Polymerase- an enzyme that makes our DNA and RNA replicate and
advertisement

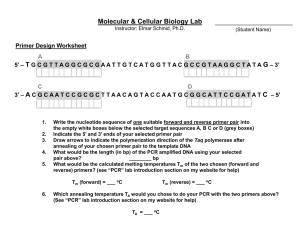
Comparing the sensitivity and specificity of three primer pairs on the detection of Plasmodium vivax using the polymerase chain reaction (PCR) Kimberly Leyster Saint Martin’s University Senior Seminar Spring 2007 Kimberly Leyster Table of Contents Abstract…………………………………………………………………………………...3 Introduction…………………………………………………………………………....3-16 Materials and Methods.……………………………………………………………....17-26 Results………………………………………………………………………………..26-33 Discussion…………………………………………………………………………….33-37 Acknowledgments………………………………………………………………………..37 Literature Cited…………………………………………………………………….…38-39 2 Kimberly Leyster Abstract With millions of people dying each year from malaria, a quicker and more accurate diagnosis is becoming more important. This study evaluated the use of polymerase chain reaction (PCR) as a more sensitive and specific method of diagnosing malaria caused by Plasmodium vivax when compared to microscopy. For this experiment, three PCR primer pairs were evaluated: UNR/PLF/VIR (hemi-nested PCR), rPLU5/rPLU6/rVIV1/rVIV2 (nested PCR), and PL1473F18/ PL1679R18 (real-time PCR). Serial dilutions of 1/1 to 1/1,000,000 were run with each primer pair to test for the sensitivity. PCR was then run using the two most sensitive primer sets and the results were compared to those of microscopy to determine specificity and sensitivity. Using the number of true positive and true negative diagnoses the overall concordance of each primer set was determined to find which primer set was most reliable. The sensitivities of the hemi-nested and real-time primers were 86% and 79% respectively. The specificities calculated for the hemi-nested and real-time primer set were 100% and 93% respectively and their overall concordances were 93% and 86% respectively. Although the primer sets were unable to accurately Diagnose samples when used individually, when used together they were able to accurately diagnose 96% of the samples. Introduction Worldwide, there are approximately 500 million people living with malaria and 1.5-2.7 million people who die each year from this disease (Swan et al. 2005). There are certain community aspects that allow this disease to exist. Although the disease used to be more widespread, it is now found predominately in Africa, Asia and Latin America 3 Kimberly Leyster because of poor health and low socioeconomic conditions in these areas (World Health Organization, 2006). The region of infection has narrowed, but the complications involved with malaria have grown. At the moment, microscopy is considered the “gold standard” for diagnosis, but this method is not very efficient. Because of this, scientists are researching the use of the polymerase chain reaction to allow for the detection of malaria more quickly and effectively; this is what my experiment addresses. Another concern that these countries now face is the inability to cure the disease in a timely manner. Over the past few years, there has been an increased resistance to antimalarial drugs, such as chloroquine, making them less effective at killing the parasites that cause malaria (World Health Organization, 2006). Malaria is transmitted from one person to another by the saliva of an infected female Anopheline mosquito, from the genus Anopheles (World Health Organization, 2006). Malaria parasites are injected into a person’s bloodstream and transported to the liver. From there, the parasites attack the cells and multiply. After 9-16 days, the parasites return to the blood and break down the red blood cells, which can lead to fever and anemia. Although there are roughly 380 species of Anopheline mosquitoes, only about 60 of them are known to transmit malaria causing parasites (World Health Organization, 2006). The protozoan parasites that causes malaria are members of the genus Plasmodium. Within this genus are four species: P. falciparum, P. vivax, P. ovale, and P. malaria. The most common and deadly of the four is P. falciparum; if left untreated, it can cause cerebral malaria, in which red blood cells block blood vessels in the brain (NOVA, 1997). The next most common is P. vivax. Although this strain is rarely fatal, it 4 Kimberly Leyster causes many social and economic problems due to possible organ failure and the total cost of treatment the decreasing the quality of life for those infected (World Health Organization, 2006). Malaria has traditionally been detected using microscopy (Center for Disease Control and Prevention, 2005). Although it is inexpensive, microscopic diagnosis is technically demanding and can only be done by trained personnel who can distinguish among the various species to ensure proper treatment. By using PCR to detect malaria, malaria can be diagnosed in a more timely and efficient manner. Detecting the disease earlier and having the means to properly diagnose the causative species would allow more lives to be saved. There have been many studies in which PCR was used to identify a Plasmodium genus, and some studies have found primers specific for each species. The purpose of my study was to find three primer sets that have been previously tested and reported to be sensitive and specific in detecting for P. vivax and compare them to the “gold standard” (microscopy). After choosing the three primer sets based on previous research, I performed PCR using each one and compared my results of their sensitivity and specificity to those reported by previous studies. Polymerases are enzymes that are necessary for life; catalyzing DNA and RNA production and repair (Rabinow, 1998). The chain reaction was invented in the 1980’s by Kary Mullis, who found a way to make the polymerase start and stop on specific parts of the DNA strand. He also noticed that specific regions of DNA were amplified exponentially. After many trials, scientists found a way to manipulate this reaction reliably and called it the polymerase chain reaction or PCR. This discovery was important enough to earn Mullis the Nobel Prize in 1993. With this breakthrough, 5 Kimberly Leyster scientists are able to amplify specific regions of DNA and use them to solve crimes, diagnose diseases, and develop new and better medicines (Rabinow, 1998). DNA is a blueprint to who we are as individuals; it is what makes us unique. From DNA, scientists are able to diagnose disease and investigators are able to solve crimes. If the amounts or concentrations of DNA samples are too small to work with, it can be difficult to identify a disease or match the DNA to a single person. By amplifying specific regions, PCR provides a virtually unlimited supply of that DNA (Brown, 1995). PCR allows us to locate a specific region of the DNA, and by knowing only the sequences that “flank” (Brown, 1995) or lay on either side of the region, we can replicate it. We do not need to know the sequence in between them because, by knowing the flanking sequences, the complementary bases naturally come together. Primers are a specific sequence of nucleotides that are complementary to the specific region of DNA we want to amplify. When the primer sequences are specific for the region of the chromosome we want to amplify, we can then proceed with PCR (Brown, 1995). There are three general steps that occur in every traditional PCR, which are repeated 24-45 times to get sufficient copies of the targeted region or gene. The first step in the process is called denaturation. This step is done at 95°C for about 1 minute (IPGRI, 2003). During this step, the double stranded DNA template is separated into two single stranded chains (Roche Diagnostics, 2006) by breaking the gydrogen bonds holding the two strands together. The next part is the annealing step. This is done for about 30 seconds between 45°C and 60°C, depending on the length and base composition of the primers; the longer the primers, the higher the annealing temperature should be. To calculate the annealing temperature, the equation Tm (melting temperature) = 4(G + C) 6 Kimberly Leyster + 2(A + T) °C can be used, but only if the melting points of the two primers are similar. During the annealing step, a target temperature for 5°C below the lowest Tm (Rybicki, 2001) is desired. The last step is extension, which lasts for about 1 minute at 72°C. During this step, Taq DNA polymerase replicates the strand. The Taq DNA polymerase starts from the primers and replicates the template DNA strand using complementary bases or nucleotides that are in the solution (dNTP’s), adding to the primers’ 3’ ends. After one cycle, there are two copies of the target DNA, and after each cycle, the numbers of copies double. After the second cycle, we start to get what are called “target DNA,” (Sumanas Inc., 2006) which means that the ends of the PCR products are defined by the primers. Since primers are used to begin the extension step, which replicates the target sequence, the primers cannot be a random chain of nucleotides. The primer has to be specific enough to attach only to the sequences flanking the target region, long enough so it does not anneal (stick) to unwanted places, and short enough so it can anneal to the sequence we want to amplify. Primers are typically about 20 nucleotides long (Sumanas Inc., 2006). There are additional guidelines to follow in designing primers. For instance, the purine to pyrimidine ratio should be close to one, and the primers should have 1-2 G or C’s on both the beginning and end of the sequence, if possible. There are software programs that can be used to design specific primer pairs such as “CPrimer,” which also calculate an annealing temperature to use with each primer pair (Henegariu, 2000). Since the primers can be of various lengths and compositions, the annealing temperatures for PCR will also vary. 7 Kimberly Leyster The temperature at which the annealing step takes place is very important. If the temperature is too high or too low, then the expected results may not be achieved (Henegariu, 2000). This can be a good thing however, because, by using various temperatures, concentrations of other ingredients, such as MgCl2 can be manipulated to obtain optimize results. With various temperatures, too many bands can appear, meaning the primer stuck to too many regions or no bands appear, meaning the temperature was too specific and did not allow for any annealing (Henegariu, 2000). Finding the ideal temperature takes trial and error. The annealing temperature may be different for each pair of primers, but the ingredients that go into each PCR tube are not. The easiest way to put the ingredients into each tube is by using a dry PCR bead that already has each ingredient in the correct amount. Each bead contains PCR buffer, dNTP mixture, and Taq DNA polymerase (Lairmore, 1990). The buffer is a solution that provides an optimal pH for the reaction to take place, along with ions for conductivity (Bowen, 2000). The dNTP mixture is an assortment of free deoxyribonucleotides (dATP, dCTP, dGTP, and dTTP). These nucleotides are used to extend the primers from their 3’ ends. Primers are added separately to the mixture (GeneCRC, 2004). The nucleotides are added to the primers by Taq DNA polymerase. This enzyme is extracted from Thermus aquaticus, which occupy hot springs, explaining why the enzymes are able to withstand such high temperatures (Brock, 1994). Lastly, ddH2O (double distilled water) is added to the beads, making a solution in which the reaction can occur without contaminants. After going through many cycles, it is time to evaluate the results of the PCR. To do this, agarose gel electrophoresis is use. The gel is made up of agarose powder mixed 8 Kimberly Leyster with electrophoresis buffer. After the gel has polymerized, positive and negative currents are hooked up to the gel box. The DNA is mixed with a loading buffer and loaded onto the gel at its negative end, since the DNA will have a negative charge. A current is run through the gel, causing the DNA to migrate toward the positive end (Bowen, 2000). Since the DNA is moving through a gel matrix, the smaller fragments will move faster, taking them farther down the gel. By mixing bromophenol blue and xylene cyanol dyes with the DNA in the loading buffer, the samples can be seen as they move through the gel. After a period of time, the gel is stained with ethidium bromide. This will bind to the double stranded DNA, so when it is put under an ultraviolet transilluminator, the DNA will fluoresce (Bowen, 2000). Along with unknown DNA fragments, a marker that contains known sizes of DNA fragments (also known as a ladder) is loaded into the gel (Dolan, 2006). The fragments move logarithmically, so the migration bands of unknown size can be measured and their sizes calculated. Sometimes, there are two different fragments that are the same size and in the same position; these appear as a single band. Other times, there will be no bands in a given lane, and this could be because the PCR did not work (Vierstraete, 1999). Along with traditional PCR, there is also nested PCR and real-time PCR. Nested PCR is used to ensure specific annealing of the primers, since a nonspecific primer may bind at more than one locus causing amplification of the wrong segment. Nested PCR uses two primers pairs. The external primer pair will amplify one region of the DNA, as with traditional PCR. The internal primer pair, which is more specific, then amplifies a product within the first product. Hemi-nested PCR means that either the forward or reverse primer from the internal primer pair is the same from the 9 Kimberly Leyster external primer pair. The purpose of doing the double amplification is that it reduces the chances of amplifying the wrong locus (Davidson College, 2002). If the external primer did amplify the wrong locus, then it is unlikely that the internal primers will amplify that same strand, meaning the majority of new products will be from the correct locus. Another form of PCR is real-time PCR. This is used in place of traditional PCR, because it is not as time consuming since it analyzes the data in the early stages of the reaction instead of waiting until the end (Applied Biosystems, 2006). Traditional PCR is not as sensitive as real-time PCR because of the variations in the end point, along with the fact that the results are not quantitative as with real-time PCR. Real-time PCR is more precise, because it measures the buildup of amplicons during the exponential phase, which is the optimal time to analyze and measure the data. Real-time PCR also differs from the traditional and nested forms, because there are different ingredients that need to be added in order to analyze the data with the real-time machine. One of the differences in ingredients is AmpliTaq DNA polymerase in place of traditional Taq DNA polymerase. This type of DNA polymerase is used because it contains 5’ exo-nuclease activity, which removes any obstacles on the template, such as DNA, that may interfere with the annealing of primers (Applied Biosystems, 2006). Another additional ingredient used in real-time PCR is Fluorescent Resonance Energy Transfer or FRET. When a high energy dye is in close proximity to a low energy dye, then the energy will transfer from high to low, triggering the probe to act. TaqMan probe is added to the master PCR mix and is designed to anneal to a specific region between the reverse and forward primers. The probe is positioned in the pathway of the enzyme and, when they collide, the probe is cleaved. The TaqMan probe is designed with a reporter 10 Kimberly Leyster dye at its 5’ end that is high energy, and a quencher dye at its 3’ end that is low energy (Applied Biosystems, 2006). Before the probe has been cleaved, there is no fluorescent emission because of the closeness of the high and low dye, but when the probe is cleaved, the fluorescent emission of the reporter increases and the quencher emission decreases. The increase in reporter emission is detected by the real-time machine and is proportional to the amount of product being formed. It is the combination of FRET and the TaqMan probe that allows for the machine to detect levels of fluorescent signal. Once the fluorescent signal is above the background intensity, the threshold point is determined using the most accurate reading, and the cycle that reaches this point is labeled the cycle threshold, Ct (Applied Biosystems, 2006). This new technology has allowed progress in both forensics and medicine. Investigators are now able to trace someone by using a single blood cell because of their ability to amplify it. The medical field is also expanding with this process because the PCR is highly sensitive, can rapidly multiply DNA is a short time, and requires only a small sample of DNA (Shariff, 2006). The process that is used during PCR only deals with a specific sequence, so no time is wasted on unnecessary fragments (Shariff, 2006). This allows diseases to be diagnosed more quickly and with greater accuracy. Microscopy has been the “gold-standard,” but researchers are looking for quicker and more accurate ways to detect malaria in patients, especially when microscopy-trained technicians are in short supply. In 1996, Rubio et al. (1999) conducted an experiment in Madrid, Spain to compare PCR with microscopy. Their subjects were 159 children under six years old from four different villages. The patients were examined, and thick and thin blood samples were prepared for microscopy. 11 Fingerprick samples were taken on filter Kimberly Leyster paper and stored in a plastic bag until used for PCR. The purpose of the study was to measure the specificity and sensitivity of PCR compared to microscopy. The PCR was performed twice. The first round used the genus-specific primers UNR: 5’- GACGGTATCTGATCGTCTTC -3’, PLF: 5’AGTGTGTATCCAATCGAGTTTC -3’, and HUF: 5’-GAGCCGCCTGGATACCGC-3’. The next round, which was independent from the first, used primer PLF again and a species-specific primer (VIR: 5’- AGGACTTCCAAGCCGAAGC -3’) along with primers for other species in a multiplex system. The species-specific primers were designed to amplify regions from each species’ mitochondrial 18S gene. The amplification started with the dried blood samples on filter paper, which were combined with 10 mM of Tris with a pH of 8.3, 50mM KCL, 1.5mM MgCl2, 0.001% (w/v) gelatin, 1% glycerol, 200µM of each dNTP, 25 units of AmpliTaq DNA polymerase (Perkin-Elmer, Norwalk, CT), and 41.1 µl of template DNA creating a final volume of 50µl. The second reaction mixture contained 10mM Tris-HCL (Ph 8.3), 50 mM KCl, 205 mM MgCl2, 0.001% (w/v) gelatin, 1% glycerol, 200µM of each dNTP, 1 units of AmpliTaq DNA polymerase, and template DNA (2µl of PCR from first reaction, diluted to 1ml with water, and 2µl was added) creating a final volume of 25µl. The total amplification for the first reaction involved 5 minute of denaturation at 90°C, followed by 40 cycles of 45 seconds of annealing at 94°C, and 45 sec at 62°C , and 60 sec at 72°C, followed by a final extension of 72°C for ten minutes. The second reaction followed the same initial denaturation but went through 35 cycles at 94°C for 20 sec, 62°C for 20 sec, and 72°C for 30 sec followed by the final extension of 72°C for ten minutes. 12 Kimberly Leyster This primer set was more reliable than the thin and thick microscopy because it detected 10% of the infected patients that the microscopy was not able to diagnose. The sensitivity of this primer set was found using all four types of Plasmodium and was found to be 100%. The specificity of this primer set was a little lower at 67%, but the positive predictive value, was 87% and the negative predictive value, the ability of the primer set to detect true negatives, was 100%. Specifically, the P. vivax was thought to be found in two children using microscopy and the diagnoses were confirmed using PCR. This article is useful for my experiment because it gave me a set of primers to test using PCR. Rubio et al. (1999) found these primers to be accurate; I tested their specificity and sensitivity. In addition, this study also used a traditional PCR protocol similar to the one I used when evaluating these primer pairs for specificity and sensitivity. Mangold et al. (2005) recognized the disadvantages of microscopy and conducted a study to test real-time primer pairs. They obtained controls from the American Type Culture Collection (ATCC; Manassas, Va.) including plasmids containing a partial 18S rRNA gene sequence from each of the four Plasmodium species. Along with these sequences, 10 DNA samples from human red blood cells known to contain P. falciparum and monkey blood samples infected with P. vivax or P. malaria were used. The samples were from 200 patients whose blood was being tested for something other than malaria and from 158 blinded samples, meaning the diagnoses is unknown to the analyst, from patients who had been experiencing fever and recently traveled to areas were malaria is endemic. About 40µl of blood from each sample was collected and allowed to dry on 13 Kimberly Leyster ISOCODE card (Schleicher &Schuel, Keene, N.H.). The DNA was then extracted and amplified using real-time PCR. The target gene for this reaction was 18S and the LightCycler (Roche Molecular Systems, Indianapolis, Ind.) was used. After comparing incomplete 18S rRNA gene sequences for each of the four Plasmodium species, consensus primers were diagnosed (PL1473F18 5’-TAACgAACgAgATCTTAA-3’ and PL1679R18 5’gTTCCTCTAAgAAgCTTT-3’). Each 20µl reaction contained 2 to 5 µl of sample DNA, 2 µl of 10X FastSTART DNA SYBR Green reagent (Roche), 6.5 mM MgCl2 (final concentration), and 0.5 mM of each primer. The PCR conditions were as follows: initial denaturation at 95°C for 10 min; 40 cycles of 10s at 95°C, 5 s at 50°C, and 20 s at 72°C wish fluorescence acquisition at the end of each extension step; melt program of 2 min at 95°C, 2 min at 68°C and a stepwise temperature increase of 0.2°C/s until 90°C with fluorescence acquisition at each temperature transition. After the PCR, melting curve analysis was used to determine the species specific mean melting temperature (Mangold et al., 2005). The melting point for P. vivax was found to be between 79 to 81°C. The sensitivity of this primer pair was found to be 100% and was even able to correct a misdiagnosis by microscopy. The specificity of this primer pair was 99.1%, showing this primer set to be reliable. This paper, once again, gave me a guide by which I designed my own real-time PCR. I adjusted some of the concentrations of certain ingredients to reach optimal results under the circumstances, but research gave me a good place to start and work from. This paper also supplied me with the melting point of P. vivax which I used when looking at 14 Kimberly Leyster my melting cure analysis. I used these primers in my experiment and tested to see how accurate they were compared to microscopy and the other primer sets I chose. In an experiment performed by Perandin et al. (2004), 122 whole blood samples were taken from patients who had just returned from places where malaria is endemic and had the symptoms associated with it. Five milliliters of blood were taken from each patient and stored for use with PCR; thin blood films were prepared at time of collection. Before PCR could occur, DNA was extracted from 200 µl of the blood sample using a High Pure PCR template preparation kit (Roche, Indianapolis, Ind.). Both nested and real-time PCR were performed. For nested PCR, a genus-specific primer set was used (rPLU5 5’-CTT GTT GTT GCC TT AAA CTT C-3’ and rPLU6 5’-TTA AAA TTG TTG CAG TTA AAA CG-3’) to detect samples carrying the Plasmodium parasite. Next, was a species-specific amplification with primers specific for each species of the malaria-causing parasite. The primer pair used for both genus and species-specific primers amplified regions of the 18SrRNA gene. The PCR mixture was as follows: 250 nM each oligonucleotide primer (P. vivax: rVIV1 5’-CGC TTC TAG CTT AAT CCA CAT AAC TGA TAC-3’ and rVIV2 5’-ACT TCC AAG CCG AAG CAA AGA AAG TCC TTA-‘3), 125 µM dNTP’s, 10X PCR buffer (500mM KCl, 100mM Tris-HCl with pH 8.3, 20 mM MgCl2), and Taq DNA polymerase. In each PCR tube, 95 µl of the reagent mixture was used along with 5 µl of template DNA. Initial denaturation took place at 95°C for 5 minutes. Then, a total of 25 cycles were performed using the following times and temperatures: annealing at 58°C for 2 minutes, extension at 72°C for 2 minutes, denaturation at 94°C for 1 minute. After the 25 cycles were completed, a final annealing at 58°C for 2 minutes and final 15 Kimberly Leyster extension at 72°C for 5 minutes occurred. Perandin et al. (2004) performed a second nested PCR with a total of 30 cycles. Real-time PCR was also evaluated in this experiment. The use of Primer Express software (Applied Biosystems, Foster City, Calif.) was used to design the primers and TaqMan fluorescence-labeled probes. These primers were also used to amplify a specific region of the 18S rRNA gene in Plasmodium. The forward and reverse primers used to detect P. vivax were VIV-F 5’-ACG CTT CTA GCT TAA TCC ACA TAA CT-3’ and VIV-R 5’-ATT TAC TCA AAG TAA CAA GGA CTT CCA AGC-3’. The probe used to detect this was VIV probe (TET) 5’-TTC GTA TCG ACT TTG TGC GCA TTT TGC3’. The DNA templates were amplified in an Applied Biosystems 7700 analytical PCR system with the species-specific primers and the probe. Each PCR tube contained the following: 5 µl template DNA, 25 µl of TaqMan 2× universal PCR master mix, 200nM concentration of each species-specific primer set and a 200 nM concentration of each corresponding probe. The amplification was then performed using the following steps: 2 minutes at 50°C to accomplish optimal AmpErase uracil-N-glycosylase activity, 10 minutes at 95°C to stimulate the AmpliTaq Gold DNA polymerase, and 45 cycles of 15s at 95°C and 1 minute at 60°C. The sensitivity found when using serial dilutions down to 0 parasites/µl of blood was 1.5 parasites/µl of blood in the P. vivax. To evaluate the specificity of these primer pairs, the PCR results were compared to the microscopy. Among the 122 patients, 61 were found to be positive for Plasmodium by microscopy, and 11 of these were diagnosed with P. vivax. When comparing the nested and the real-time PCR, the results were the exact same so when I compare them to microscopy, I will refer to them together 16 Kimberly Leyster as PCR. The number of total positive diagnoses was the same in PCR as it was in the microscopy, but when looking at the different species, the PCR and microscopy had different amounts of positives for each species. The number of negatives in the microscopy was 61, but the PCR found 60 negative but 1 P. falciparum. The sensitivity of this primer pair was found to be 73% while the specificity was 98%. The reason I chose to study this primer pair was because of its high level of specificity, not its sensitivity. The paper helped me develop my hypothesis, because the inability to calculate specificity indicated to me that this primer pair might not be as reliable and sensitive as the other two I chose to research. After researching PCR and learning more about it, I was able to evaluate various primers and know what to look for. I found three primer pairs that have been tested for specificity and sensitivity which I based my hypothesis. My hypothesis was the primer pair PL1473F18 and PL1679R18, together amplifying a section from the 18S gene, was going to be the most sensitive and specific. I chose this set because it was 100% sensitive, and 99.1% specific in detecting P. vivax in previous studies. These results were obtained in a different laboratory than the one in worked in, using different brands of material, and under different conditions. By testing this primer, along with the other two, I determined whether the results achieved by previous experiments can be repeated under different conditions. For a primer pair to be of value for disease diagnoses, the results need to be consistent across various conditions. Out of the three primer sets, I predicted that PL1473F18 and PL1679R18 would be the most reliable and accurate in detecting the Plasmodium vivax parasite. 17 Kimberly Leyster Materials and Methods The following experiment was performed at the Fort Lewis Center for Health Promotion and Preventive Medicine-West (CHPPM-W) with the help of Miguel Quintana and Naomi Iihoshi. Samples and controls: After researching the disease and finding many articles dealing with PCR experiments involving P. vivax, I chose three primer sets, which were supplied by CHPPMW, that had the highest sensitivity and specificity. The name, sequence, length, nuclear position, and melting temperature (if applicable) of each primer is listed in Table 1. Table 1. The following primer pairs were chosen after researching previous studies using PCR to detect P. vivax. These sequences were the most sensitive and specific of the primer sets researched. Name UNR PLF VIR Sequence (5’-3’) GACGGTATCTGATCGTCTTC AGTGTGTATCCAATCGAGTTTC AGGACTTCCAAGCCGAAGC Predicted Length 499 bp Tm (Hemi-nested) (Rubio et al., 1999) PL1473F18 PL1679R18 (Real-time) TAACgAACgAgATCTTAA gTTCCTCTAAgAAgCTTT 79.081.0°C *lower cases indicate basepair mismatches used to make melting curve (Mangold et al., 2005) rPLU5 rPLU6 rVIV1 rVIV2 CTTGTTGTTGCCTTAAACTTC TTAAAATTGTTGCAGTTAAAACG CGC TTC TAG CTT AAT CCA CAT AAC TGA TAC ACT TCC AAG CCG AAG CAA AGA AAG TCC TTA 120bp (Nested) (Perandin et al.,2004) U.S. Army CHPPM-W supplied the 30 samples of DNA extracted from human blood that I tested for Plasmodium vivax. They also supplied me with a positive control, human blood found positive for P. vivax using both thin and thick film microscopy, and a negative control, which was water. The purpose of using water was to see if any 18 Kimberly Leyster contamination occurred during the PCR process. After running a serial dilution, a procedure that evaluated the sensitivity of each primer pair, I chose the two most sensitive primer sets (UNR/PLF/VIR and PL1473F18/PL1679R18) for further analysis. Serial dilution: For my serial dilution, I used two positive controls, #1 and #2, which were known to be positive for P. vivax and one negative control, water. For each positive control, I diluted the of DNA with DNase/RNase free water (Molecular Biolgoy Reagent Sigma, cat # W4502). The first tube contained only the positive control and from that tube I used a micropipettor to take 5µl of the control and put it in a new tube with 45 µl of water, creating a 1:10 dilution. I continued with 1:10 serial dilutions until I reached a final dilution of 1:1,000,000. This concluded the preparation for my serial dilutions, and before I ran PCR to test each primer pair for sensitivity, I programmed the PCR machines. Programming the thermocyclers I programmed the thermocyclers according to Table 2 for all my reactions before I started. For the hemi-nested primers UNR, PLF, and VIR, I used a Thermal Cycler Gradient DNA Engine Tetrad (MJ Research, PTC-225 Peltier Thermal Cycler) (Table 1a1b); nested primers rPLU5, rPLU6, rVIV1, and rVIV2 used a Minicycler (MJ Research, PTC-150 Minicycler) for the first amplification and a DNA Engine Tetrad for the second amplification (Table 2c-2d); real-time primers PL1473F18 and PL1679R18 under conventional PCR used the MJ Mini Gradient Thermal Cycler (Biorad, PTC-1148 MJ Mini Thermal Cycler) (Table 2e). The machines were all programmed for a volume of 25µl and a heated lid at 100°C. 19 Kimberly Leyster Table 2. The PCR cycles programmed into various thermocyclers according to each primer set’s protocol. The first and second amplification for the hemi-nested primers are described in A and B respectively. The nested primer pairs for the first and second amplification are described in C and D respectively. The real-time primer pair for the conventional method is described in E. A Hemi-nested first amplification Phase Temp (°C) Time Cycles Initial Denature 94 5’ 1 Denature 94 45” 40 Anneal 62 45” Extend 72 60” Final Extension 72 5’ 1 Store 4 Indefinite 1 B Hemi-nested second amplification Phase Temp (°C) Time Cycles Initial Denature 95 5’ 1 Denature 94 20” 35 Anneal 62 20” Extend 72 30” Final Extension 72 5’ 1 Store 4 Indefinite 1 C Nested first amplification Phase Temp (°C) Time Cycles Initial Denature 95 5’ 1 Denature 94 1’ 25 Anneal 58 1’ Extend 72 2’ Final Extension 72 5’ 1 Store 4 Indefinite 1 D Nested second amplification Phase Temp (°C) Time Cycles Initial Denature 95 5’ 1 Denature 94 1’ 30 Anneal 58 1’ Extend 72 1’ Final Extension 72 5’ 1 Store 4 Indefinite 1 E Real-time using conventional PCR Phase Temp (°C) Time hold Cycles Initial Denature 95 10’ 1 Denature 95 10” 40 Anneal 50 5” Extend 72 20” Melt Curve 72 5’ 1 Store 4 Indefinite 1 20 Kimberly Leyster Preparing and running the primer pairs for serial dilution The total number of reactions I performed for each primer set was 16, but to ensure I had enough mix for each tube, I used 20 to calculate the volumes for my master mixes. After preparing master mixes according to Table 3(A, C, E), I added the total volume per reaction of the mix to a PuReTaq Ready-To-Go PCR bead tube (Amersham Biosciences, cat # 27-9557-02). Each bead contained the following ingredients: buffer, MgCl2, nucleotides, M-MuLV reverse transciptase, RNAguard and Taq DNA Polymerase. After the beads had dissolved, I added the appropriate amount of positive control DNA and negative control (sterile nuclease-free water) to each respective tube so the total volume of each tube was 25 µl (Table 3 A, C, E). I then briefly centrifuged the tubes to collect the ingredients at the bottoms of the tubes and kept them on ice until putting them in the thermocycler. After the thermocyclers were finished, I put the tubes on ice and prepared the master mix for the second amplification for the hemi-nested and nested PCR (Table 3 B and D). After adding the appropriate amount master mix to a new bead tube, I added enough of the first amplicon to each tube so the total volume of each tube was 25µl. I briefly centrifuged the tubes and ran them through PCR according to Table 2. 21 Kimberly Leyster Table 3. The master mix contained PCR grade water and primers. For each primer set, the total volume was always 25µl, but the amount of each component differed depending on the primers. For hemi-nested primers, I used the appropriate amounts for the first and second amplification from A and B respectively. For the nested primers, I used the amounts in C and D for the first and second amplification respectively. The real-times primers were both run using conventional PCR and the LightCycler using the concentrations in E and F respectively. It is from these mixes that I took the appropriate amounts for the serial dilutions. A Hemi-nested first amplification Component Volume (µl) # of reactions Total volume per reaction (µl) Water (PCR grade) 22.0 20 440 25 µM UNR 0.5 20 10 25 µM PLF 0.5 20 10 TOTAL 23.0 B Hemi-nested second amplification Component Volume (µl) # of reactions Total volume per reaction (µl) Water (PCR grade) 23.0 20 460 25 µM PLF 0.5 20 10 25 µM VIR 0.5 20 10 TOTAL 24.0 C Nested first amplification Component Volume (µl) # of reactions Total volume per reaction (µl) Water (PCR grade) 22.0 20 440 25 µM rPLU5 0.5 20 10 25 µM rPLU6 0.5 20 10 TOTAL 23.0 D Nested second amplification Component Volume (µl) # of reactions Total volume per reaction (µl) Water (PCR grade) 22.0 20 440 25 µM rPLU5 0.5 20 10 25 µM rPLU6 0.5 20 10 TOTAL 23.0 E Real-time using conventional PCR Component Volume (µl) # of reactions Total volume per reaction (µl) Water (PCR grade) 19.0 20 380 25 µM rPLU5 0.5 20 10 25 µM rPLU6 0.5 20 10 TOTAL 20.0 22 Kimberly Leyster F Real-time using the LightCycler Reagent Primer final concentration Water N/A SyBR Premix 1X Ex Taq 2X 25 µM PL1473F18 0.5 25 µM PL1679R18 0.5 TOTAL N/A Volume (µl)/ reaction 4.00 10.00 # of Reaction 20 20 Total volume (µl) 80 10 0.50 0.50 15.00 20 20 10 Along with the nested and traditional PCR, I also ran real-time PCR for primer pair PL1473F18 and PL1679R18. I used the master mix from Table 3 F and added an additional 5µl of the positive and negative control to each capillary tube. I then ran the tubes using the following conditions: 1) Initial denaturation at 95°C for 10 min; 2) amplification for 40 cycles of 10 s at 95°C, 5 s at 50°C and 20 s at 72°C; and 3) melting program of 2 min at 95°C, 2 min at 68 and a stepwise temperature increase of 0.2°C/s until 90°C. (Mangold, 2005). To analyze the real-time products, I compared the melting curve and the fluorescence of each product to the negative and positive control to determine the sensitivity of the primer pair. After the PCR was finished with the hemi-nested, nested, and traditional PCR were complete, I analyzed the products by using agarose gel electrophoresis. Gel electrophoresis: To prepare a 2% (w/v) agarose gel, I used 1X TBE buffer (Sigma, cat # t-3913) and a 2 gram pre-weighed bottle of low melting agarose (Fisher Scientific, BP1360-100). I measured out 100 ml of 1X TBE buffer and added it to the buffer in a flask. I placed it in a microwave for 1 minute , swirling the flask every 30 seconds until the agarose was completely dissolved. After all the agarose had dissolved, I added 5 µl of 10mg/ml 23 Kimberly Leyster Ethidium Bromide (Sigma, cat # E-1510) and swirled to mix. I poured the 2% agarose gel into a gel tray containing a comb at one end. I let it polymerize for 20 minutes and, after it had solidified, I put it in an electrophoresis chamber with the well end towards the negative electrode. I then added enough 1X TBE buffer to just cover the gel. I removed the comb and made sure the wells were filled with buffer. I used a microplate and placed 3 µl of gel loading solution (Sigma, Saint Louis, Missouri) into 16 wells, one per tube, for each primer pair. I then added 10 µl of sample to each microplate well and mixed it with the loading solution. After the samples had been mixed, I loaded 10 µl to each corresponding well in the gel. After loading the wells with my samples, I loaded the end well with a 100 bp marker (Roche Applied Science, cat # 1721 933). After placing the cover on the electrophoresis chamber and connecting the leads so the DNA would migrate towards the positive electrode, I ran the gel at 100 volts for 30 minutes. So the DNA didn’t diffuse after running, I immediately placed the gel on a UVP High Performance UV transilluminator (UVP, Upland, CA) inside a EDAS 290 Imaging Cabinet. I then took a digital picture using a Kodak DC290 Zoom Digital Camera with a EDAS 290 close-up lens and a EDAS ethidium bromide filter (Kodak, Rochester, NY). After the pictures were taken I analyzed them using a Kodak ID Image Analysis Software. Evaluating the serial dilutions Once the gels had run and the real-time PCR had finished, I evaluated my results. To assess the gels, I evaluated which dilutions of DNA template had been detected by each primer set. To evaluate the real-time primer pair, I used the melting temperature found for each dilution to see if parasites had been detected. If the melting temperature 24 Kimberly Leyster of the dilutions was similar to the positive control (+/- .05°C), I concluded that the parasites had been detected at that particular dilution. Choosing my primer pairs and testing the samples After running the serial dilutions and PCR the first time, I did not achieve the expected results. I repeated the serial dilutions with more concentrated controls for each primer pair and changed the protocol for the nested primer pair. First, the volume of primer was changed from 0.5 to 0.3 µl because, when previously tested, this gave stronger and more specific bands. Therefore, the amount of water was increased to 22.4 µl, so the final volume remained 25µl. Finally, the denaturation, annealing, and extension times were changed from 1 minute to 30 seconds, because the product was only 120bp and it did not need to run that long. After running the PCR again, I chose the two most sensitive primer pairs to test my samples with. I got the highest sensitivity when I used the hemi-nested primers UNR, PLF, VIR and the real-time primers PL1473F18 and PL1679R18, so I continued my experiment with these two primer sets. I made the master mixes (Table 3) and ran the two primer pairs using the same protocol as before (Table 2), except I used 40 reactions instead of 20 since I was using the master mix for 32 samples. Another difference was that instead of using the diluted DNA, I used my 30 samples along with a known positive and a negative control, water. I ran the PCR and, when the hemi-nested primer pair was finished, I visualized the results using electrophoresis using the same protocol as before. After the real-time PCR had completed, I used the melting points and fluorescence to determine the sensitivity and specificity of the primer. 25 Kimberly Leyster After evaluating my results, it was decided that there was contamination in my data and a repeat of both primer sets was necessary. After I repeated the PCR with the hemi-nested and real-time primer sets, I decided to also run the real-time products using gel electrophoresis, using the same protocol as with the hemi-nested primer set, to characterize uncertain samples. Data analysis To analyze the accuracy of each primer set, I calculated the sensitivity, specificity, and overall concordance. I first determined the number of true positives, true negatives, false positive,s and false negatives. I calculated the sensitivity by dividing the number of true positives found by PCR by the number of total positives found by the microscopy. The sensitivity is the primer sets ability to detect only true positives and nothing else. The specificity was found by dividing the number of true negatives found by each primer set using PCR by the number of total negatives found using microscopy. The specificity of each primer set is the ability to detect only true negatives and nothing else. Overall concordance is the primer sets capability to characterize a given sample correctly. To calculate the overall concordance, the number of true positives plus the number of true negatives for each primer set when compared to microscopy was divided by the number of total samples. Results Serial dilutions After running PCR with my serial dilutions, I used an E-gel to run the products so I could evaluate the ability of the hemi-nested primer set UNR, PLF, VIR to detect low concentrations of parasites. The results (Figure 1) show that these primers were able to 26 Kimberly Leyster amplify DNA from a parasite dilution of 1:10 with the positive control #1 (Fig 1A lane 2) and a parasite dilution of 1:100 with the positive control #2 (Fig 1B lane 3). A) B) Figure 1. Serial dilutions were run on a 2% TBE agarose gel using Hemi-nested PCR primer set UNR, PLF, and VIR. A) PCR with positive control #1 using template DNA. B) PCR with positive control #2 using template DNA. Lanes 1/9 were a 1:1 dilution, 2/10 were a 1:10 dilution, 3/11 were a 1:100 dilution, 4/12 were a 1:1,000 dilution, 5/13 were a 1:10,000 dilution, 6/14 were a 1:100,000 dilution, 7/15 were a 1:1,000,000 dilution and 8/16 were a negative control (water). Lane M contains the 100bp marker. I then used gel electrophoresis to analyze the ability to detect low concentrations of parasites for the nested primer pairs (rPLU5, rPLU6, rVIV1, rVIV2) and the conventional primer pair (PL1473F18 and PL1679R18). Figure 2 shows that the nested primers were able to detect parasite concentration levels at a 1:10 dilution with both positive #1 (Fig 2 Lanes 1-8) and #2 (Fig 2 Lanes 11-18) controls. 27 Kimberly Leyster M 1 2 3 4 5 6 7 8 9 M 10 11 12 13 14 15 16 17 500bp 100bp Figure 2. Serial dilutions were run on a 2% TBE agarose gel using Nested PCR primer pairs rPLU5, rPLU6, rVIV1, rVIV2. Lanes 1/10 were a 1:1 dilution, 2/11 were a 1:10 dilution, 3/12 were a 1:100 dilution, 4/13 were a 1:1,000 dilution, 5/14 were a 1:10,000 dilution, 6/15 were a 1:100,000 dilution, 7/16 were a 1:1,000,000 dilution and 8/17 were a negative control. Lane M contains the 100bp marker. The conventional primer pair was not able to detect any parasites using positive control #1 (Fig 3A), but were able to detect parasites at a dilution of 1:1 (Fig 3B Lane 1) with positive control #2 as shown in Figure 3. A) M 1 2 3 4 5 6 7 8 B) M 1 2 3 4 5 6 7 8 Figure 3. Serial dilutions were run on a 2% TBE agarose gel using conventional primer pair PL1473F18 and PL1679R18. A) PCR with positive control #1 using template DNA. B) PCR with positive control #2 using template DNA. Lanes M indicates were the 100 bp markers were placed. Lanes labeled 1 were a 1:1 dilution, 2 were a 1:10 dilution, 3 were a 1:100 dilution, 4 were a 1:1,000 dilution, 5 were a 1:10,000 dilution, 6 were a 1:100,000 dilution, 7 were a 1:1,000,000 dilution, and 8 were a negative control. 28 Kimberly Leyster Real-time PCR was also used to test the primer pair PL1473F18 and PL1679R18. The lowest parasite concentration detected using positive control #1 was found at a 1:100 dilution and the lowest concentration detected for positive control #2 was at a 1:10 dilution (Table 4). Table 4. Real-Time PCR using primer pair PL1473F18 and PL1679R18. Each rotator was loaded with the corresponding positive dilution (PC) or negative control (NC). The samples were then run through the LightCycler system to obtain the following results. Those dilutions with no data in the melting temperature (Tm ) indicates no detection of the sample. Rotator Position 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Sample Name PC 1 1:1 PC 1 1:10 PC 1 1:100 PC 1 1:1000 PC 1 1:10000 PC 1 1:100000 PC 1 1:1000000 NC 1 PC 2 1:1 PC 2 1:10 PC 2 1:100 PC 2 1:1000 PC 2 1:10000 PC 2 1:100000 PC 2 1:1000000 NC 2 Tm(°C) 80.43 80.36 80.53 80.35 80.49 Sensitivity After running the serial dilutions, I ran PCR on my 30 samples plus the negative and positive control using the hemi-nested primers set UNR, PLF, VIR and the real-time primer pair PL1473F18 and PL1679R18. I then evaluated the hemi-nested products using gel electrophoresis. For the real-time primers, I used data from the LightCycler (Rosche Molecular Biochemicals, product # 2043 912) and ran the products using gel electrophoresis. The sensitivity of each primer was calculated using the number of positive samples found with each PCR method compared to the number of positive samples found 29 Kimberly Leyster using microscopy. After running the gels, there was one sample that could not be defined as either positive or negative, so that sample was not included in the calculations. The gel electrophoresis with the hemi-nested products showed positive amplification of P. vivax in wells 2-3, 5-7, 9-11, 15-16, 20, 23-24, and 32. 1 2 3 4 5 6 7 8 M 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 M 25 26 27 28 29 30 31 32 500bp 100bp Figure 4. Samples run on a 2% TBE agarose gel using PCR products amplified with the hemi-nested primer set UNR, PLF, VIR. Each lane contained a different sample of blood which had gone through PCR; some samples were positive and some were negative for P. vivax. Those lanes labeled M is were the 100 bp markers where loaded. The negative control was loaded in lane 31 and the positive control was loaded in lane 32. The results from the real-time PCR are shown in Figure 5 using the melting curve analysis. The samples with melting temperatures between 78.5°C and 81.5°C were considered positive. 30 Kimberly Leyster Positive samples Negative samples Figure 5. Real-time amplification using the primer pair PL1473F18 and PL1679R18 using melting point analysis. The positive and negative samples of DNA for P. vivax are indicated. The graph was generated using LightCycler software. Figure 6 shows the gel electrophoresis of PCR products amplified with primers PL1473F18 and PL1679R18 after they had been run through the LightCycler. Wells 2-3, 5-11, 14-16, 24, and 32 all show positive for P. vivax. M 1 2 3 4 5 6 7 8 M 9 10 11 12 13 14 15 16 M M 17 18 19 20 21 22 23 24 M 25 26 27 28 29 30 31 32 M 500bp 100bp Figure 6. Gel electrophoresis using the products from LightCycler real-time PCR with the primer pair PL1473F18 and PL1679R18. Each lane was loaded with a different blood sample; some were positive and some were negative for P. vivax. The lanes labeled M is were the 100 bp marker was loaded. Lane 31 was loaded with a negative control, and lane 32 was loaded with a positive control. 31 Kimberly Leyster The total number of samples used in both PCR reactions was 29, with 14 total positives and 15 total negative samples. After comparing results from PCR and gel electrophoresis, I concluded that the hemi-nested primers amplified 12 true positives, 15 true negatives and 2 false negatives (Table 5). The sensitivity of the hemi-nested primers was calculated to be 12/14 = 86 %. Table 5. A comparison of microscopy results and the results from the hemi-nested primers. Shown are true positives, true negatives, false positives, and false negatives, along with the total number of positives and negatives for both microscopy and PCR. These data were used to calculate the sensitivity and specificity. Microscopy results Hemi-nested results POSITIVE POSITIVE 12 NEGATIVE 2 True Positives False Negatives NEGATIVE 0 15 False Positives True negatives 15 12 17 29 TOTAL TOTAL 14 After looking at the gel electrophoresis using the real-time primer pairs I found there were 11 true positives, 1 false positive, 14 true negatives and 3 false negatives (Table 6). The sensitivity of the real-time primer pairs was 11/14 = 79 %. Table 6. A comparison of microscopy results and the results from the real-time primers. Shown are true positives, true negatives, false positives, and false negatives, along with the total number of positives and negatives for both microscopy and PCR. These data were used to calculate the sensitivity and specificity. Microscopy results Real-time results POSITIVE NEGATIVE TOTAL POSITIVE 11 3 True Positives False Negatives NEGATIVE 1 14 False Positives True negatives 15 12 17 29 TOTAL 32 14 Kimberly Leyster Specificity Using the values shown in Tables 5 and 6, the specificity for the hemi-nested primer pairs was calculated to be 15/15 = 100 % and for the real-time primer pairs 14/15 = 93 %. Overall concordance The overall concordance for the hemi-nested primer pairs was 27/29 = 93 % and the real-time primer pairs had a concordance of 25/29 = 86 %. When evaluating the gels, not only were the negative and positive determinations important, but also the brightness and clarity of the bands. The hemi-nested PCR resulted in clear and bright bands, but there were some smearing and non-specific bands as well. The bands from the real-time PCR were specific and clear, but not as bright. Discussion In my study, the results failed to support my hypothesis, because not one primer set was more sensitive and specific than the others. When evaluated with serial dilutions, the primer set UNR, PLF, and VIR had equivalent sensitivity to the primer pair PL1473F18 and PL1679R18, with both sets being able to detect 1:10 and 1:100 parasite dilutions. The previous studies performed by Mangold et al. (2005) and Rubio et al. (1999) did not record the primers ability to detect parasites at low concentrations so I could not compare my results with the previous studies, but I used the results from the serial dilution to investigate the sensitivity and specificity further. After evaluating the PCR products with gel electrophoresis or the LightCycler, there was one sample that could not be designated as either positive or negative (Figure 4 lane 3, Figure 6 lane 3). Although microscopy showed the sample to be positive, I could not definitely characterize the band using either the real-time primer pair or the hemi- 33 Kimberly Leyster nested primer set. Further investigation of this sample is recommended. Because the sample was not characterized, I did not include it in final calculations of sensitivity, specificity, and overall concordance. The sensitivities I found for the hemi-nested and real-time primer sets, 86% and 79% respectively, were different than the 100% that had been reported for both primers in previous studies, (Rubio et al., 1999; Mangold et al. 2005). This could be because I used different conditions and different methods. Furthermore, different samples were evaluated, and the technicians who previously tested the primer sets were likely to have been more experienced. I had to repeat parts of my experiment due to contamination, and there is no way to know whether my final outcomes were free of error. Although I was careful in my pipetting, it is possible my lack of expertise contributed to the low sensitivity I found with the primer sets. Another explanation could be that the microscopy results to which I compared the PCR results were inaccurate. There was one sample that microscopy had determined to be positive for P. vivax, but both PCR primer sets determined it to be negative. There were also many samples using the LightCycler that could not be characterized as either positive or negative, so the real-time products were analyzed by gel electrophoresis to confirm the results found using the LightCycler. The bands on the gel were faint and some were barely visible. The characterization of these bands could have been either negative or positive, but in the end they were all characterized positive for P. vivax. The 100% specificity of the hemi-nested primer set was much higher than the 67% reported by Rubio et al. (1999), while the 93% specificity of the real-time primers was lower than the 99.1% reported by Mangold et al. (2005.) Further investigation is 34 Kimberly Leyster required to determine why my results differ from those reported by Mangold et al. (2005) and Rubio et al. (1999). A few of the samples (Figure 4 lane 2, 5, 6, 7, 11, 15, 16, 24, 32) showed two or more bands, with the brightest and most defined characterizing P. vivax. The nonspecific binding of the primers is caused by secondary structures (when DNA folds onto itself) because the fragments get stuck in the gel matrix and move slower and the rest of the DNA. Previous sequencing of these products was done and all of them were positive for P. vivax (M. Quintana, personal communication, Apr. 2007). To reduce nonspecific binding, I could have reduced the number of cycles in my PCR reactions, but this would also lower the sensitivity so I did not alter my protocol. To decide whether the sensitivity and specificity are acceptable, there are a few different levels of acceptance that can be used. If physicians were making the judgment on what was suitable, it is usually agreed that a >90 % certainty would be acceptable (M. Quintana, personal communication, Apr. 2007). On the other hand, a laboratory technician would not less than 95 % accuracy. Other factor that must be considered when deciding if the sensitivity and specificity calculated for each primer set is acceptable are the pathogen and methods used. A formula has been devised to determine the acceptance rate depending on the pathogen and methods used, but for the sake of this lab I am using the physician’s certainty of >90 % (M. Quintana, personal communication, Apr. 2007). Since both primer sets had sensitivities below 90 %, they are not acceptable in determining true positives. The specificity of both primers was above 90 % so they both are acceptable in detecting true negatives. 35 Kimberly Leyster When diagnosing patients, it is better to have error in sensitivity than in specificity, meaning a false negative is better than a false positive. The reason is because, depending on the disease, a false positive diagnosis could mean receiving harsh medications. On the contrary, a false negative diagnosis could later be re-evaluated when the patient continued to have symptoms and would likely be accurately diagnosed. Of course, 100% sensitivity and 100% specificity would be ideal, but if errors occur, it is best to err on the side of sensitivity. My results of 100% specificity with the hemi-nested primer set and 93% specificity with my real-time primers show both these primer sets to have high specificity. Most often, traditional PCR is better at detecting malaria than microscopy and the percentage I got for the specificity of my primer sets are higher than the average microscopist uses (M. Quintana, personal communication, Apr. 2007). Although I was not able to determine that one primer set was superior to the others, I did find a combination of two primer sets were able to correctly identify 96% of the samples. If I had time to continue this experiment, I would run a third set of primer pairs to test the samples that were not clearly positive or negative and see if there is a trend. It would also be useful to test the ability these primer sets to detect other species of Plasmodium. As reported in previous research (Rubio et al., 1999; Mangold et al., 2005; Perandin et al., 2004), many people are diagnosed with more than one species of Plasmodium, and the ability of a primer set to detect all species would be valuable. In areas were malaria is endemic, insecticides, bed nets and antimalarial drugs are effective devices in fighting malaria (Center for Disease Control and Prevention, 2005). But with resistance to the drugs increasing, a quicker diagnosis is becoming more 36 Kimberly Leyster important. By diagnosing the disease quickly, not only can treatment begin earlier, but the spread of the disease in the community may be reduced. Since microscopy depends greatly on the quality of the reagents, the microscope used, and the ability of the technician, more accurate diagnostic techniques are needed. The polymerase chain reaction has the potential to be a better diagnostic tool than microscopy, but the cost of the procedure and the reliability of current primer sets have prevented it from becoming the new “gold standard” (Center for Disease Control and Prevention, 2005). With continued testing of different primer sets, one day PCR could serve as the primary mechanism to more rapidly and accurately diagnose malaria. Acknowledgements I would like to take this opportunity to express my gratitude to the Fort Lewis Center for Health Promotion and Preventive Medicine-West (CHPPM-W) for their financial support and the use of their lab. I would also like to especially thank Miguel Quintana and Naomi Iihoshi who gave continual support and guidance throughout my project. In addition, I would like to express appreciation to Dr. Margaret Olney and Dr. Mary Jo Hartman for their direction and assistance. Finally, I want to thank Kevin Warren, Aaron Warren, and Dennis Hidalgo who graciously read and corrected my papers and gave constant support and advice throughout my project. 37 Kimberly Leyster Literature Cited Applied Biosystems. Real-time PCR vs. traditional PCR. <http://www.appliedbiosystems.com/support/tutorials/pdf/rtpcr_vs_tradpcr.pdf>. [accessed 2006 November 15] Bowen, R. Agarose Gel Electrophoresis. 15 January 2000. <http://www.vivo.colostate.edu/hbooks/genetics/biotech/gels/agardna.html>. [accessed 2006 October 15] Brock, T.D. Life at High Temperatures. 1994. <http://www.bact.wisc.edu/Bact303/b27>. [accessed 2006 October 14] Brown, J.C. What the heck is PCR? 1995. <http://www.hepatitis-c.de/pcr.htm>. [accessed 2006 October 13] Center for Disease Control and Prevention. Malaria. 12 September 2005. <http://www.cdc.gov/malaria/diagnosis_treatment/diagnosis.htm>. [accessed 2006 October 16] Davidson College: Department of Biology. Nested Primers for PCR. 2002. <http://www.bio.davidson.edu/courses/genomics/method/NestedPCR.html>. [accessed 2006 November 26] Dolan DNA Learning Center. < http://www.dnalc.org/ddnalc/resources/electrophoresis.html>. [accessed 2006 October 14] GeneCRC. 15 June 2004. < http://www.genecrc.org/site/lc/fp6c.pdf>. [accessed 2006 October 15] Henegariu, O. Choosing/designing PCR primers. March 2000. <http://info.med.yale.edu/genetics/ward/tavi/p02.html>. [accessed 2006 October 14] IPGRI and Cornell University. Using molecular marker technology in studies on plant genetic diversity. 2003. <http://www.igd.cornell.edu/MolecularMarkers/PCR%20basics.pdf>. [accessed 2006 October 14] Lairmore, T. C. Method: polymerase chain reaction. 9 May 1990. <http://hg.wustl.edu/hdk_lab_manual/pcr/pcr1.html>. [accessed 2006 October 14] Mangold, K. A., Manson, R. U., Koay, E. S., Stephens, L., Regner, M., Thomson Jr., R. B., Peterson, L., R., Kaul, K. L. May 2005. Real-Time PCR for Detection and Identification of Plasmodium spp. J Clinical Microbiology. 2435-2440. NOVA: Science in the News. Glossary-Malaria, a growing threat. June 1997. <http://www.science.org.au/nova/011/011glo.htm>. [accessed 2006 November 26] Perandin, F., Manca, N., Calderaro, A., Piccolo, G., Galati, L., Ricci, L., Medici, M.C., Arcangeletti, M.C., Snounou, G., Dettori, G., Chezzi, C. Development of a realtime PCR assay for detection of Plasmodium falciparum, Plasmodium vivax, and Plasmodium ovale for routine clinical diagnosis. < http://www.ajtmh.org/cgi/reprint/73/5/850>. [accessed 2006 November 3] Rabinow, P. What is PCR? 1998. <http://sunsite.berkeley.edu/PCR/whatisPCR.html>. [accessed 2006 October 13] 38 Kimberly Leyster Roche Diagnostics. The steps of PCR. 2006. <http://us.labsystems.roche.com/products/pcr/steps.shtml>. [accessed 2006 October 13] Rybicki, E. PCR primer design and reaction optimization. 2001. <http://www.mcb.uct.ac.za/pcroptim.htm#Annealing>. [accessed 2006 October 13] Shariff, M., Soon, S., Lee, K.L., Tan, L.T. Practical problems with PCR detection in Asia: the importance of standardization. <http://www.fao.org/DOCREP/005/X4946E/x4946e0d.htm>. [accessed 2006 October 13] Sumanas, Inc. The polymerase chain reaction (PCR). <http://www.sumanasinc.com/webcontent/anisamples/molecularbiology/pcr.html >. [accessed 2006 October 14] Swan, H., Sloan, L., Muyombwe, A., Chavalitshewinkoon-Petmitr, P., Krudsood, S., Leowattana, W., Wilairatana, P., Sooareesuwan, S., Rosenblatt, J. Evaluation of a real-time polymerase chain reaction assay for the diagnosis of malaria in patients from Thailand. < http://www.ajtmh.org/cgi/reprint/73/5/850>. [accessed 2006 October 4] Vierstraete, A. Principle of the PCR. 11 August 1999. <http://users.ugent.be/~avierstr/principles/pcr.html>. [accessed 2006 October 13] World Health Organization. Malaria. 9 October 2006. < http://wwwmicro.msb.le.ac.uk/224/Malaria.html>. [accessed 2006 November 5] 39