Customizable Protocol
advertisement

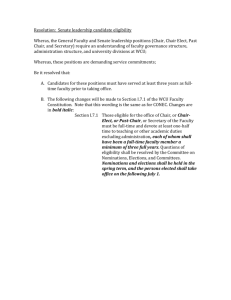
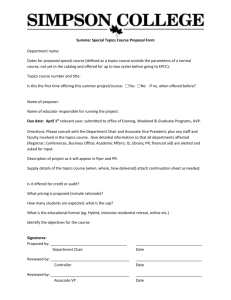
Prevalon® Seated Positioning System (SPS) Protocol Authors: Kathleen M Vollman MSN, RN, CCNS, FCCM, FAAN, Clinical Nurse Specialist, Educator, Consultant, ADVANCING NURSING LLC; Suzanne Harrington MS, PT, ATC, Assistant Physical Therapy Director, Cook County Hospital, Chicago, IL Natalie S. McAndrew, MSN, RN, CCRN, ACNS-BC, Clinical Nurse Specialist - Medical Intensive Care Unit, Froedtert Hospital, Milwaukee, WI Kathy Krenz BS, RN, CWOCN, APN, Wound Ostomy Continence Nurse, Centegra McHenry Hospital, McHenry IL Procedure: Prevalon® Seated Positioning System with Microclimate Management Pad Purpose: The purpose of the Prevalon® Seated Positioning System with Microclimate Management Pad is to help the caregiver achieve these goals: Redistribute pressure to protect patients’ skin Promote easier breathing, swallowing through better posture Microclimate management to reduce the risk of moisture related skin injury. Help prevent skin shear and friction Help prevent caregiver injury during repositioning Help prevent patients from inadvertently sliding forward in the chair The system is designed to provide easy patient manipulation within a chair to help achieve maximal comfort, pressure redistribution, position shifting and reduced shear and friction forces while minimizing the physical effort required for repositioning by caregivers, thus reducing the risk of injury to the patient and caregiver. Independent Indications for use: 1. 2. 3. 4. 5. 6. 7. Braden friction/shear subscale score of 1. Incontinence of urine or stool and or a Braden moisture subscale score of 2 or less. Mobility subscale of 1 when in combination with a low moisture or friction/shear subscale scores. Sensory/Perceptual subscale score of 2 or less. Pre-existing sacral pressure ulcer. Unable to achieve a sustained chair position related to comfort or lack of posture control. Chair use after remaining in bed for >3days. Cautions: 1. 2. 3. 4. 5. 6. 7. 8. Only use with standard hospital chair or rolling chair with brakes. DO NOT use Prevalon® Seated Positioning System to lift patients. Avoid direct skin contact with gray surface for hygiene purposes. Patient repositioning should be performed following your facility’s safe patient handling policies and procedures. For single patient use only. If soiled, wipe cushion with a damp cloth to clean. Periodically check product for signs of wear. Replace if product is damaged. Weight capacity: 350 lbs./160 kg. for Prevalon® Seated Positioning System. Contraindications: 1. 2. The presence of ischial pressure ulcers. Inability/medical restriction to sitting up in a chair at 90 degrees. Discontinue use: 1. When patient is able to independently mobilize. References: 1. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: clinical practice guideline. Washington D.C. National Pressure Ulcer Advisory Panel;2009. 2. Institute for health care improvement: Prevent pressure ulcers. http://www.ihi.org/IHI/Programs/Campaign/PressureUlcers.htm. Accessed October 7th, 2007 3. Courtney BA, Ruppman JB, Cooper HM. Save our skin: Initiative cuts pressure ulcer incidence in half. Nursing Management. 2006;37(4):35-46. 4. Driver DS. Perineal dermatitis in critical care patients. Critical Care Nurse 2007;27(4):42-46. 5. Gould D, James T, Tarpey A, et al. Intervention studies to reduce the prevalence and incidence of pressure sores: a literature review. J Clin Nurs, 2000;9(2):163-177. 6. Bergstrom N, Braden B, Kemp M, Champagne M, Rudy E. Predicting pressure ulcer risk: A multisite study of the predictive validity of the Braden scale. Nursing Research, 1998;47(5):261-269 7. Black J, Baharestani M, Cuddigan J, et al. National Pressure Ulcer Advisory Panel’s Updated Pressure Ulcer Staging System. Derm Nurs. 2007;19(4):343–350. 8. Gray M, Weir D. Prevention and treatment of moisture-associated skin damage (maceration) in the periwound skin. J WOCN. 2007;34(2):153–157. 9. Vollman KM. Ventilator-associated pneumonia and pressure ulcer prevention as targets for quality improvement in the ICU. Critical Care Nursing Clinics of North America, 2006;18:453-467 10. Warner D, Konnerth K, (1993). “A patient teaching protocol for pressure ulcers prevention and management” Ostomy and Wound Management, 39 (2): 35-43 Procedure: Prevalon® Seated Positioning System with Microclimate Management Pad Wash hands Ensure privacy for the patient Steps 1. 2. Rationale Product Setup: Position chair with space behind for clinician(s) access Make sure chair brakes are locked. To help ensure safety of the caregiver during the transfer process. To help ensure safety of the patient and caregiver during the transfer process. 3. Remove the SPS from plastic packaging, unfold and place on chair seat with cushion directly against chair seating surface. 4. Place cushion so product tag is to the back of chair, tuck cushion into crease in chair. If cushion is not placed properly, its ability to both relieve pressure and allow for proper patient repositioning will be adversely affected. Drape straps over each side of the chair so that they are both visible and accessible. DO NOT allow patient to sit on straps. Ensures safety of patient. 5. Face Up Face Down Cushion facilitates pressure redistribution, shear/friction reduction & helps protect clinicians throughout the chair repositioning process Special Considerations 6. 7. 8. Cover SPS with enclosed Microclimate Management Pad. a. Do not allow the top layer of the cushion to slide backwards on the chair surface during this process. The microclimate management pad is designed for optimal heat and moisture control under the patient. Alternative materials, while compatible with the device, may not be as effective at moisture management or microclimate control. Patient Positioning: Clinicians must have access either behind or on both sides of bedside chair for this technique a. With patient safely seated, stand behind chair and grasp handle at nearest comfortable location. b. Brace a foot or leg on the back of the chair for support. c. Simultaneously pull handles until the patient slides back into chair, in the upright seated position. d. Secure handles behind chair so they are safely out of the way. Proper patient positioning with this device will shift pressure away from the sacrum and onto the larger surface area of the buttocks. When patient is ready to return to bed, the SPS can be used to help move the patient toward the edge of the chair in preparation for the transfer process. a. From front of chair, grasp both straps at the most comfortable handle location. b. Pull each strap in an alternating manner Allows clinician to help shift the patient’s base of support forward to help facilitate safe transfer. Caregiver access from the rear or sides of the chair will allow the clinicians to assume a good body position to help minimize the risk of musculoskeletal injury Place a pillow against the chair back if needed. (Left-right-left, etc.) until patient is positioned safely toward front of chair c. Transfer patient to bed per your facility’s protocol. 9. Storage and Cleaning a. Wipe with damp cloth to clean. b. Store SPS in a clean, dry location within patient room © Advancing Nursing LLC, 2013 21895 The only changeable component of the system is the Microclimate Pad