Vaccines and Preventable Communicable Illness of Childhood
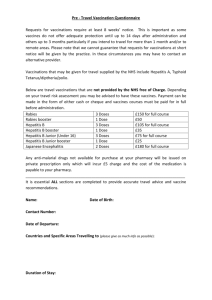
advertisement

Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 1 of 13 CHILDHOOD IMMUNIZATIONS The introduction of vaccines against childhood diseases such as measles, mumps, rubella, polio, whooping Cough (pertussis), diphtheria, smallpox, haemophilus influenza, hepatitis b and varicella has greatly improved the quality of life for both children and adults. Vaccines need to be administered at specific ages and time intervals, timing for the first sets of immunizations is determined by the age in which transplacental immunity decreases or disappears, and the infant has the ability to make antibodies in response to the disease. The effectiveness of vaccines depends on proper storage and handling. Most vaccines need to be refrigerated and Varivax (for varicella) needs to be kept frozen, when involved in the administration of vaccine, the RN is responsible for both the proper storage and handling. TYPES OF IMMUNIZATIONS Live attenuated (live virus) can cause illness o MMR, Varivax Inactivated (killed virus vaccine) o DTaP (Diptheria, Tentanus, accelerated Pertussis), HiB (influenza), IPV (polio), Prevnar (pneumococcal disesases) Recombinant (genetically rendered) o Hep A, B Immunoglobulins (IVIG) o Varicella, Measles, RSV, Rabies, Tetanus, hepatitis A, B, C Botulism PEDIATRIC NURSING RESPONSIBILITIES AND NURSING INTERVENTIONS Be prepared for life-threatening reaction whenever immunizing children. At every visit/encounter child’s immunizations record should be reviewed. Review of child’s allergies (food and medicine). Review potential contraindications to each vaccines Review past immunization history for past reactions Assess child for anxiety and fear related to administration Obtain informed consent. In females of child bearing age (11-50) perform rapid urine HCG before administering Live vaccines (MMR/Varicella). Parent and patient education about the need for specific vaccinations, risk of not getting vaccination and getting dieses and potential side effects of vaccine. Record vaccines administered in patients chart and vaccine record (card) Federal law requires that patient and parent are given VIS (vaccine information statement) in APPROPRIATE language before discharge. Monitor child for 15 minutes post vaccination. Report all vaccine related reactions using the federal VAERS (vaccine adverse reaction reporting system) and as per institution policy. Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 2 of 13 Things to have on hand when administering immunizations: o Epinephrine o Benadryl o Airway DTaP VACCINE: DIPHTHERIA, TETANUS, aCELLULAR PERTUSSIS Ages: 2, 4, 6, 15-18 months; 4-6 years with a separate Td (tetanus booster) at age 11-12y; Td booster every 10 years for life; Total 5 doses. Route: IM Common side effects: Redness, swelling, pain at injection site; T >100.9; drowsiness, anorexia. Serious side effects: Anaphylaxis, shock or collapse, fever > 102, persistent, inconsolable crying, seizure, encephalopathy. Contraindications: Occurrence of a serious side effect after previous dose. NURSING CONSIDERATIONS DTaP VACCINE Use the same brand whenever possible. Carefully question parents if they say the child had previous reaction to immunizations Inform parents of increased risk of reaction to doses 4 and 5 If child had a serious adverse reaction to any previous dose, the next doses should be deferred. This is the one children have reactions to. DIPHTHERIA A bacterium that occurs in winter. Symptoms can be mild – severe with a gradual onset (1-2 days). Low-grade fever, malaise, anorexia, rhinorrhea (with foul odor), hoarseness, stridor, cervical lymphadenitis, pharyngitis. There is a characteristic membrane that covers the tonsils, it is a membranous thick bluish white to grayish black in color, can spread to the soft & hard palates. Any attempt to remove the membrane results in significant bleeding. Treatment: Administration of IV antitoxin within 3 days of onset of sx. Also PCN G and surgical removal of membrane if occluding airway. Maternal antibodies last as long as 6 months Transmission: Contact with infectious nasal or eye discharge, unpasturized milk can also serve as a mode of transmission. Complications: Produces an endotoxin that causes myocarditis, peripheral neuropathy and a ascending paralysis (similar to Guillain-Barre syndrome). Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 3 of 13 PERTUSSIS (WHOOPING COUGH) Most common in children under 6 months of age Occurs frequently in HC workers and adults that are immunosuppressed, adults have mild illness but spread to nonimmunized kids. Starts with runny nose followed by an irregular, non-productive cough, cough becomes severe at night and changes into spasms of paroxysmal coughing followed by inspiratory stridor or “whooping”, the whooping sound is produced by forceful inhalations and a narrowed glottis. Non-stop coughing. Accompanied by flushing, cyanosis (from coughing fits), vomiting, and profuse drainage from eyes, nose, and mouth. Dehydration may occur from decreased PO intake. Paroxysmal coughing may last up to 2 weeks. Treatment: erythromycin TETANUS Characterized by painful muscular rigidity, usually of the mastoid bone and neck muscles. Tetanus spore are found in soil, dust and the gut of humans and animals. Tetanus is not an invasive organism but enters a susceptible host through an opening in the skin, usually a puncture wound, burn or crushed injury. In the newborn, infection may occur through the umbilical cord (when child is delivered in an unsanitary way using a “dirty” instrument to cut the cord). Substance abusers are particularly susceptible through using contaminated injectable drug equipment. Organism multiples and grows rapidly in “unclean” wound and the endotoxin affects the CNS, there are several forms of Tetanus but the most common form is the most lethal. Initial sx: stiff neck, tenderness of the muscles in the jaw & neck, eventually all voluntary muscles are affected, complete recovery is possible Mortality is about 30%, infections in the newborn are almost always fatal. POLIO VACCINE OPV: Oral polio vaccine, live virus - NO LONGER USED IN USA. IPV: Inactive Polio Vaccine, killed virus. Ages: Route: Common side effects: Serious side effects: Contraindications: . 2, 4, 6-18 months, booster at 4-6 years. Total 4 doses SQ Swelling and tenderness at injection site, irritability. Anaphylaxis Hypersensitivity to vaccine components, allergy to neomycin, streptomycin and polymyxin B Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 4 of 13 POLIOMYELITIS 3 identified types and a “wild-type”. Polio affects the CNS and causes paralytic disease. Causes fever, headache, decreased deep tendon reflexes, progressive weakness and paralysis. The paralysis results from damage to neurons; onset of paralysis may be sudden or gradual (3- 5 days) and is accompanied by respiratory difficulties leading to respiratory distress and respiratory failure. Pt will require intubation/tracheostomy and mechanical ventilation OPV: Oral polio vaccine, live virus vaccine. Virus is excreted in stool. No longer used in the U.S. Complications of Polio: Permanent motor paralysis, respiratory arrest, myocardial failure, aseptic meningitis. MMR VACCINE: MEASLES, MUMPS & RUBELLA - Combination Live Vaccine Ages: 12- 15 months, 4-6 years (Total 2 doses) Route: SQ Common side effects: Elevated temperatures 1-2 weeks after immunization, redness/pain at injection site, joint pain. Serious side effects: Anaphylaxis, encephalopathy, thrombocytopenia, chronic arthritis. Contraindications: Allergy to neomycin or gelatin Severely impaired immune system (HIV/AIDS, cancer or other immunosuppressant medications or treatments. MMR cannot be given to any child with a history of cancer (accept order for MMR only from a Pediatric Hematologist/Oncologist). Children with HIV can get MMR (CD4 count must be assessed prior to administration) Cannot be given within 3 months of blood or blood product transfusion Cannot be given to pregnant women NURSING CONSIDERATIONS: Allergy status Urine HcG for all women capable of being pregnant Question pt/parents abut immunosuppression Vaccine is a clear yellow solution that must be mixed with diluting before administration MMR and Varicella need to be mixed; MMR is pale yellow (like urine). Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 5 of 13 MEASLES/ RUBEOLA (2 SHOTS) A viral illness that occurs most often in the late winter & early spring. Most cases are reported from children who immigrate to the US from countries which do not require vaccination and children who do not get vaccinated for various reasons. Vaccination provides life long immunity. Measles is a cause of significant cause of infant and child morbidity in developing countries. Measles Treatment: Mode of transmission: Incubation: Period of communicability: Complications of Measles: None, supportive only, abx used for secondary bacterial infections (which are very common) Airborne (resp droplets) 8-12 days During prodromal phase, ends 2-4 days after rash appears. Diarrhea, OM, bronchopneumonia, encephalitis *Measles in an immunocompromised child can be fatal CLINICAL MANIFESTATIONS MEASLES Children are quite ill during prodromal phase with: High fever Conjunctivitis Cough Anorexia Small, irregular, bluish-white spots on buccal mucosa know as “Koplik spots” Characteristic red, blotchy maculorpapular rash appears 2-4 days after prodromal phase, rash begins on face and then spreads to trunk and extremities, Sx subside in 2-4 days MUMPS/PAROTITIS A paramyxovirus that occurs world wide in unvaccinated children, most often in late winter/early spring. Both infection and vaccination provide life long immunity. Maternal antibodies begin to disappear in the infant 12-15 months. Clinical manifestations of Mumps Malaise Low grade fever Decrease appetite Decreased activity level Unilateral parotid swelling, swelling peaks around day 3. Meningeal signs: stiff neck, headache, photophobia (in about 15% of pts) Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 6 of 13 Mumps Treatment: Mode of transmission: Incubation: Period of communicability: Complications of Measles: None, supportive only. saliva droplets and direct contact with secretions 12-25 days 7 days before swelling till 9 days after swelling subsides (can be as long as 2-3 weeks) Orchitis (unilateral scrotal swelling). Sterlity is a rare occurrence. Oophoritis, pancreatitis, aseptic meningitis and unilateral deafness (permanent and fairly common) RUBELLA/ GERMAN MEASLES German measles is a mild disease with a characteristic pink, maculorpapular rash that appears on the face, neck, trunk, legs and disappears in the same order. Clinical manifestations Rubella Prodromal sx begin 1-5 days before rash Low grade fever headache Malaise Sore throat Anorexia Generalized lymphadenopathy involving the postaricular, suboccipital and posterior cervical lymph nodes, common up to 7 days before rash begins. German Measles is a self limiting disease in children with very rare side effects. German Measles Treatment: Mode of transmission: Incubation: Period of communicability: Complications of Measles: None, supportive only. Droplets, direst contact with infected persons, or contact with articles soiled by nasal secretions 14-21 days 7 days before rash until about 4 days after. Infants with CRS shed virus for months and should not be cared to by susceptible persons, strict isolation from pregnant women (or potentially pregnant women) is required. Rare but includes arthritis in the adolescent, encephalitis, by far the most common and serious complication is CRS Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 7 of 13 CRS: CONGENITAL RUBELLA SYNDROME If mother is infected in the first trimester of pregnancy, the fetus can be severely affected: Spontaneous abortion Still birth Fetal death 10% of infected fetuses die after birth Multiple significant congenital anomalies are common, Severe congenital heart disease (pulmonary atresia-PA, tricuspid atresia-TA hypoplastic left heart syndrome-HLHS) IUGR Ear defects (causing deafness) Eye defects (causing congenital cataracts) Caused by mother not being immunized as a child, rates of CRS are on the rise; seen in immigrant populations. Infant can shed virus for months so HC workers, especially pregnant ones need to take contact precautions. HAEMOPHILUS INFLUENZA TYPE B VACCINE (HiB) trivia – causes epiglottitis Ages: 2, 4, 6, 12- 15 months (4 doses total) Route: IM Common side effects: pain, redness or swelling at injection site Serious side effects: anaphylaxis HAEMOPHILUS INFLUENZA TYPE B A bacterium which has several serotypes. Occurs in spring and summer. Most commonly affects infants and children in day care settings, LBW children, children with chronic illnesses. Invasive HiB disease was a major source of mortality and morbidity before routine vaccination was implemented (1987). Clinical manifestations of HiB disease HiB starts as a viral URI, the organism can pass though out the nasal mucosa to directly invade the blood stream, it causes several severe invasive illnesses: Meningitis Epiglottis Pneumonia Septic arthritis OM Bronchitis Pericarditis HiB disease is a leading cause of sepsis in newborns. Treatment is ampicillin, however 1/3 of strains are resistant. Rifampin may be given to unimmunized contacts. Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 8 of 13 HEPATITIS A, B, C, D, E AND G Hep A – HAV Most contagious form, fecal-oral route Hep B – HBV Blood and blood products (high % of HC workers) Hep C – HCV Blood/ blood products, sexual Hep D- HDV Only present with Hep B most common in IVDU/hemophiliacs Hep E – HEV (non-A non-B) fecal-oral route Hep G- HGV Transfusions and organ transplants exclusively Hep A and Hep B are preventable with a vaccine. Hepatitis = an acute inflammation of the liver. Acute viral Hepatitis is the most common cause of hepatitis. Hepatitis can also be caused by drugs (including alcohol) chemicals and autoimmune liver disease . It is a significant cause of morbidity and mortality in world wide. The changes in the liver tissue results in varying degrees of swelling, infiltration of the liver with subsequent degeneration, necrosis and fibrosis of the liver. Hepatitis can be self limiting and complete regeneration of liver cells can occur but it is unknown which case of Hepatitis will do so FULMINATE HEPATITIS Severe, acute disease with massive destruction of the liver which results in rapid liver failure followed by death 1-2 weeks after infection, usually caused by Hep B accompanied by Hep D. Most common cause is toxic reactions to drugs. SUB ACUTE OR CHRONIC HEPATITIS Progressive destruction of liver cells can be present for years as an asymptomatic infection but will eventually result in cirrhosis and liver failure PERINATAL HEP B Most hepatitis B infections are acquired in childhood either from the mother (perinatal) or as an adolescent (sexual transmission and IV drug use). Route of transmission from mom-fetus if the mother is a carrier or has active infections. The virus will cross the placental barrier late in pregnancy or during labor, when the child ingests amniotic fluid or via breast milk. Most women who pass Hep B to their fetus are unaware of their status. The infection can lie dormant for 2-3 decades and in their 30’s or 40’s the hepatitis can become active and can lead to cirrhosis and liver failure. Hepatitis B is the #1 cause of liver failure in the world and the number one reason for liver transplants in the US. Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 9 of 13 Clinical Manifestations of Hep B Insidious onset Jaundice Anorexia Malaise Nausea Abnormalities in LFT’s (SGOT/SGPT/Bilirubin) Prodromal sx’s: rash, arthritis, “aches & pains” TREATMENT FOR HEP B: No specific treatment, supportive. Prevention is the best treatment. Rest Hydration Nutritional support (high calorie, high protein, high carbohydrate, low fat diet ) Vitamin supplementation No Alcohol or drugs metabolized by the liver Hospitalization when sx are severe or clotting factors are altered More importantly treatment involves early detection, monitoring, recognition of chronic liver disease and the prevention of spread. Treatment with Monolclonal antibodies, a-interferon, and antiviral agents: Ribavirin has shown some success. Hepatitis B Vaccine Ages: Route: Common side effects: Serious side effects: Birth, 2 - mths, 6 – 18 mths (3 or 4 doses) IM Pain/redness at injection site, headache, photophobia, altered LFT’s Anaphylaxis, Guillian–Barre type illness with progressive muscle weakness. NURSING CONSIDERATIONS All pregnant women should be screened before birth (or immediately following birth), If mom is HbsAG+, vaccine must be given to infant within 12 hours, followed by HBIG to prevent transmission to infant. Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 10 of 13 Varivax Ages: Route: Storage and handling: Common side effects: Serious side effects: 12-18 months. 1 dose SQ Must be kept frozen and used within 30 minutes, cannot be refrozen Pain/redness at injection site, fever up to 38.8 (102), generalized rash, sub-acute varicella infection. Anaphylaxis NURSING CONSIDERATIONS Prior to immunization a carefully assessment of medical history must be obtained with emphasis on possible immunosuppression Urine HcG of all women that can potential be pregnant prior to immunization Assess for allergy to neomycin or gelatin VARICELLA (CHICKEN POX) A viral illness caused by the varicella- zoster virus, a herpes virus 6. Occurs in late fall, winter and spring. Maternal antibodies disappear 2-3 months after birth. The onset of symptoms is acute, mild fever, malaise, and irritability occurs before rash. Rash begins as a maculae on an erythematosus base and progresses to a papule, then a clear filled vesicle. Lesions of all stages can be present at one time. Rash starts on body. NURSING CONSIDERATIONS- VARICELLA Any child with a rash as described above should be put in isolation IMMEDIATELY If a case of varicella is diagnosed, ALL contacts at school, work, daycare, clinic, playgroup must be notified and assessed for infection. Treatment: Mode of transmission: Incubation: Period of communicability: Complications of Measles: None, supportive only. Direct contact with lesions, airborne spread of secretions 14-21 days up to 5 days before the onset of rash and until ALL lesions are crusted over. The incubation period may be extended in immunocompromised children In the healthy child complications are rare can include: secondary bacterial infections, hepatitis, pneumonia thrombocytopenia, Glomerulonephritis, Reye syndrome, encephalitis In the immunosuppressed child the results of a varicella infection can be catastrophic. Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 11 of 13 TREATMENT OF VARICELLA None, care is supportive. Oral and IV acyclovir (retroviral) is used for immunocompromised children ONLY. Most children with varicella recover fully with only supportive care (prevention of dehydration, reduction of fever, prevention of secondary bacterial skin infections) In an immunosuppressed child, prompt recognition and aggressive treatment with VZIG must begin immediately to prevent varicella pneumonia/overwhelming infection. Varicella immunoglobulin (VZIG) is used to prevent varicella in exposed, susceptible individuals at risk for complications. The use of VZIG has been recommended for immunosuppressed individuals, pregnant females, neonates, and health personnel. Children infected prenatal or postnatal have a very poor prognosis Varicella lesions are frequently seen in various stages: maculae on an erythematosus base and papule, clear filled vesicle. Lesions of all stages can be present at one time PNEUMOCOCCAL VACCINE- PCV-7 / PREVNAR 2, 4, 6, 12-15 months Ages: Route: IM Common side effects: Serious side effects: Soreness, redness, swelling at injection site. Mild-moderate fever, irritability. Anaphylaxis Contraindications: Hypersensitivity to diphtheria toxoid PNEUMOCOCCAL DISEASE Caused by streptococcus pneumoniae, a gram + bacteria. The organism is found in the pharynx of healthy people. Outbreaks occur in the winter and spring under crowded conditions. Most common in the 6 month- 2 year age group. S & S of disease are related to the focal area of infection. Pneumococcal disease can cause: OM, sinusitis, URI, Laryngotracheobronchitis, pneumonia, meningitis and bacteremia. Treatment of invasive pneumococcal disease PCN BUT up to 48% of infections are PCN resistant. Macrolide antibiotics (erythromycin, azithromycin and clairthromycin) or third generation cephalosporins (Cefotaxime or Ceftriaxone) Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 12 of 13 SCARLET FEVER Etiology: Mode of transmission: Incubation: Period of communicability: Potential complications: Group A- beta hemolytic strep Direct contact with droplets, contact with contaminated items, and ingestion of contaminated food/milk. 2-5 days During incubation period and illness (about 10 days) Otits media, peritonsillar and retropharyngeal abscess, sinusitis, Glomerulonephritis, Carditis Clinical manifestations of Scarlet Fever Enlarged edematous tonsils covered with exudate (in some cases looks like membrane seen in diphtheria). Beefy red pharynx, Day 1 & 2 tongue is coated (white) Day 4-5, white coating sloughs off leaving tongue/papillae prominent and “strawberry tongue” appears, palate is covered with lesions. Rash: appears within 12 hours of onset of fever, Red pin-sized lesions, generalized but absent on face, face becomes flushed with circumoral pallor. Rash more intense in folds of skin (elbows/knees) especially femoral region. At end of 1st week desquamation begins, fine sandpaper consistency with sloughing of skin on palms & soles. Can take up to 3 weeks for rash to resolve completely. Treatment: Penicillin (or erythromycin in allergic children) fever should disappear after 24 hours of antibiotic treatment. Respiratory precautions for 24 hours. Oral antibiotic for 10 days. Treat sore throat with analgesics, gargles, lozenges, and antiseptic throat spray. NURSING CONSIDERATIONS Respiratory precautions until 24 hours after initiation of antibiotics. Rest during febrile phase; push fluids during febrile stage. ERYTHEMA INFECTIOSUM /FIFTH’S DISEASE Etiology: Caused by human parvovirus B19 Mode of transmission: Unknown but believed to be spread by respiratory secretions and blood. Incubation: 4-14 days Period of communicability: During incubation period and illness (about 10 days) Potential complications: Uncertain, but before onset of symptoms and for about 1 week after onset of symptoms Chapter 10: Vaccines and Preventable Communicable Illnesses of Childhood, Page 13 of 13 Clinical Manifestations of Fifth's disease Rash that appears in 3 stages 1st- stageErythema of face “slapped cheek” rash, disappears in-4 days. 2nd stageAbout 1 day after rash appears on face, maculopapular red spots on upper & lower extremities. Progresses from proximal to distal and may last up to 1 week. 3rd stageRash is gone but will return if skin is irritated (heat/cold/sun/friction) Complications: self-limiting but can result in fetal death if mother is infected during pregnancy in the first half of pregnancy. (10% risk of fetal death).Aplastic crisis in children with hemolytic disease or immunodeficiency. Treatment: none, symptomatic use of Tylenol/Motrin, blood transfusions for kids with aplastic crisis. EXANTHEMA SUBITUM/ ROSEOLA Etiology: Human herpes virus type 6 (HHV-6) Mode of transmission: Unknown, almost exclusively in children 6 months-3 years. Incubation: 5-15 days Period of communicability: Unknown Potential complications: Recurrent febrile seizure, rare encephalitis Clinical manifestations: Persistent high fever for 3-4 days, child appears well, fever disappears with appearance of rash. Rash: discrete light- pink macules or maculopapules that appear on trunk spreads to neck, face and extremities. Fades with pressure, lasts 1-2 days See blackboard for additional documents on immunizations