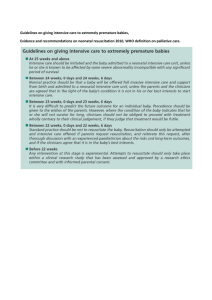
Guidance notes to assist with completing this form
advertisement

Policy: Executive Summary and associated documents Resuscitation (In- Patient Unit) Policy and Procedure POLICY STATEMENT: A decision whether to attempt cardiopulmonary resuscitation (CPR) or not in the event of an unexpected cardiac/respiratory arrest should be made and recorded in individuals with advanced disease in advance of the possible event. Decisions will be made in accordance with the patient’s wishes and clinical condition. Such a decision does not refer to other measures to relieve reversible causes of cardiorespiratory collapse – for example, a blocked tracheostomy tube may be relieved by suction, or measures to treat anaphylaxis as a response to medication or blood transfusion may still be undertaken. A decision whether or not to resuscitate will make no difference to other clinical care and support. This will be maintained on an individual basis to the highest standard possible. The following have been used in the preparation of this Policy: A Joint Statement from the British Medical Association, the Resuscitation Council (UK), and the Royal College of Nursing. Resuscitation Council (UK), published in October 2007i. New recommended standards for recording DNAR (Do Not Attempt Resuscitation) decisions have been issued in 2009 by the Resuscitation Councilii. The GMC document, Withholding and Withdrawing Life-Prolonging Treatments: Good Practice in Decision-making – in 2002iii. This policy respects the individual’s absolute right to life in accordance with the Human Rights Act (1998)iv and the Mental Capacity Act (2005)v. RELATED HOSPICE POLICIES AND PROCEDURES: Description of Amendment(s) Safeguarding Adults Updated abbreviation “DNACPR”. Reference to new community DNACPR policy. 2.4.13 This Policy will impact on:Policy Area Effective Date: Author (full job title) All Clinical Staff Ratified by: Clinical June 2008 Review Date: Sept 2014 Dr Trevor Rimmer Macmillan Palliative Consultant / Medical Director Approval Record Date Ratified by Clinical Governance Sept 2011 Hospice Director: Mike Pyrah Resuscitation (In- Patient Unit) Policy and Procedure AIMS: To have clear decisions recorded for individuals who experience a cardiorespiratory collapse before the event, so staff can make an immediate decision as to what action to take at the time such an event occurs. To avoid offering or giving CPR to patients when it would be unsuccessful, allowing a natural and dignified death. To enable discussion and decision making with patients if CPR might be successful in the case of cardiorespiratory arrest, or, if not mentally competent, the patient’s representative(s) To ensure that, in the case of a cardiorespiratory arrest, there are always staff present who are competent to initiate basic CPR and call for help. STAFF RESPONSIBILITIES: The ultimate responsibility for resuscitation decisions lies with the Medical Director, or, in his/her absence, the senior doctor on duty, supported by senior nursing staff. If the patient has difficulty understanding or communicating decisions, due to sensory impairment, physical disability, lack of understanding of English or other reason, then all reasonable effort should be made to assist them in all relevant discussions. The admitting doctor has responsibility for: Deciding whether to make a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) order on the clinical grounds that resuscitation would be unsuccessful If an Advance Plan has been made, deciding if it is applicable, and if so making a DNACPR order accordingly Deciding whether to discuss resuscitation with the patient, or, if not competent, the family or legal representative, and recording the outcome of any discussions on the Resuscitation Order form Discussing such decisions with the appropriate qualified nurse on duty and recording agreement, or otherwise Recording details if there is disagreement about the decision, and bringing this to the attention of the Medical Director and/or Head of Clinical Services as soon as is practical The admitting nurse has the responsibility to: Discuss the resuscitation decision with the admitting doctor Countersign the resuscitation order if in agreement; or recording reasons for disagreeing with such a decision if agreement is not reached Ensure that the resuscitation status of the patient is known by the nursing team Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 1 of 11 The doctor doing the daily ward round should: update resuscitation decisions on the Resuscitation Order where a review date has been set or the patient’s condition or decision has changed record changes in resuscitation decisions by completing a new Resuscitation Order form and striking out the old one discussing any changes in the resuscitation decision with the responsible qualified nurse on duty caring for the patient concerned The qualified nurse on duty caring for the patient should: check that resuscitation details are up to date, and inform the doctor doing the ward round if this needs updating if resuscitation details are altered, discuss this with duty doctor and countersign the Resuscitation Order ensure that changes in the resuscitation status of the patient is known by the nursing team and marked All qualified staff should have training in Basic Life Support annually. PROCEDURE: For patients for whom no prior decision has been made and recorded - in the event of a cardiorespiratory arrest, CPR should be attempted, unless a doctor or senior nurse who knows the patient well is present and able to make a decision not to resuscitate. Such a decision must be recorded in the clinical notes, with the reasons for which it was made and the Duty Doctor, Medical Director or Head of Clinical Services informed as soon as possible. If a patient has been transferred from another unit or situation with a valid DNACPR order from the referring team, then this shall normally be respected as guidance until the individual has been assessed and admitted by the clinical team. After admission to the Hospice and medical assessment, a Resuscitation Order (“Orange Form”) shall be completed, and confirmed in the clinical notes in the medical admission section. The decision shall be clearly marked as “R” (Resuscitate) or “DNAR” (Do Not Attempt ... Resuscitation). In most people referred to the hospice, there is an identifiable risk of cardiac or respiratory arrest, such as an underlying incurable condition (e.g. advanced cancer), the history (e.g. severe advanced heart failure or respiratory disease), or current clinical condition (e.g. renal or liver failure). A significant minority of patients, particularly those admitted for neurological respite care or symptom control with a prognosis of months or years, have a relatively low risk, and would have a relatively good chance of successful CPR in the case of a cardiorespiratory arrest. Thus a decision should be made in advance about the appropriateness of CPR whenever possible. 1. A DNACPR order applies only to in-patients of the East Cheshire Hospice. The Resuscitation Order refers solely to cardiopulmonary resuscitation; i.e. in the event of a cardiac or respiratory arrest no attempts at cardiopulmonary resuscitation will be made. No other treatment and care, where appropriate, shall be precluded or influenced by a Do Not Attempt CPR decision. 2. The decision is only valid during the patient’s current in-patient admission and is automatically revoked on discharge from the hospice. A new Resuscitation Order must be made on any subsequent admissions. The old form should be struck through on discharge. 3. If an individual near the end of life is being sent home by urgent discharge, in order that he or she can die at home according to their wishes, then a valid Community DNACPR Order should be Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 2 of 11 completed, and NWAS (North West Ambulance Service) be informed by the appropriate form, in accordance with the “Do Not Attempt Cardiopulmonary Resuscitation Adult Policy for Central and Eastern Cheshire Primary Care and Community Services”. A copy of the original may be given to the transferring ambulance crew. The policy and copies of relevant forms, together with contact details, are available at: http://www.cheshire-epaige.nhs.uk/Stages/DNA-CPR%20in%20the%20Community.aspx . 4. Any decision not to undertake CPR on a patient is taken following appropriate consideration of the likely clinical outcome and the patient’s known wishes. The following guidelines may support a decision not for CPR: 4.1 Where attempting CPR could not restart the patient’s heart and breathing. If the health care team is as certain as it can be that attempting CPR would not restart the patient’s heart and breathing because of the patient’s clinical condition, the patient cannot gain any clinical benefit from an attempt. This should be a team decision and based on clinical assessment of the patient’s condition and up-to-date clinical guidelines, and in the patient’s best interests. 4.2 Where there is no benefit in restarting the patient’s heart and breathing. If the individual is terminally ill and death is inevitable within a short period of time, then that person should be allowed to die naturally with full comfort and palliative measures. Normally the patient and/or relatives and carers should be made aware of the condition and situation. Occasionally discussion with patient and/or family members may not be appropriate or possible and in this situation the doctor should use his/her discretion – this should be recorded and discussed with the nursing staff. An example would be a patient who has impaired consciousness or delirium, or has previously expressed a desire not to be informed. An explanation for not involving the patient and/ or relatives in the decision-making process should be documented on the Resuscitation form - e.g. patient lacks capacity and relatives not available. 4.3 Where the expected benefit is outweighed by the burdens of resuscitation. Where CPR may be successful in restarting the patient’s heart and breathing, and thus prolong the patient’s life, the benefits to be gained from the prolongation of life must be weighed against the burdens to the patient of the treatment. Again, this should be a team decision and based on clinical assessment of the patient’s condition and up-to-date clinical guidelines and in the patient’s best interests. 4.4 Where the patient with capacity has asked that CPR NOT be attempted. It is established in law and ethics that adults with capacity have the right to refuse any medical treatment, even if that refusal may result in death. The Hospice will respect the individual’s wishes. A summary of any such discussion should be made in the case records and witnessed. If a patient decides they do not wish to have CPR attempted, and this was against the advice of the medical team, this should be documented carefully in the medical record and countersigned by the patient. Unless this decision is signed by the patient and the signature is witnessed, it is unlikely to meet the legal criteria for a valid advance decision. Thus some patients may prefer to make a formal, written advance decision. If the patient is unable to write, someone else should write it down for them – e.g. a family member can write down the decision on their behalf, or a healthcare professional can record it in the person’s healthcare notes. If the patient is unable to sign, they can direct someone to sign on their behalf in their presence. This must be witnessed. The witness must then sign to indicate that they have witnessed the nominated person signing the document in front of the patient making the advance decision (see the Mental Capacity Act Code of Practice, Chapter 9 – “What does the Act say about advance decisions to refuse treatment?”vi Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 3 of 11 4.5 Where a patient has a valid Advance Directive clearly refusing cardio-pulmonary resuscitation. This must be assessed for validity and applicability (see the Mental Capacity Act Code of Practice, Chapter 9 – “What does the Act say about advance decisions to refuse treatment?”vii An advance decision to refuse life-sustaining treatment must meet specific requirements: It must be put in writing. If the person is unable to write, someone else should write it down for them. The advance decision must include a clear, specific written statement from the patient making an advance decision to refuse CPR even if life is at risk. If this statement is made at a different time or in a separate document to the advance decision, the patient making the advance decision (or someone they have directed to sign) must sign it in the presence of a witness, who must also sign it. If there is any doubt about the validity of an Advance Directive, legal advice should be sought as soon as possible. 4.6 If a patient or a proxy decision maker is requesting CPR in the case of a cardiorespiratory arrest, but the healthcare team believes that this would not re-start the heart and breathing, this should be explained in a sensitive way. These discussions may be difficult and should be carried out by experienced senior clinicians. If the decision is not accepted, then a second opinion should be offered. It may be necessary to consider transfer to the District General Hospital if the risk of cardiorespiratory arrest is high. 4.7 If a patient is to undergo a surgical or other invasive procedure (such as cardiac catheterization, pacemaker insertion) in a hospital unit then it may be appropriate to suspend a DNACPR order for the duration of the procedure and monitored recovery. Under these circumstances, the risk of precipitating an arrhythmia is increased, but the arrest is much more likely to be quickly and readily reversible. Such a decision must be reviewed before transfer for the procedure with the patient, or their appointed representative if they lack capacity, as part of the consent process. If a patient wishes an advance decision refusing CPR to remain valid during such a procedure and this would significantly increase the risks, and the clinician believes that it would not be safe or successful with the DNACPR order in place, it would be reasonable not to proceed. The agreed DNACPR management option must be documented and communicated to all the healthcare staff managing the patient during the procedure and recovery. 5. If the patient lacks mental capacity and has an appointed health proxy (Personal Welfare Lasting Power of Attorney or a Court Appointed Deputy) then decisions about resuscitation must be discussed with them. A Welfare Attorney may be able to refuse life-sustaining treatment on behalf of the patient, if this power is included in the original Lasting Power of Attorney. Such a representative cannot insist upon CPR if it is felt by the medical team not to be in the patient’s best interests. If the patient has an Independent Mental Capacity Advocate (IMCA), then there should be discussion before a decision is made. If there is disagreement then a second opinion should be obtained. Please refer to the East Cheshire Hospice Capacity and Consent Policy Procedures. DOCUMENTATION AND COMMUNICATION 1. The Resuscitation Order (RO) form is printed on a single sheet of Orange A4 paper as shown in appendix 1. The form must be completed in full, and no abbreviations should be used. It must be dated and signed with the doctor’s name and position (section 6). The guidelines for the use of the form are printed on the reverse. Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 4 of 11 2. The doctor recording the decision should insert this form securely into the front of the patient’s medical records and document the decision in the case notes in the appropriate section of the medical admissions assessment form. If applicable state clearly what was discussed and agreed with the patient or health proxy. 3. It is the responsibility of this doctor to ensure that the decision is communicated to the qualified nurse caring for the patient who should be involved in the decision making process. This should be documented, dated and signed on the RO (section 5). 4. It is the duty of this nurse to ensure that this decision is communicated to all other relevant members of staff and documented in the nursing notes REVIEW 1. The Resuscitation Order is valid for the duration of the patient’s admission unless a review date is set. If a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Order is made, and the patient’s condition is not likely to improve or expected to deteriorate, then it is not necessary to review this again for the duration of the admission. It may be necessary to make a temporary order for Resuscitation or DNACPR if the patient’s condition is variable, or if desired by the patient. In this case a review date should be set in section 7. If repeated review dates need setting, then a further RO must be completed and the old one struck out and filed. It is not usually necessary to discuss CPR with the patient each time the decision is reviewed. However, where a patient has previously been informed of a decision and it subsequently changes, they should be informed of the change of decision and the reason for it, where appropriate. The details of the decision and discussion should be recorded in the medical record. 2. If the decision is altered, and when the patient is discharged home, the Resuscitation Order should be crossed through with 2 diagonal lines in black ink, with the date, name and signature of the healthcare professional cancelling the order clearly written. The form should then be removed from the front of the patient’s medical records and filed chronologically with the appropriate medical notes. If an urgent discharge requires a Resuscitation Order for the ambulance crew, a fresh one should be written and given to them, with a photocopy for the case notes. VALIDITY 1. A fixed review date is not now required in all cases (in contrast to the previous policy). 2. The decision not to resuscitate a patient is valid for the current in-patient admission only, or for the period of time documented at the last review if specified, unless the order is cancelled. 3. Any Do Not Attempt CPR orders recorded in the medical or nursing notes relating to a previous admission are no longer valid. 4. If the decision is appropriate for a subsequent admission, another Do Not Attempt CPR form must be completed, signed, dated and filed as above. NOTE Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 5 of 11 A community DNACPR policy is being rolled out in the North West of England starting 2013. This is unlikely to happen in the Central and Eastern Cheshire locality before 2014. Practice is likely to change little in relation to discharging patients with Community DNACPR forms. The Hospice will change practice in order to concord with any necessary changes in this area. Definitions Cardiopulmonary arrest – collapse due to cessation of effective cardiac output (“cardiac arrest”) and respiration Cardiopulmonary resuscitation – Basic - cardiac massage and artificial respiration in an attempt to support circulation and oxygenation of the tissues – Advanced - defibrillation and/or intravenous or intracardiac drugs, with specialist aftercare in a hospital unit Training Requirements Basic life support for nursing and medical staff. STATUTORY REFERENCES: Decisions Relating To Cardiopulmonary Resuscitation. October 2007. A Joint Statement from the British Medical Association, the Resuscitation Council (UK) and The Royal College Of Nursing. British Medical Association, London (2007). Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 6 of 11 Recommended standards for recording "Do not attempt resuscitation" (DNAR) decisions. Resuscitation Council (UK) (2009). Mental Capacity Act 2005. Policy Name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Jun 2008 Sep 2014 Page 7 of 11 Appendix 1 East Cheshire Hospice In-Patient Unit RESUSCITATION ORDER Revised August 2009 See Reverse for Guidance Notes to help in completing this form. ORDER (MARK R OR DNAR) Name of Patient ………………………………………… DoB …………………… Hospice Number …………… Address R = Attempt Resuscitation DNAR = Do Not Attempt Resuscitation Date of Order …………………………………………… If A DNAR decision is made, in the event of cardiac or respiratory arrest no attempts at cardiopulmonary resuscitation will be made. All other appropriate treatment and care will be provided. 1 Does the patient have capacity to make and communicate decisions about CPR? YES / NO If “NO”, are you aware of a valid advance decision refusing CPR which is relevant to the current condition? If “YES”, go to box 5 YES / NO If “NO”, has the patient appointed a Welfare Attorney (as part of a Lasting Power of Attorney) to make decisions on their behalf? If “YES” they must be consulted. YES / NO All other decisions must be made in the patient’s best interests and comply with current law. Go to box 2 2 Summary of main clinical problems & reasons why CPR would be inappropriate, unsuccessful or not in the patient’s best interests: 3 Summary of communication with patient (or Welfare Attorney). If this decision has not been discussed with the patient or Welfare Attorney state the reason why: 4 Summary of communication with patient’s relatives or friends: 5 Healthcare professional (i.e. Registered Doctor) completing this DNAR order: Name (PRINT) ………………………………………………………… Position ………………………………….. 6 Signature ………………………………….. Date …………….. Time …………….. Qualified Nurse caring for the patient: Name (PRINT) ………………………………………………………… Signature ………………………………….. Date …………….. Time …………….. Names, signatures and positions of other members of multidisciplinary team: 7 ………………………………………………………..……… ……………………………………………………………. ………………………………………………………..……… ……………………………………………………………. ………………………………………………………..……… ……………………………………………………………. Mark review date(s) if appropriate or write “Indefinite” here: ……………………………………………………… Date ……………… Name (PRINT) …………………………………………. Signature ……………………………… Date ……………… Name (PRINT) …………………………………………. Signature ……………………………… Date ……………… Name (PRINT) …………………………………………. Signature ……………………………… Policy name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Oct 2009 Sep 2014 Page 8 of 11 Guidance notes to assist with completing this form This form should be completed legibly in black ball point ink. All sections should be completed. The patient’s full name, date of birth and address should be written clearly or addressograph attached. The date of writing the order should be entered. Enter detail in Clinical Notes. This should be in the appropriate section of the Admission Assessment Form; if the decision is made after admission, then an acceptable entry would be “In the event of cardiac or respiratory arrest patient is not for Cardiopulmonary Resuscitation” (do not use abbreviations). This order will be regarded as “INDEFINITE” for this hospice admission unless it is clearly cancelled or a definite review date is specified. The order should be reviewed whenever clinically appropriate such as a change in the patient’s condition. On discharge the order must be cancelled using the instructions below. If the decision is cancelled the form should be crossed through with 2 diagonal lines in black ballpoint ink and “CANCELLED” written clearly between them, signed and dated by the healthcare professional cancelling the order. 1. Capacity / advance decisions Record the assessment of capacity in the clinical notes. Ensure that any advance decision is valid for the patient’s current circumstances. 16 and 17-year-olds: Whilst 16 and 17-year-olds with capacity are treated as adults for the purposes of consent, parental responsibility will continue until they reach age 18. Legal advice should be sought in the event of disagreements on this issue between a young person of 16 or 17 and those holding parental responsibility. 2. Summary of the main clinical problems and reasons why CPR would be inappropriate, unsuccessful, or not in the patient’s best interests Be as specific as possible. If space on form is insufficient, write more detail in the case notes and indicate that this has been done. 3. Summary of communication with patient Whenever possible and appropriate this decision should be discussed with the patient. State clearly what was discussed and agreed. The CPR information booklet should be given to the patient at this time. If this decision was not discussed with the patient, state the reason why this was inappropriate. 4. Summary of communication with patient’s relatives or friends If the patient does not have capacity, their relatives or friends should be consulted and may be able to help by indicating what the patient would decide, if able to do so. If the patient has made a Lasting Power of Attorney, appointing a Welfare Attorney to make decisions on their behalf, that person must be consulted. A Welfare Attorney may be able to refuse life-sustaining treatment on behalf of the patient, if this power is included in the original Lasting Power of Attorney. If the patient has capacity ensure that discussion with others does not breach confidentiality. State the names and relationships of relatives or friends or other representatives with whom this decision has been discussed. More detailed description of such discussion should be recorded in the clinical notes where appropriate. 5. Healthcare professional completing this DNAR order This must be a qualified doctor contracted to work within the Hospice. 6. Members of multidisciplinary team The qualified nurse caring for the patient is to sign and date the form at the time of the decision being made. It is the duty of this nurse to ensure that this decision is communicated to all relevant members of staff and documented in the nursing notes. State the names and positions of multidisciplinary team members contributing to this decision as appropriate. 7. Review A routine fixed review date is not recommended. If it is most unlikely that circumstances will change, then this section may be endorsed as “Indefinite”, for the duration of the patient’s admission. If there is some uncertainty, a date for review should be set on the form. In addition, a review should occur whenever circumstances change. Policy name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Oct 2009 Sep 2014 Page 9 of 11 i A Joint Statement from the British Medical Association, the Resuscitation Council (UK), and the Royal College of Nursing. Resuscitation Council (UK) 2007. At http://www.resus.org.uk/pages/dnar.htm (accessed 18/8/09) ii Recommended standards for recording "Do not attempt resuscitation" (DNAR) decisions. Resuscitation Council (UK). At http://www.resus.org.uk/pages/DNARrstd.htm (accessed 18/8/09) iii Withholding and Withdrawing Life-Prolonging Treatments: Good Practice in Decision-making. General Medical Council, London (2002). At http://www.gmc-uk.org/guidance/current/library/witholding_lifeprolonging_guidance.asp (accessed 18/8/09) iv A Guide to the Human Rights Act 1998: Third Edition. Department for Constitutional Affairs, London. (2006). Available at http://www.justice.gov.uk/guidance/docs/act-studyguide.pdf (accessed 18/8/09) v Department of Health. Mental Capacity Act 2005. Available at http://www.dh.gov.uk/en/SocialCare/Deliveringadultsocialcare/MentalCapacity/index.htm (accessed 2/7/09) vi Mental Capacity Act Code of Practice. The Stationery Office, London (2007). At http://trustnet/MCA%20Code%20of%20Practice.pdf (accessed 15/7/09) if at East Cheshire NHS Trust, or see below) vii Mental Capacity Act Code of Practice. The Stationery Office, London (2007). At http://www.dca.gov.uk/menincap/legis.htm#codeofpractice (accessed 18/8/09) Policy name: Issue Date: Review Date: Resuscitation (In-Patient Unit) Oct 2009 Sep 2014 Page 10 of 11