treatment protocols oct 13
advertisement
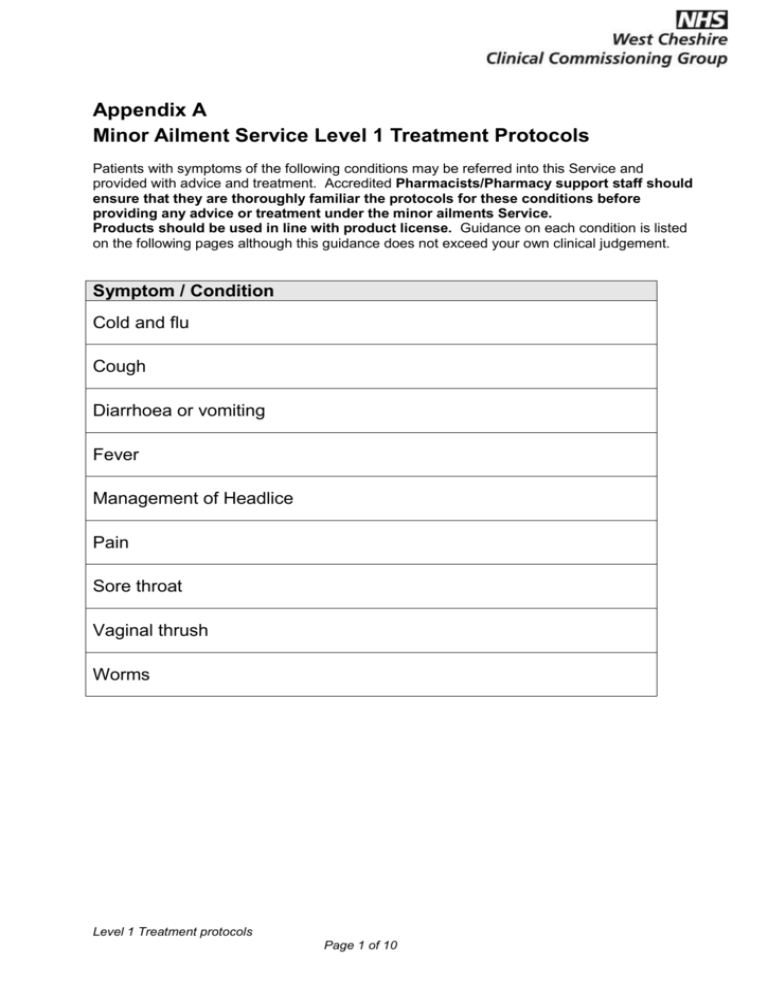
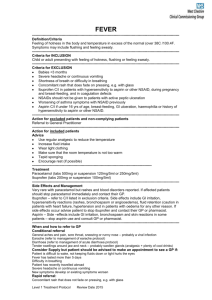
Appendix A Minor Ailment Service Level 1 Treatment Protocols Patients with symptoms of the following conditions may be referred into this Service and provided with advice and treatment. Accredited Pharmacists/Pharmacy support staff should ensure that they are thoroughly familiar the protocols for these conditions before providing any advice or treatment under the minor ailments Service. Products should be used in line with product license. Guidance on each condition is listed on the following pages although this guidance does not exceed your own clinical judgement. Symptom / Condition Cold and flu Cough Diarrhoea or vomiting Fever Management of Headlice Pain Sore throat Vaginal thrush Worms Level 1 Treatment protocols Page 1 of 10 COLD AND FLU --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Nasal congestion, sneezing, mild temperature, sore throat, general aches and pains are associated with the common cold. Refer to other relevant protocols as appropriate. --------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Children or adults presenting with cold or flu-like symptoms --------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Patients under one year Concomitant rash that does not fade under pressing e.g. with glass Patient is breathless Light hurts the eyes It is painful to bend the neck Systemic decongestants (pseudoephedrine) should be avoided in patients taking MAOI inhibitors and used with caution in patients with diabetes, hypertension, hyperthyroidism and ischaemic heart disease --------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner --------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Simple analgesics to bring temperature down Steam inhalation (with or without aromatic inhalant) Maintain a good fluid intake Encourage rest (if possible) Warm soothing drinks Common cold does not require antibiotics for effective treatment Remind high risk patients of influenza vaccination programmes (over 65s, and those patients under 65 with CHD, respiratory disease or diabetes) No improvement in symptoms after three days, consult GP -----------------------------------------------------------------------------------------------------------Treatment Paracetamol (tabs 500mg or suspension 120mg/5ml or 250mg/5ml) --------------------------------------------------------------------------------------------------------------------------------Side Effects and Management Very rare with paracetamol but rashes and blood disorders reported. If affected patient should stop paracetamol immediately and contact their GP. --------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral Patients with other chronic illness e.g. heart, kidney or lung disease, those with reduced immunity or patients living in long-stay institutions. These patients would benefit from influenza vaccination. Consider Supply but patient should be advised to make an appointment to see a GP if: New symptoms develop particularly in young children, the elderly or the infirm Symptoms worsening Patient becoming breathless Painful to bend the neck or light hurts the eyes Rapid referral: Development of a rash that does not fade when you press a glass tumbler against the rash Level 1 Treatment protocols Page 2 of 10 COUGH --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Coughing arises as a defensive reflex mechanism --------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Troublesome cough requiring soothing --------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Patients under one year Cough of more than three weeks’ duration Cough productive of blood-stained sputum Asthmatics presenting with wheeze or reduced peak-flow Family history of asthma Difficulty breathing or shortness of breath --------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner --------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice only to be given, no medication. Smoking status to be checked and advice given regarding cessation if appropriate. --------------------------------------------------------------------------------------------------------------------------------Recommended Treatments, Route and Legal status. Frequency of administration and maximum dosage N/A --------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral: If cough and other symptoms persist beyond one week the patient should consult the GP; Rapid referral: Constant chest pain or chest pain on normal inspiration Difficulty breathing Green or rusty sputum If pain related to exertion Level 1 Treatment protocols Page 3 of 10 DIARRHOEA & VOMITING --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Diarrhoea Increased frequency and fluidity of defecation Vomiting Forcible ejection of contents of stomach ---------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Patients experiencing the above symptoms ---------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Children under the age of 1 year Pregnant women Patients with chronic diarrhoea problems Vomiting not improving after 1 day Diarrhoea not improving after 5 days, especially following return from tropical or developing country. ---------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner ---------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Patient should have adequate fluid replacement for 24 – 48 hours until the symptom resolves Fast for 24hours with clear fluids only Sip fluids Light diet for first few days Diarrhoea not improving after 5 days, especially following return from tropical or developing country. These patients will be advised to collect a specimen bottle from the surgery for stool culture and to make an appointment to see the doctor when the results are available. ------------------------------------------------------------------------------------------------------Treatment Loperamide caps x 12 Dioralyte sachets x 6 Criteria Loperamide for adults and children over 12 years ---------------------------------------------------------------------------------------------------------------------------------Side effects and their management Loperamide can cause abdominal pain and bloating ---------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral If symptoms persist beyond 48 hours, consult the GP Consider Supply but patient should be advised to make an appointment to see a GP if: Patients taking medication with recognised diarrhoea effect Rapid referral: Adults, where symptoms have lasted more than 5 days Children, where symptoms have lasted more than 48 hours or who look ill or dehydrated Pregnancy Level 1 Treatment protocols Page 4 of 10 FEVER -----------------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Feeling of hotness in the body and temperature in excess of the normal (over 38C /100.4F. Symptoms may include flushing and feeling sweaty. ---------------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Child or adult presenting with feeling of hotness, flushing or feeling sweaty. ---------------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Babies <3 months Severe headache or continuous vomiting Shortness of breath or difficulty in breathing Concomitant rash that does fade on pressing, e.g. with glass Ibuprofen C/I in patients with hypersensitivity to aspirin or other NSAID, during pregnancy and breast-feeding, and in coagulation defects NSAIDs should not be given to patients with active peptic ulceration Worsening of asthma symptoms with NSAID previously Aspirin C/I if under 16 yrs of age, breast-feeding, GI ulceration, haemophilia or history of hypersensitivity to aspirin or other NSAID. ---------------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner ---------------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Use regular analgesic to reduce the temperature Increase fluid intake Wear light clothing Make sure that the room temperature is not too warm Tepid sponging Encourage rest (if possible) ----------------------------------------------------------------------------------------------------Treatment Paracetamol (tabs 500mg or suspension 120mg/5ml or 250mg/5ml) Ibuprofen (tabs 200mg or suspension 100mg/5ml) -----------------------------------------------------------------------------------------------------------------------------------------Side Effects and Management Very rare with paracetamol but rashes and blood disorders reported. If affected patients should stop paracetamol immediately and contact their GP. Ibuprofen – refer to C/I listed in exclusion criteria. Side effects include GI irritation, hypersensitivity reactions (rashes, bronchospasm or angiooedema), fluid retention (caution in patients with heart failure, hypertension and in patients with oedema for any other reason. If side effects occur advise patient to stop ibuprofen and contact their GP or pharmacist. Aspirin – Side –effects include GI irritation, bronchospasm and skin reactions in some patients – stop aspirin use and consult GP or pharmacist. ---------------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral General aches and pain, sore throat, sneezing or runny nose – probably a viral infection Earache (refer to management of earache protocol) Diarrhoea (refer to management of acute diarrhoea protocol) Tender swellings around jaw and neck – probably swollen glands (analgesic + plenty of cool drinks) Consider Supply but patient should be advised to make an appointment to see a GP if: Patient is difficult to wake, not keeping fluids down or light hurts the eyes Fever has lasted more than 5 days Difficulty in breathing Patient has recently travelled abroad Severe headache or continuous vomiting New symptoms develop or existing symptoms worsen Rapid referral: Concomitant rash that does not fade on pressing, e.g. with glass Level 1 Treatment protocols Page 5 of 10 MANAGEMENT OF HEADLICE --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria An infection by the head louse (Pediculus humanus capitis). A person must have a living, moving louse to be infected. Head lice can only be transmitted by direct, prolonged, head to head contact between individuals. Nits are the empty egg cases that stick to hair and do not indicate a current infection. --------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Children or adults presenting with evidence of a living, moving louse seen on the scalp (most reliable method is detection combing). Children under 1 yr can be treated at the pharmacist’s discretion (medical supervision for children under 6 months). All family members should be checked for head lice. Only those found to have a live, moving louse should be considered for treatment --------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Family/siblings of patient, who are not proven to be infested (note: infestation is not indicated by the presence of nits [hatched and empty egg shells]) Children under the age of six months --------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner --------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Broad comb, then wet comb well conditioned hair to remove dead lice and eggs Regular detection combing as treatment will not prevent re-infection from classmates Remove all adult lice before return to school Continue combing for two weeks Check all members of family (including grandparents etc. if contact) If live lice still present, consult health visitor or pharmacist to check technique Hair should be allowed to dry naturally – avoid flames. Do not use hair dryers Check pillow and collars for little black specks (lice droppings) and shed lice skins Encourage patient or parent to contact close relatives and friends to ensure detection and treatment of further confirmed cases. -----------------------------------------------------------------------------------------------------------Treatment Wet Combing - an alternative to chemical application using a ‘Bug-busting kit’ Requires mechanical removal of head lice by meticulous combing with a detection comb (for at least 30 minutes at a time) over the whole scalp, at four days intervals, for a minimum of two weeks. Use any conditioner. --------------------------------------------------------------------------------------------------------------------------------Side effects and their management Side effects are experienced rarely --------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Refer to GP if combing has failed and further treatment with liquid head lice lotions is required to halt infestation. Level 1 Treatment protocols Page 6 of 10 PAIN --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Pain is a subjective experience, the nature and location of which may vary considerably. ---------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Patients requiring relief or pain / fever associated with upper respiratory tract infections and dental problems ---------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Children under the age of 3 months Recurrent or severe pain ---------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner --------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Enquire about concurrent analgesic usage Paracetamol daily dose – other products containing Paracetamol Other NSAIDs – prescribed or OTC Rest, warming, cooling or changing position, may obtain relief from pain. Patients should be advised to avoid any aggravating factors Pharmacists should be aware of the National Institute for Clinical Excellence guidance on Feverish Children and can advise on alternating ibuprofen with paracetamol if neither work individually NB. Overuse of analgesics can cause headaches -----------------------------------------------------------------------------------------------------------Treatment Paracetamol (tabs 500mg or suspension 120mg/5ml or 250mg/5ml) Ibuprofen (tabs 200mg or suspension 100mg/5ml) ---------------------------------------------------------------------------------------------------------------------------------Side Effects and Management Side effects are rare with occasional use of Paracetamol Ibuprofen should be taken after food to avoid GI side effects. --------------------------------------------------------------------------------------------------------------------------------- Level 1 Treatment protocols Page 7 of 10 SORE THROAT -------------------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Painful, inflamed throat which makes swallowing difficult. Most sore throats are caused by viruses and symptoms can take 2-7 days to clear after they start -------------------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Children or adults presenting with symptoms of acute, uncomplicated sore throat. -------------------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Patients under one year Presence of tender lumps below the ear or at the jaw angle Severe difficulty in swallowing Five or more episodes of sore throat in the last 12 months causing serious disruption of daily life Suspicion of more serious disorder e.g. leukaemia, drug induced neutropenia Aspirin C/I if under 16 yrs of age, breast-feeding, GI ulceration, haemophilia or history of hypersensitivity to aspirin or other NSAID. Symptoms not improved after 5 days -------------------------------------------------------------------------------------------------------------------------------------------Action for excluded patients Referral to General Practitioner Can consider supply where the pharmacist considers this appropriate providing there is no delay in seeking further treatment (see below) -------------------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Maintain good fluid intake Eat soft foods or warm soup Encourage rest (if possible) Avoid a smoky environment - smoking status to be checked and advice given regarding cessation if appropriate. Regular pain relief Advise on natural course of sore throat i.e. can take several days for symptoms to subside PIL Patients >16 years gargle with soluble aspirin Patients <16 years analgesia -----------------------------------------------------------------------------------------------------------Treatment Soluble aspirin 300mg (over 16s only) Ibuprofen tabs 200mg tabs Ibuprofen suspension 100mg/5ml SF Paracetamol susp 120mg/5ml or 250mg/5ml -------------------------------------------------------------------------------------------------------------------------------------------Side Effects and Management Very rare with paracetamol but rashes and blood disorders reported. If affected patient should stop paracetamol immediately and contact their GP. Aspirin and ibuprofen – refer to C/I listed in exclusion criteria. Side effects include GI irritation, hypersensitivity reactions (rashes, bronchospasm or angioedema), fluid retention (caution in patients with heart failure, hypertension and in patients with oedema for any other reason. If side effects occur advise patient to stop aspirin or ibuprofen and to contact their GP or pharmacist. -------------------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral If symptoms persist more than one week If tonsils are dotted with white or yellowish spots – possible tonsillitis or pharyngitis – is the treatment any different? Medical advice. Patients on immunosuppressants, oral steroids, drugs causing bone marrow suppression Patient having reported five or more episodes of sore throat Swelling of neck glands – common with sore throats Consider Supply but patient should be advised to make an appointment to see a GP if: Prolonged throat soreness, difficulty in swallowing or voice hoarseness If new symptoms develop (could also contact pharmacist or NHS Direct) Rapid referral: Patient unable to swallow own saliva – call 999 or NHS Direct Level 1 Treatment protocols Page 8 of 10 VAGINAL THRUSH --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Vaginal candidiasis (Thrush) ---------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Occuring in adult females with a previous diagnosis of Thrush who are confident it is a recurrence of the same condition. ---------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Patients under 16 years Patients over 60 years Patients unsure if it is Thrush Recurrent (more than 2 episodes in 6 months) No previous diagnosis by GP Pregnancy ---------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Referral to General Practitioner ---------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Make aware sexual partners should be treated concurrently Advise if symptoms do not resolve within 7 days to make an appointment to see a GP Avoid irritants e.g. bath additives Make aware of problems with vaginal deodorants, scented soap etc. ---------------------------------------------------------------------------------------------------Treatment Clotrimazole pessary 500mg with clotrimazole cream if needed for external symptoms Fluconazole capsule 150mg ---------------------------------------------------------------------------------------------------------------------------------Side Effects and their Management Sensitivity to Imadazoles Drug Interactions Pharmacist should consider interactions, for example with anti-coagulants, some antihistamines, tranquillisers, statins etc. ---------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral On 3rd occurrence Consider Supply but patient should be advised to make an appointment to see a GP if: Post-menopausal women Rapid referral: Presence of loin pain Fever If blood present in discharge Level 1 Treatment protocols Page 9 of 10 WORMS --------------------------------------------------------------------------------------------------------------------------------Definition/Criteria Threadworm infection --------------------------------------------------------------------------------------------------------------------------------Criteria for INCLUSION Patients with intense perianal or perivaginal night time itching who can confirm a threadworm infection. ---------------------------------------------------------------------------------------------------------------------------------Criteria for EXCLUSION Patients under 2 years Pregnancy Breastfeeding Recent return from tropical/developing country ---------------------------------------------------------------------------------------------------------------------------------Action for excluded patients and non-complying patients Non-drug therapy (hygiene measures) ---------------------------------------------------------------------------------------------------------------------------------Action for included patients Advice Family members should be treated simultaneously For 14 days after treatment hygiene measures should be taken which include: o Wear underpants at night; o Have a bath or wash around the anus (back passage) each morning immediately on rising; o Change and wash underwear, nightwear and bed linen (if possible) each day; o Keep fingernails short; o Wash hands and scrub under the nails first thing every morning, after using the toilet or changing nappies, and before eating or preparing food; o Vaccum all carpets and clean bathroom surfaces daily; For Mebendazole – a second dose may be required after 2-3 weeks if re-infection occurs -----------------------------------------------------------------------------------------------------------Treatment Mebendazole tabs 100mg ---------------------------------------------------------------------------------------------------------------------------------Side Effects and their Management Side effects are rare but transient abdominal pain or diarrhoea may occur. Very occasionally there may be hypersensitivity reactions. ---------------------------------------------------------------------------------------------------------------------------------When and how to refer to GP Conditional referral Pregnant women and breastfeeding mothers who have failed to eradicate after 6 weeks of hygiene measures. Consider Supply but patient should be advised to make an appointment to see a GP if: If there is a risk of a secondary infection due to intense scratching of the perianal skin In persistent or heavy cases of infection where patient has suffered loss of appetite, weight loss, insomnia and irritability If recently returned from tropical/developing country Level 1 Treatment protocols Page 10 of 10