antidepressants and substances of abuse may increase sedation or cardiovascular effects. Bupropion may theoretically increase the risk of psychosis in psychotic patients, but concomitant treatment with antipsychotic medication will reduce this risk. Drug-drug interactions mediated through the cytochrome P450 system are common (e.g., methadone and antidepressants metabolized via cytochrome P450 2D6 or 3A4). Antipsychotics Clozapine may have benefits in decreasing substance use among individuals for whom it is otherwise indicated. Smoking decreases blood levels of some antipsychotics (e.g., clozapine, olanzapine, haloperidol, fluphenazine, thioridazine, chlorpromazine) via the cytochrome P450 1A2 enzyme. Simultaneous use of some antipsychotics and substances of abuse may increase sedation or cardiovascular effects. Anxiolytics and Anxiolytics and sedative-hypnotics with abuse potential should be sedative- prescribed cautiously (e.g., dispense in limited quantities, keep hypnotics track of prescription refills, and monitor ongoing medical necessity and response to medication). These medications may have increased sedative and respiratory effects in combination with specific substances (e.g., alcohol, other sedatives, opioids). Drug-drug interactions may be mediated through the cytochrome P450 system (e.g., CYP 3A4, CYP 2C19). Stimulants Evidence suggests that appropriate use of stimulants in attentiondeficit/hyperactivity disorder does not augment later risk of substance use disorders. Limit abuse potential by prescribing these medications cautiously (e.g., dispense in limited quantities, keep track of prescription refills, and monitor ongoing medical necessity and response to medication). 8. Confidentiality B. Psychiatric Management 5.2. THEORETIC QUESTIONS: 1. Definition of notion narcology and toxicomania. 2. Medical and social problems using toxic substances. 3.Etiological and pathogenesis factors due to dependence from toxic substances. 4. Mental and behavioural disorders due to abuse tranquilisers. 5.Mental and behavioural disorders due to abuse soporific. 5 6.Mental and behavioural disorders due to abuse cholinolitic. 7.Mental and behavioural disorders due to abuse products with coffeine. 8.Mental and behavioural disorders due to use inhalant and solvents. 9.Smoking as form of toxicomania. 10.Age peculiarities toxicomanies. 11.Principles and methodic of treatment toxicomanies. 12. Urgent help at the poisons toxic substances. 13.Prophylactic of toxicomanies. 14.Expertise of toxicomanies. 5.3. Practical tasks on the class: 1. To collect anamnesis, clinical psychopathological examination of patients with toxicomanies. 2.To help about abstinence syndrome. 3.Make up of plan. Diagnose and treatment of patient with toxicomanies. 5.4.Material for self-contrrol. A. Questions of self-controls: 1.Definition of notion narcology and toxicomania. 2. Medical and social problems using toxic substances. 3.Etiological and pathogenesis factors due to dependence from toxic substances. 4. Mental and behavioural disorders due to abuse tranquilisers. 5.Mental and behavioural disorders due to abuse soporific. 6.Mental and behavioural disorders due to abuse cholinolitic. 7.Mental and behavioural disorders due to abuse products with coffeine. 8.Mental and behavioural disorders due to use inhalant and solvents. 9.Smoking as form of toxicomania. 10.Age peculiarities toxicomanies. 11.Principles and methodic of treatment toxicomanies. 12. Urgent help at the poisons toxic substances. 13.Prophylactic of toxicomanies. 14.Expertise of toxicomanies. B. TESTS: 1. The condition of dependence from toxic substances named: A. Asthenic syndrome B. Narcotic syndrome C. Hypochondriac syndrome D. Abstinential syndrome E. Depressive syndrome 2. What is cholinolitic of central action, which using with purpose toxicomania: A. Phenobarbital B. Tincture of belladonna C. Ephedrine D. Heroine E. Caffeine 6 3. What is purpose abusing of tranquilisers: A. Stimulation B. Hypnotic effect C. Anti depressive effect D. Euphoria E. General tonic effect 4. With purpose blocking of feel (inclination) to toxic substances using: A. Sedatives B. Anti depressants C. General tonic remedies D. Psychotherapy E. Nootropics B. SITUATIONAL TASKS 1. In hospital was convey patient K, 28 old year. Relatives told, that he using unknown pills in last times. Psychical status: patient excited, euphoric, has ataxia, reflexes reduced, bradycardia, hypotonia. Diagnose kinds of toxicomania. 2. Patient A., 63 old year used phenobarbital for good sleep during long time. He did not these pills duration last week. Psychical status: general weakness, breakness, tireness, insomnia, anxiety, muscle tics, pain in abdomen, nausea, vomiting. What syndrome in patient? 3. Patient has poison of cnolinolitics. Psychical status: optical hallucinations, delusion of relation of erotic content. Pupils dilated, non mobility, arterial pressure incresed. Your tactic? 8. RECOMMENDED LITERATURE IS: 8.1. Basic: 1. Clinical Psychiatry from Synopsis of Psychiatry by H.I.Kaplan, B.J.Sadock. – New York: Williams @ Wilkins. – 1997. 2. Psychiatry. Course of lectures. – Odessa: The Odessa State Medical University. – 2005. – 336 p. 3. Lectures. 4. Internet resource. 8.2. Additional: 1. Морозов Т.В., Шумский Н.Г. Введение в клиническую психиатрию. – Н.Новгород: Изд-во НГМА, 1998. 2. Попов Ю.В., Вид В.Д. Современная клиническая психиатрия. – М., 1997. 3. Сонник Г.Т. Психіатрія: Підручник / Г.Т.Сонник, О.К.Напрєєнко, А.М.Скрипніков. – К.: Здоров’я, 2006. Prepared by assistant S.D.Savka