ASTHMA POLICY - St Matthew`s C of E Primary School
advertisement

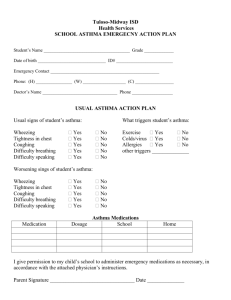
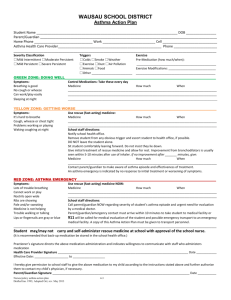
St. Mathew’s CE Primary School Asthma Policy Introduction Asthma is potentially a life threatening condition which demands to be taken seriously. Asthma can affect up to one in five children and any class may have up to 5 children with the condition. Therefore, it is important for teachers and allied staff to be aware of asthma, its symptoms, triggers and management in a school environment. Whilst at school, a child with asthma has the right to expect 1) Appropriate support to fully participate in school activities including physical education 2) An environment as free of asthma triggers as possible 3) Help in catching up with lessons after time away from school 4) Access to their usual medicaments as per their asthma management plan 5) Immediate access to their life saving reliever medication should this be necessary. Asthma symptoms include 1) 2) 3) 4) 5) Wheezy breathing (a whistling noise from the chest) Cough (usually not producing sputum) Difficulty in breathing/shortness of breath Tightness in the chest Difficulty in speaking due to shortness of breath Asthma triggers include 1) 2) 3) 4) 5) Pollens Dust/house dust mite Cigarette smoke Respiratory tract infections Exercise Asthma medication There are two main groups of medications used in the treatment of asthma 1) Relievers such as Salbutamol (Ventolin) 2) Stabilisers such as Beclomethasone (Becotide) Both of these groups have delivery systems which are usually a variety of inhaler with or without a spacer device to aid usage. Relievers work within a few minutes of their usage and the effect usually lasts for 4-6 hours. Stabilisers are normally slower in action and are given twice daily such that they are usually used prior to and after school hours. As well as an emergency supply of reliever medication, the school will hold, in safe keeping, an individual child’s medication which is suitably labelled and used as per that particular child’s asthma management plan. Emergency use equipment such as spacers, puffers etc. will be cleaned by soaking in Milton solution or equivalent after use for 20 minutes and then allowed to “air” dry. Asthma management plan Every child with asthma attending school should have a written asthma management plan filled out by an appropriate person (parent, family doctor, paediatrician etc.) which will be attached to the child’s school record. The plan will include 1) 2) 3) 4) 5) Usual medical treatment (i.e that which is taken when child is well) How to recognise worsening symptoms. An action plan detailing medications used if the asthma should worsen. Name, address and telephone number of an emergency contact Name, address and telephone number of child’s general practitioner Supplementary first aid supplies The school’s essential equipment for managing an asthma attack must include 1) A reliever medication in the form of a metered dose inhaler (e.g. Salbutamol) 2) A large volume spacer (volumatic/aerochamber etc.) to assist with the effective use of the reliever medication 3) Clear written instructions on how to use the inhaler and spacer. Schools can legally obtain the reliever and spacer for emergency use from a pharmacist on written authority of the Headteacher. A staff member should be delegated the responsibility of regularly checking this equipment and the expiry date of the inhaler. Stages of asthma An asthma attack may be mild, moderate or severe 1) Mild – this involves coughing, a soft wheeze, minor difficulty in breathing and no difficulty speaking sentences 2) Moderate – this involves persistent coughing, loud wheeze, obvious difficulty in breathing and an ability to speak in short sentences only 3) Severe – The child is often distressed or anxious, gasping for breath, unable to speak more than a few words, pale, sweaty and may have blue lips How to manage an asthma attack/ a child’s deteriorating condition 1) Ensure that the reliever inhaler is taken immediately. Whenever possible allow the medication to be taken where the attack occurs. 2) If the child’s own inhaler is not accessible, use the school emergency devices. Up to 10 puffs may be used in the spacer at one time. 3) Stay calm and reassure the child. Stay with the child until the attack is resolved. 4) Help the child to breathe by encouraging them to breathe as slowly and deeply as possible 5) After the attack and as soon as they feel better, the child can return to normal school activities 6) The child’s parents must be informed of the attack. Emergency situation Call the ambulance urgently (dial 999) if 1) 2) 3) 4) 5) The reliever has no effect after 5-10 minutes The child is either distressed or unable to talk The child is getting exhausted The carer/ staff member has any doubts about the child’s condition Continue to give reliever medication every few minutes until help arrives. Exercise induced asthma Exercise can bring on an attack of asthma. This varies from day to day in an individual child and can be particularly problematic in a child with a respiratory infection, soon after an asthma attack or in very cold weather. It may come on after the exercise is complete rather than during the exercise. Exercise induced asthma can frequently be prevented by a simple “warm up” period and use of the reliever medication immediately prior to the exercise. Optimal use of the preventer medication can also make exercise induced asthma less likely. Any asthma attack should be managed as under “How to manage an asthma attack” Signed: Chair of Curriculum Committee …………………………………… Date …………………….. …………………………………… Date …………………….. Signed: Chair of Governors Asthma Policy Questionnaire Child’s name ……………………………………… Emergency contact telephone number ……………………………………… Date of Birth ……………………………………… Own Doctor (G.P./ Consultant) ……………………………………… Is there a family history of asthma? Yes / No Does your child suffer from:1) 2) 3) 4) 5) Regular chest infections Allergies Persistent night coughs Persistent wheezing Cough or wheeze after exercise Yes / No Yes / No Yes / No Yes / No Yes / No Has your child been diagnosed with asthma? Yes / No Does your child take any medication for asthma? – please specify name and frequency of usage Yes / No 1) 2) 3) 4) Does your child need help with their inhaler (if any)? Yes / No Does your child ever miss PE/Games at school because of their Asthma and if so, how often? ……………………………... Do you know of anything that makes your child’s asthma worse? If so please specify Yes / No …………………………………………………………………………... How many times, in the past 12 months, has your child: 1) Been admitted to hospital because of asthma 2) Seen a G.P. for an asthma attack/episode 3) Attended an asthma clinic either at hospital or your G.P.s ……………………… ……………………… ……………………… It is proposed that should your child require treatment for their asthma whilst at school, the above policy will be followed and you will be informed. If you object to this, you should inform the child’s teacher in writing. Parental/guardian advice of asthma attack/ emergency medication usage This note is to inform you that: Name of child ………………………………………… Class ……………………………. Needed to use (name of medication) ……………………………………………… Date and Time ……………………………………………… ……………………………………………… ……………………………………………… Signed (Staff member) ………………………………………………