Guidance - The Scottish Government
advertisement

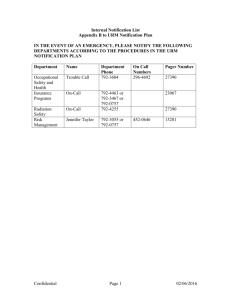
PAPER NSG 16 THE PUBLIC HEALTH ETC. (SCOTLAND) ACT 2008 Draft 1: Guidance to health boards, registered medical practitioners and diagnostic laboratories 1. Whilst the electronic issues concerning notification have yet to be fully addressed, I thought that it would be useful to draw together the work undertaken by the group to date, so that it can be considered within an overall framework. The following documents (which I have attached to this for ease of reference) comprise: - - A covering guidance note to Health Boards (both to ensure that they comply with their statutory notification duties, but also to issue the other guidance to registered medical practitioners and diagnostic laboratories in their areas); Paper 1 – guidance to registered medical practitioners; Paper 2 – guidance to health boards; Paper 3 – guidance to diagnostic laboratories. 2. You will wish to consider how I have incorporated the guidance to date on HRSs, nurse-led clinics, ‘urgent’ notifications, case definitions and other general information, including governance and offences. I have tried to be as brief as possible. Lorna is currently considering further advice relating to organisms to try to ensure consistency of notification timescales (within the statutory deadline), and she’ll be able to speak about that at the meeting. 3. In the meantime, it would be useful to have your views on what has been developed, particularly on clarity, bearing in mind that this is still very much work in progress. I think that it also re-inforces the need for the group to consider the communication needs around the implementation of Part 2 of the Act. Molly Robertson Public Health Act Implementation Team March 2009 Part 2 General HB guidance – Draft 1 – March 2009 PUBLIC HEALTH ETC. (SCOTLAND) ACT 2008 IMPLEMENTATION OF PART 2: NOTIFIABLE DISEASES, ORGANISMS AND HEALTH RISK STATES Purpose 1. This paper advises that Part 2 and Schedule 1 of the Public Health etc. (Scotland) Act 2008 comes into effect on [1 January 2010] and provides supporting guidance to health boards, registered medical practitioners and directors of diagnostic laboratories on their obligations under the Act with regard to the notification of infectious diseases, organisms and health risk states. Current responsibilities under the Public Health (Notification of Infectious Diseases) (Scotland) Regulations 1988 and the Infectious Disease (Notification) Act 1889 cease to apply on [31 December 2009]. 2. Part 2 and Schedule 1 of the Act are replicated in Annex A. Guidance 3. Guidance is contained in the following papers, attached: Paper 1: Notifiable diseases and health risk states: duties on registered medical practitioners Paper 2: boards Notifiable diseases and health risk states: duties on health Paper 3: Notifiable organisms: duties on directors of diagnostic laboratories 4. Health boards should ensure that they meet their new statutory obligations on 1 January 2010 (Paper 2). They are also invited to note the guidance to registered medical practitioners (Paper 1) and diagnostic laboratories (Paper 3) in their areas which have implications for the work within the boards’ health protection teams. 5. In addition, health boards are requested to issue the relevant advice to registered medical practitioners and laboratories in their areas to ensure a smooth transition to the new arrangements. The guidance would also be useful to those registered nurses leading clinics or out of hours services or working in isolated communities without immediate access to a registered medical practitioner. The guidance should be augmented, before issue, by the provision of local Health Protection Team contact details for notifications, where appropriate, including urgent notifications and for inquiries. Methods of notification [ISSUES AROUND THE ELECTRONIC TRANSMISSION ARRANGEMENTS ETC] 2 Part 2 General HB guidance – Draft 1 – March 2009 6. Further detailed information on the Act is http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/publicact 3 available at Part 2 General HB guidance – Draft 1 – March 2009 ANNEX A [COPY OF PART 2 AND SCHEDULE 1 TO BE INSERTED] 4 Part 2 guidance – paper 1, draft 1 – March 2009 PAPER 1 PUBLIC HEALTH ETC . (SCOTLAND) ACT 2008 NOTIFIABLE DISEASES AND HEALTH RISK REGISTERED MEDICAL PRACTITIONERS STATES: DUTIES ON Diseases notifiable under the Public Health etc. (Scotland) Act 2008 from [1 January 2010] *Anthrax *Meningococcal disease *Severe Acute Respiratory Syndrome (SARS) *Botulism Mumps *Smallpox Brucellosis *Necrotizing fasciitis Tetanus *Cholera *Paratyphoid Tuberculosis (respiratory or non-respiratory *Clinical syndrome due to *Pertussis *Tularemia E.coli 0157 infection *Diphtheria *Plague *Typhoid *Haemolytic Uraemic *Poliomyelitis *Viral haemorrhagic fevers Syndrome (HUS) *Haemophilus influenzae *Rabies *West Nile fever Type b (Hib) *Measles Rubella Yellow Fever Case definitions can be accessed online at [ ]. Notification of health risk states As well as those diseases above which are notifiable in their own right, medical practitioners are obliged to notify any case suffering from a ‘health risk state’ (HRS), and anyone likely to have been exposed to such a case with an HRS, or the same risk factor. Further guidance is contained in Annex A. Please note that we would expect notification of a health risk state to be an exceptional occurrence. Further requirements and supporting guidance Notification is on grounds of reasonable suspicion that a patient whom the practitioner is attending has a notifiable disease/HRS. Practitioners must notify their health board, in writing (which includes electronic transmission) within 3 days of suspicion, unless he/she has reasonable grounds to believe that another practitioner has notified the disease/HRS. This does not include the potential notification by a laboratory of the organism which causes the disease. Separate notification arrangements are in place for diagnostic laboratories. For the purposes of electronic notification, a document is to be taken to be received on the day of transmission. If the case is ‘urgent’, notification should take place by telephone as soon as reasonably practicable. The need to notify urgently is determined by the registered medical practitioner, having regard to the nature of the disease, the 5 Part 2 guidance – paper 1, draft 1 – March 2009 ease of transmission of that disease, the patient’s circumstances and any guidance issued by Scottish Ministers. It is suggested that those diseases above marked with an * may require urgent notification, i.e. within same working day. However, there may be other circumstances where immediate notification might be necessary, e.g. if there are a cluster of cases. Further guidance on the need for telephone notification may be provided locally from time to time, based on changing epidemiology or particular local circumstances. It is recognised that there may be nurses leading clinics or out of hours services, or working in isolated communities who may well form a suspicion that a patient has a notifiable disease etc., which requires immediate action. If such a nurse were to communicate a suspicion by telephone to a registered medical practitioner, the practitioner may choose to commence notification procedures immediately on this basis. Should there be delay in contacting a registered medical practitioner to facilitate notification, for any reason, the registered nurse should call the local health protection team directly to inform them of their suspicion. However, this does not constitute a formal notification under the Act. The registered nurse should continue to pursue formal notification through the relevant registered medical practitioner. Information to be notified (in so far as it is known) the patient’s name; the patient’s address and postcode; the patient’s occupation (if the practitioner considers that it is relevant); the name, address and postcode of the patient’s place of work or education (if the practitioner considers that it is relevant); the patient’s sex; the patient’s date of birth; the suspected disease; and the patient’s NHS identifier, i.e. the patient’s community health index number or where that number is not known, the NHS identification number, or where neither of these numbers are known, any other number of other indicator which is used to identify a patient individually. Method of notification [GUIDANCE ON ELECTRONIC REPORTING ARRANGEMENTS, INCLUDING FORM] Local contacts The Act requires notification to the Health Board for the area in which the practitioner works. For [ [ ] NHS Board, the contacts are: ] 6 Part 2 guidance – paper 1, draft 1 – March 2009 Further information The list of diseases has been considerably reduced from existing statutory notification requirements and only contains diseases which may prompt urgent public health action. For example, food poisoning and chickenpox, which constitute about 80% of current notifications, have been removed. The fee to registered medical practitioners has been removed, recognising that notification of the significant diseases on the list will become an unusual event for a medical practitioner and should be undertaken under his/her general duty of care to protect public health. Non-notification is a governance issue which falls to the health board for employed doctors, and for GPs as independent contractors, through their own clinical governance systems, and ultimately through the GMS contractual requirement in paragraph 114 of the GMS regulations, i.e. the contractor shall comply with all relevant legislation; and have regard to all relevant guidance issued by the health board and the Scottish Ministers. Scottish Ministers may amend the list set out above, by regulation, by adding to or removing an item from the list, and varying the description of an item in the list. Scottish Ministers may also, by regulation, amend any other aspect of the notification arrangements. Further detailed information on the Act is http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/publicact 7 available at Part 2 guidance – paper 1, draft 1 – March 2009 Annex A NOTIFICATION OF HEALTH RISK STATES Why is it necessary to notify suspected 'health risk states'? The aim of notifying suspected health risk states is to identify diseases or conditions which are not notifiable in their own right but which pose or may pose a significant risk to public health. Pubic health authorities need to be able to identify and respond quickly to new and emerging public health threats, even when a condition is identified from its symptoms and epidemiology and the causative organism is not yet identified. This is particularly relevant in the modern world of global travel and trade. For example, urgent public health action was required in the early stages of the SARS (Severe Acute Respiratory Syndrome) outbreak in 2003, even before the causative agent was known. Other examples from the past of conditions that would fulfil the criteria of a health risk state include the initial five cases of Pneumocystits carinii pneumonia heralding the AIDS epidemic, avian flu, Polonium exposure and poisoning in the Litvinenko case. What should be notified? If a novel serious condition occurs at home or abroad, it may be designated an HRS by the Scottish Government's Chief Medical Officer (CMO), who will provide a case definition for exactly what should be notified. In the absence of a definition from the CMO, medical practitioners should notify as an HRS any condition which is: 1. Serious: A case must be very ill or have died, or be likely to become very ill or die. AND 2. Be potentially serious to others. The three principal ways in which a HRS might be serious for others are if it is: (i) infectious; (ii) the result of contamination with, for example, a radioactive material; (iii) the result of a toxin or poison to which others may be exposed. An HRS is likely to be new, rare, unexplained, or difficult to diagnose. Obviously, the more serious the condition, and the greater the likelihood of spread, the more important it is for the medical practitioner to notify it. The more cases the medical practitioner sees within a given period of time, the more likely is the potential for spread, but an HRS presenting in a single case may still have the potential to affect others. 8 Part 2 guidance – paper 1, draft 1 – March 2009 Notifications of a ‘health risk state’ will be an exceptional occurrence and should only be made on the basis that the registered medical practitioner considers that there is a risk of significant public health implications of the condition. If in doubt whether to notify a condition, on grounds of either its seriousness or potential to affect others, the medical practitioner should discuss the condition with their CPHM (CD&EH). How to notify Immediate oral notification by telephone would be expected in these circumstances, followed up in writing with the required information within 3 days of forming the suspicion of the health risk state. 9 Part 2 guidance – paper 2, draft 1 – March 2009 PAPER 2 PUBLIC HEALTH ETC. (SCOTLAND) ACT 2008 NOTIFIABLE DISEASES AND HEALTH RISK STATES: DUTIES ON HEALTH BOARDS Requirements and supporting guidance Where a health board receives a notification of a disease or health risk state from a registered medical practitioner and the patient to whom the information relates usually resides in that health board area, the board must send a return, in writing (which includes electronic transmission), to Health Protection Scotland (HPS), containing the information set out below. The return should be sent by the end of the working week in which the information is received (i.e. by close of play on Friday of that week), or, if it is not practicable to do so, as soon as practicable afterwards. For the purposes of electronic transmission of data, a document is to be taken to be received on the day of transmission. If the patient to whom the information relates does not usually reside in that health board area, the board must without delay transmit the information to the health board for the area in which the person usually resides. Where a health board receives information from another health board about a patient who usually resides in its area, that board must send the return, in writing, to HPS, by the end of the working week in which it is received (i.e. by close of play on Friday of that week) or, if it is not practicable to do so, as soon as practicable afterwards. Information to be included in return to HPS (in so far as it is known) the patient’s postcode; the patient’s occupation; the patient’s sex; the patient’s date if birth; the suspected disease or suspected health risk state; and the patient’s NHS identifier, i.e. the patient’s community health index number or where that number is not known, the NHS identification number, or where neither of these numbers are known, any other number or other indicator which is used to identify a patient individually. Method of notification [[GUIDANCE ON ELECTRONIC REPORTING ARRANGEMENTS ETC] 10 Part 2 guidance – paper 3, draft 1 – March 2009 PAPER 3 PUBLIC HEALTH ETC. (SCOTLAND) ACT 2008 NOTIFIABLE ORGANISMS: DUTIES ON DIRECTORS LABORATORIES OF DIAGNOSTIC The Public Health etc. (Scotland) Act 2008 places a new statutory obligation on directors of diagnostic laboratories in Scotland to notify the organisms set out in Annex A, with effect from [1 January 2010]. Requirements and supporting guidance The director of a diagnostic laboratory in Scotland must notify the organisms set out in Annex A to the health board in whose area the laboratory is situated and Health Protection Scotland (HPS). Notification must take place, in writing (which includes electronic transmission), within 10 days of identification. For the purposes of electronic notification, a document is to be taken to be received on the day of transmission. If the case is ‘urgent’, notification should take place by telephone as soon as reasonably practicable. ‘Urgency’ is determined by the director of the laboratory, having regard to the nature of the organism, the nature of the disease caused by the organism, the ease of transmission, the patient’s circumstances (where known) and any guidance issued by Scottish Ministers. It is suggested that those organisms marked with an * merit notification as a matter of urgency. However, there may be circumstances where notification well within the 10 day period would be appropriate, but might not necessarily merit immediate telephone notification, or where organisms might need to be notified to health boards before formal identification. Laboratories should therefore ensure that they have mutually agreed Standard Operating Procedures or other agreements in place with local health boardS, which clarify these issues and take into account their new statutory obligations. Where a diagnostic laboratory requires, under an arrangement, to send a sample to another laboratory for analysis, e.g. to a specialist facility in Scotland or elsewhere in the UK), statutory notification is required from the originating laboratory. In these cases, the day of identification for the purposes of notification will be the day on which the first diagnostic laboratory becomes aware of the identification by the other laboratory with which it has the arrangement. Information to be notified (in so far as it is known) the name of the person to whom the identification relates; the person’s address; the person’s sex; the person’s date of birth; the organism which has been identified; and 11 Part 2 guidance – paper 3, draft 1 – March 2009 the person’s NHS identifier, i.e. the patient’s community health index number or where that number is not known, the NHS identification number, or where neither of these numbers are known, any other number or other indicator which is used to identify a patient individually. Method of notification [CURRENT ELECTRONIC NOTIFICATION ARRANGEMENTS/ VIA ECOSS etc] Local contacts [ ] Further information ‘Diagnostic laboratory’ means an institution (or facility within an institution) which is equipped with apparatus and reagents for the performance of diagnostic tests for human infections. ‘Director of a diagnostic laboratory means – - the clinical microbiologist, consultant pathologist or other registered medical practitioner or other person in charge of a diagnostic laboratory; or - any other person working in the diagnostic laboratory to whom the function of making a notification under this section has been delegated by the person mentioned above. Scottish Ministers may amend the list of organisms to be notified, by regulation, by adding to or removing an item from the list, and varying the description of an item on the list. Scottish Ministers may also, by regulation, amend any aspect of the notification arrangements. Offences It is an offence for the director of a diagnostic laboratory to fail, without reasonable excuse, to comply with the duty of notification. Where the director of a diagnostic laboratory commits an offence and is employed by a body corporate, the body corporate also commits the offence. There is a defence of due diligence and that all reasonable steps were taken to avoid committing the offence, both for a director of the diagnostic laboratory and a body corporate, or its employee or agent. Further detailed information on the Act is http://www.scotland.gov.uk/Topics/Health/NHS-Scotland/publicact 12 available at NOTIFIABLE ORGANISMS ANNEX A *Bacillus anthracis Bacillus cereus *Bordetella pertussis Borrelia burgdorferi Brucella genus *Campylobacter genus Chlamydia psittaci *Clostridium botulinum Clostridium difficile Clostridium perfringens *Clostridium tetani *Corynebacterium diphtheriae (toxigenic strains) *Corynebacterium ulcerans *Coxiella burnetii *Crimean-Congo haemorrhagic fever virus *Cryptosporidium Dengue virus *Ebola virus Echinococcus genus *Verocytotoxin-producing E.coli (VTEC) *Francisella tularensis *Giardia lamblia *Guanarito virus *Haemophilus influenzae type b (from blood, cerebrospinal fluid or other normally sterile site) Hantavirus *Hepatitis A virus *Hepatitis B virus Hepatitis C virus Hepatitis E virus Influenza virus (all types, including *those caused by a new sub-type) 13 *Junín virus *Kyasanur Forest disease virus *Lassa virus *Legionella genus Leptospira genus *Listeria monocytogenes *Machupo virus *Marburg virus *Measles virus Mumps virus *Mycobacterium bovis *Mycobacterium tuberculosis complex *Neisseria meningitidis Norovirus *Omsk haemorrhagic fever virus Plasmodium falciparum, vivax, ovale and malariae *Polio virus *Rabies virus Rickettsia prowazekii *Rift Valley fever virus *Rubella virus *Sabia virus *Salmonella (all human types) *SARS-associated coronavirus *Shigella genus Enterotoxigenic Staphylococcus aureus Staphylococcus aureus (all blood isolates) Methicillin-resistant Staphylococcus aureus (MRSA) *Streptococcus pyogenes (from blood, cerebrospinal fluid or other normally sterile site) Streptococcus pneumoniae (from blood, cerebrospinal fluid or other normally sterile site) Toxoplasma gondii 14 Trichinella genus Varicella-zoster virus *Variola virus *Vibrio cholerae *West Nile fever virus *Yellow Fever virus *Yersinia enterocolitica *Yersinia pestis *Yersinia pseudotuberculosis Case definitions can be accessed online at [ 15 ]