Mental Illness and Suicide in Young People
advertisement

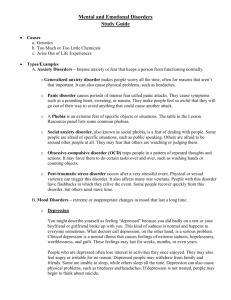
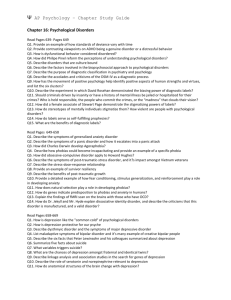
Fact Sheet Mental Illness & Suicide in Young People Mental illness has been identified as a leading factor in youth suicide. Therefore, youth who call crisis line staff with concerns and/or symptoms of mental illness are likely to be at increased risk for experiencing suicidal ideations and/or plans. Below are listed brief descriptions of some of the more common mental illnesses that young crisis line callers are known to experience. These include depression, bipolar disorder, attention-deficit/hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), schizophrenia, and posttraumatic stress disorder (PTSD). Finally, a general overview of anxiety disorders is presented. Recognizing signs and symptoms of mental illness during a crisis line call can help staff be better prepared to screen for suicidality in their young callers. Child/Adolescent Depression Depression has been identified as a leading cause of death by suicide. It is a brain disorder that affects the way young people think, feel, and act. It can lead to school failure, alcohol or other drug use, and suicide. Symptoms of childhood/adolescent depression are similar to adults. These include: Feeling sad, blue, (and/or irritability in children) Loss of interest in activities that are normally pleasurable Recent weight loss or gain Unreasonable feelings of self-reproach or guilt Recurrent thoughts of death or suicidal behaviors Diminished ability to concentrate and/or indecisiveness Change in activity level (increased agitation or slowing down) Sleep problems (interrupted sleep or oversleeping) Appetite change (decrease or increase) In addition to the depression symptoms that adult experience, adolescents often experience: Increased irritability or agitation, including angry outbursts Withdrawal from friends and from activities once enjoyed Missed school or poor school performance Frequent physical complaints, such as headaches and stomachaches Lack of enthusiasm, low energy, or low motivation Drug and/or alcohol abuse Statistics Depression is a leading cause of childhood/adolescent suicide. Fifty-seven percent (57%) of nearsuicides in children and adolescents have major depression as a diagnosis. Rates of major depression vary by age from less than 1% for ages 0-6 years; to 2-3% for ages 6-11 years; and 6-8% for ages 12-18 years. One in every 33 young children and one in eight teens suffer from depression. The rate of major depression is 2 to 3 times higher in adolescent females than males. While rates of major depression are similar for adolescent whites and blacks, black females tend to report higher levels of depression than white females. Once a young person has experienced a major depression, he or she is at risk of developing another depression within the next five years. One-third of children ages 6-12 diagnosed with major depression will develop bipolar disorder within a few years. Four out of five runaway youth suffer from depression. Youth who suffer with depression are often misdiagnosed with behavioral, social, and learning problems. Depression is often missed in children with attention deficit-hyperactivity disorders (ADHD) because the symptoms can be similar (mopey, whiney or irritable, angry, mood swings, withdrawal, lethargy, sleep disturbances, difficulty concentrating). Many children suffering from depression are thought to have learning disabilities since depression affects concentration and learning. Eating disorders are common in depressed youth and can exacerbate depression. Drinking and substance are a common element of depression in youth. Teens may resort to drugs in an effort to ease emotional pain. Treatment Youth who exhibit symptoms of depression should be referred to a mental health professional who specializes in treating children and teenagers. Although some young people may think depression will last forever, there is hope. Major depressive episodes in adolescents usually last from four to nine months. Often significant relief comes shortly after treatment begins. Treatment of major depression (medical and psychotherapy) is as effective for children as it is for adults. Bipolar Disorder Bipolar disorder, also known as manic-depressive disorder, is a brain disorder involving episodes of serious mania that are either preceded by or followed by an episode of depression. The person’s mood usually swings from overly "high" and irritable to sad and hopeless, and then back again, with periods of normal mood in-between. In adolescents, the cycling between mania and depression can be very rapid, occurring several times throughout the day. Such cycling is most often associated with low arousal states in the mornings followed by increases in energy towards late afternoon or evening. Symptoms include: Bipolar disorder usually begins in adolescence or early adulthood and continues throughout life. Extreme irritability and distractibility Excessive "high" or euphoric feelings A sustained period of behavior that is different from usual Increased energy, activity, fidgetiness, racing thoughts and rapid talking Being easily frustrated, having difficulty controlling anger, and impulsiveness Decreased need for sleep Unrealistic beliefs in one’s abilities and powers Uncharacteristically poor judgment Increased sexual drive in sexually mature adolescents and young adults Abuse of drugs, particularly cocaine, alcohol and sleeping medications Obnoxious, provocative or intrusive behavior Denial that anything is wrong Treatment The first line of treatment is to stabilize the child's mood (e.g., mood stabilizers such as lithium, Depakote) and to treat sleep disturbances and psychotic symptoms if present. Once the child is stable, therapy that helps him or her understand the nature of the illness and how it affects his or her emotions and behavior is a critical component of a comprehensive treatment plan. Attention-Deficit/Hyperactivity Disorder Attention-deficit/hyperactivity disorder (ADHD) is an illness characterized by inattention, hyperactivity, and impulsivity. The most commonly diagnosed behavior disorder in young persons, ADHD affects an estimated three to five percent of school-age children. Although ADHD is usually diagnosed in childhood, it is not a disorder limited to children-ADHD often persists into adolescence and adulthood and is frequently not diagnosed until later years. There several types of ADHD. Three of the more common types are listed below. Predominantly Inattentive Type: Fail to pay close attention to details or make careless mistakes in schoolwork, work, or other activities Have difficulty sustaining attention to tasks or leisure activities Do not seem to listen when spoken to directly Do not follow through on instructions and fail to finish schoolwork, chores, or duties in the workplace Have difficulty organizing tasks and activities Avoid, dislike, or are reluctant to engage in tasks that require sustained mental effort Lose things necessary for tasks or activities Are easily distracted by extraneous stimuli Are forgetful in daily activities Predominantly Hyperactive/Impulsive Type: Fidget with their hands or feet or squirm in their seat Leave their seat in situations in which remaining seated is expected Move excessively or feel restless during situations in which such behavior is inappropriate Have difficulty engaging in leisure activities quietly Are "on the go" or act as if "driven by a motor" Talk excessively Blurt out answers before questions have been completed Have difficulty awaiting their turn and interrupt or intrude on others Combined Type: Those with the combined type, the most common type of ADHD, have a combination of the inattentive and hyperactive/impulsive symptoms. Treatment Many treatments-some with good scientific basis, some without-have been recommended for individuals with ADHD. The most proven treatments are medication and behavioral therapy. Stimulants are the most widely used drugs for treating attention-deficit/ hyperactivity disorder. Antidepressants, major tranquilizers, and the antihypertensive clonidine (Catapres) have also proven helpful in some cases. Treatment strategies such as rewarding positive behavior changes and communicating clear expectations of those with ADHD have also proven effective. Obsessive-Compulsive Disorder (ODC) Obsessive-compulsive disorder is an anxiety disorder characterized by involuntary thoughts, ideas, urges, impulses, or worries that run through one’s mind (obsessions) and purposeless repetitive behaviors (compulsions). Approximately one million children and adolescents in the United States suffer from OCD. This can mean three to five youngsters with OCD per average-sized elementary school and about 20 teenagers in a large high school. The onset of OCD symptoms may occur as early as age three or four, but very young children and parents may not recognize the symptoms. Some of the most common obsessions are fear of contamination or a serious illness, fixation on lucky/unlucky numbers, fear of danger to self and others, need for symmetry or exactness, and excessive doubt. Some of the most common compulsions are repetitive rituals such as cleaning or washing, touching, counting, repeating, arranging or organizing, checking or questioning, and hoarding. Some children with OCD are too young to realize that their thoughts and actions are unusual. They may not understand or be unable to explain why they must go through their rituals. But older children may feel embarrassed--they don't want to be "different" from their peers and may worry that they are "going crazy". Fearing ridicule, children may hide their rituals when in front of friends at school or at home and become mentally exhausted from the strain. Other children find their rituals so time-consuming that they are too tired to play with friends or concentrate in school. Tension and discord between parents and a child with OCD may build when the child repeatedly demands answers to questions or wants help in completing their rituals. Treatment As in adults, standard treatment includes medication therapy, behavior therapy, or a combination of both. Drugs recommended for OCD are those that act upon the imbalance of serotonin. A physician should be contacted to recommend which particular medication is best suited for each specific case. Schizophrenia Schizophrenia is a brain disorder that affects approximately two percent of the population. Schizophrenia can affect anyone at any age, but most cases develop between adolescence and age 30. Young children can be affected by schizophrenia, but this is uncommon. Schizophrenia impairs a person’s ability to think clearly, manage his or her emotions, make decisions, and relate to others. The symptoms of schizophrenia are generally divided into three categories: positive symptoms, disorganized, negative symptoms. Positive Symptoms, or "psychotic" symptoms, include delusions and hallucinations because the patient has lost touch with reality in certain important ways. Delusions cause the patient to believe that people are reading their thoughts or plotting against them, that others are secretly monitoring and threatening them, or that they can control other people’s minds. Hallucinations cause people to hear or see things that are not there. Disorganized Symptoms include confused thinking and speech, and behavior that does not make sense. For example, people with schizophrenia sometimes have trouble communicating in coherent sentences or carrying on conversations with others; move more slowly, repeat rhythmic gestures or make movements such as walking in circles or pacing; and have difficulty making sense of everyday sights, sounds and feelings. Negative Symptoms include emotional flatness or lack of expression, an inability to start and follow through with activities, speech that is brief and lacks content, and a lack of pleasure or interest in life. "Negative" does not, therefore, refer to a person’s attitude, but to a lack of certain characteristics that should be there. Treatment Antipsychotic drugs are used in the treatment of schizophrenia. These medications help relieve the delusions, hallucinations, and thinking problems associated with this devastating disorder. Examples of conventional antipsychotics include: Prolixin, and Haldol. The newer, atypical antipsychotics have fewer side effects and include: Risperdal, Clozaril, Zyprexa, and Seroquel. Post-Traumatic Stress Disorder Posttraumatic stress disorder (PTSD) is an anxiety disorder that can occur following exposure to a traumatic event that caused intense fear, helplessness, or horror. PTSD can result from personally experienced traumas (e.g., rape, war, natural disasters, abuse, serious accidents, captivity) or from the witnessing or learning of a violent or tragic event. While it is common to experience a brief state of anxiety or depression after such occurrences, those with PTSD continually re-experience the traumatic event; avoid individuals, thoughts, or situations associated with the event; and exhibit symptoms of increased arousal. Those diagnosed with PTSD experience these symptoms for longer than one month and are unable to function as they did before the event. PTSD usually appears within three months of the traumatic experience, but in some circumstances can surface months or even years later. Studies suggest that anywhere between two percent and nine percent of the population has had a bout with PTSD. However, the likelihood of developing the disorder is increased by exposure to multiple traumas and traumas experienced early in life, especially if they are prolonged or repeated. Increased incidences of the disorder have also been found among inner-city youths and those recently immigrated from troubled countries. Additionally, women seem to get PTSD more frequently than men. Veterans are perhaps the community most associated with PTSD, or what was once referred to as "shell shock" or "battle fatigue." The Anxiety Disorders Association of America notes that an estimated 15 percent to 30 percent of the 3.5 million men and women who served in Vietnam have suffered from PTSD. It is important to note that those with PTSD often use alcohol or other drugs in an attempt to self-medicate. Individuals with this disorder may also be at an increased risk for suicide. Symptoms fall into three general categories: Re-experience: Individuals with PTSD often experience recurrent and intrusive recollections of and/or nightmares about the stressful event. Some may experience flashbacks, hallucinations, or other vivid feelings of the event happening again. Others experience great psychological or physiological distress when certain things (objects, situations, etc.) remind them of the event. Avoidance: Many with PTSD will persistently avoid things that remind them of the traumatic event. This can result in avoiding everything from thoughts, feelings, or conversations associated with the incident to activities, places, or people that cause them to recall the event. In others there may be a general lack of responsiveness signaled by an inability to recall aspects of the trauma, a decreased interest in formerly important activities, a feeling of detachment from others, a limited range of emotion, and/or feelings of hopelessness about the future. Increased arousal: Symptoms in this area may include difficulty falling or staying asleep, irritability or outbursts of anger, difficulty concentrating, becoming very alert or watchful, and/or jumpiness or being easily startled. Treatment PTSD can be treated effectively with psychotherapy and/or medication. Behavior therapy focuses on the development of relaxation and coping techniques. This form of therapy can involve a gradually increasing exposure to a feared situation in an attempt to decrease one's sensitivity. Alternatively, cognitive therapy is designed to help an individual examine his or her thought patterns and learn to combat negative and nonproductive thinking. Group therapy has also proven helpful for many with PTSD by allowing them to interact with others in similar situations and learn that their fears and feelings are not uncommon. Medication is often used as an adjunct to psychotherapy. Antidepressant and anti-anxiety drugs can be helpful in reducing symptoms of PTSD such as sleep problems (insomnia, nightmares), depression, and edginess. Anxiety Disorders Anxiety disorders cause people to feel excessively frightened, distressed, and uneasy during situations in which most others would not experience these symptoms. Anxiety disorders in children can lead to poor school attendance, low self-esteem, deficient interpersonal skills, alcohol abuse, and adjustment difficulty. Anxiety disorders are the most common mental illnesses affecting one in 10 young people. Unfortunately, these disorders are often difficult to recognize, and many who suffer from them are either too ashamed to seek help or they fail to realize that these disorders can be treated effectively. Most Common Anxiety Disorders Panic Disorder -- Characterized by panic attacks, panic disorder results in sudden feelings of terror that strike repeatedly and without warning. Physical symptoms include chest pain, heart palpitations, shortness of breath, dizziness, abdominal discomfort, feelings of unreality, and fear of dying. Children and adolescents with this disorder may experience unrealistic worry, self- consciousness, and tension. Obsessive-compulsive Disorder (OCD) -- see above -- OCD is characterized by repeated, intrusive, and unwanted thoughts (obsessions) and/or rituals that seem impossible to control (compulsions). Adolescents may be aware that their symptoms don’t make sense and are excessive, but younger children may be distressed only when they are prevented from carrying out their compulsive habits. Compulsive behaviors often include counting, arranging and rearranging objects, and excessive hand washing. Post-traumatic Stress Disorder -- Persistent symptoms of this disorder occur after experiencing a trauma such as abuse, natural disasters, or extreme violence. Symptoms include nightmares; flashbacks; the numbing of emotions; depression; feeling angry, irritable, and distracted; and being easily startled. Phobias -- A phobia is a disabling and irrational fear of something that really poses little or no actual danger. The fear leads to avoidance of objects or situations and can cause extreme feelings of terror, dread, and panic, which can substantially restrict one’s life. "Specific" phobias center on particular objects (e.g., certain animals) or situations (e.g., heights or enclosed spaces). Common symptoms for children and adolescents with "social" phobia are hypersensitivity to criticism, difficulty being assertive and low self-esteem. Generalized Anxiety Disorder -- Chronic, exaggerated worry about everyday, routine life events and activities that lasts at least six months is indicative of generalized anxiety disorder. Children and adolescents with this disorder usually anticipate the worst and often complain of fatigue, tension, headaches, and nausea. Other recognized anxiety disorders include: agoraphobia, acute stress disorder, anxiety disorder due to medical conditions (such as thyroid abnormalities), and substance-induced anxiety disorder (such as from too much caffeine). Treatment Effective treatments for anxiety disorders include medication, specific forms of psychotherapy (known as behavioral therapy and cognitive-behavioral therapy), family therapy, or a combination of these. Cognitivebehavioral treatment involves the young person’s learning to deal with his or her fears by modifying the way he or she thinks and behaves by practicing new behaviors. The mission of MHA Indy is to advance mental health across all communities in Greater Indianapolis through education, advocacy, and intervention. 317-251-0005 (office) 24-hour Crisis Hotline 317-251-7575, 1-800-273-TALK, or Text ‘CSIS’ to 839863 www.mhaindy.net