Congenital and Hereditary Retinal and Optic Nerve Disease
advertisement

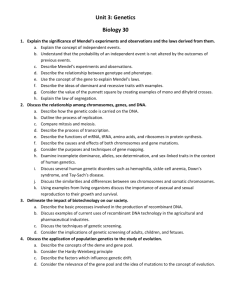
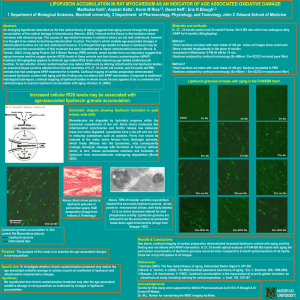
1 I. II. Orphan Diseases Definitions Retinitis Pigmentosa a. Prevalence i. 1 in 3500 people worldwide; 100,000 in the US b. Clinical characteristics i. Attenuated arterioles ii. Pigment degeneration iii. Pale waxy disc iv. PSC cataract v. CME c. Symptoms i. Night blindness ii. Field loss d. Types i. Diffuse RP ii. Sector RP iii. RP Sine Pigmento iv. RP Albescens v. Usher’s syndrome (RP with deafness) 1. 16,000 cases in US e. Diagnostic testing i. ERG ii. VF f. Hereditary patterns i. AD, AR, Sex-linked g. Differential from cone-rod dystrophies h. Genetics i. Dominant RP Genes 1. RHO (Rhodopsin)-30% a. 12-15%: Pro23His mutations b. 5%: Pr0347Leu mutations 2. Peripherin/human Retinal degeneration Slow (RDS-10% ii. Recessive 1. As many as 60 genes iii. X-linked RP 1. RPGR gene (75%) 2. RP2 (25%) iv. Usher’s Syndrome i. Treatment for a Future of Care i. Genetic testing ii. Gene specific treatments 1. Gene replacement 2. Knockdown by RNAi iii. Other treatments 1. Neurotophic factors-photoreceptor cell rescue 2 III. IV. V. 2. Vaccination against neurodegeneration 3. Drug therapy 4. Nutrient therapy Leber Congenital Amaurosis a. Prevalence i. 5000 cases in the US b. Clinical characteristics i. Normal fundus early on ii. Eventual mottling and degeneration c. Symptoms i. Severely reduced VA from birth ii. Nystagmus iii. Night blindness d. Diagnostic tests i. ERG e. Types i. Simple LCA ii. Complicated LCA f. Hereditary patterns i. AR ii. AD (extremely rare) g. Genetics i. Eight genes account for 10% of cases 1. RPE65, RDH12,CRX, RP-GRIP, AIPL1, CRB1, GUCY2D, TULP1 genes h. Treatment for a Future of Care i. Genetic testing ii. Bypassing biochemical steps iii. Prevention of cone loss using injections of 11-cis chromophores iv. Gene replacement 1. Success in Briard dogs Achromatopsia a. Clinical characteristics i. Macular granularity b. Symptoms i. Nystagmus ii. Reduced VA from birth iii. Abnormal color vision c. Hereditary pattern i. AR d. Genetics i. ACHM2, ACHM3 ABCA-4 Dystrophies a. Stargardt Disease/ Fundus Flavimaculatus i. Prevalence 1. 1 in 10,000 children; 30,000 in the US 3 VI. ii. Clinical characteristics (may include one or more) 1. Early macular granularity 2. Eventual “beaten-bronze” macula 3. Fish-tail shaped lipofuscin flecks iii. Symptoms 1. Loss of acuity in teenage years 2. Central scotomas (paracentral) 3. Various rates of progression iv. Diagnostic testing v. Hereditary patterns 1. AR, AD Stargardt-Like Dystrophy vi. Differential Diagnosis from other White Dot Diseases vii. Genetics 1. ABCA-4 mutations on short arm of chromosome 1 a. Results in formation of toxic A2E i. Contributes to lipofuscin formation viii. Treatment for a Future of Care 1. Genetic testing 2. Drugs to reduce A2E accumulation b. Other ABCA-4 Dystrophies i. Cone and Cone-rod dystrophy 1. Clinical characteristics a. Bull’s eye macular lesion b. Macular granularity 2. Symptoms a. Color vision loss b. Acuity loss c. Variable progression 3. Diagnostic tests a. ERG b. FA 4. Hereditary patterns a. AR, AD ii. AMD (1-2%) Other Macular Disorders a. Pattern Dystrophy of the RPE i. Clinical characteristics 1. Lipofuscin deposits in the macula a. Butterfly-shaped b. Reticular pattern ii. Symptoms 1. Mild loss of VA iii. Hereditary pattern 1. AD iv. Genetics 1. RDS gene 4 VII. b. X-Linked Juvenile Retinoschisis i. Clinical Characteristics 1. Foveal schisis 2. Reduced VA at birth 3. Inferotemporal schisis ii. Hereditary pattern 1. Sex-linked 2. Males affected iii. Genetics 1. XLRS1 gene c. Best’s Vitelliform Dystrophy i. Clinical characteristics 1. Lipofuscin disorder of the RPE 2. Egg-yolk macular lesion early on with good VA 3. Scrambled-egg lesion with reduced VA a. CNV development ii. Diagnostic testing 1. EOG iii. Hereditary pattern iv. Differential from other maculopathies 1. Adult-onset vitelliform dystrophy v. Genetics 1. Bestrophin gene mutations vi. Treatment for a Future of Care 1. No good animal models available at present 2. Monitor for CNV A Future of Care a. Importance of Diagnosing Orphan Disease i. Pedigree construction 1. Determine pattern of inheritance in single gene diseases 2. Ask about consanguinity or close geographic relation ii. Genetic testing 1. Available sites: a. www.carverlab.org b. www.genetests.org