Objectives 37 - U
advertisement
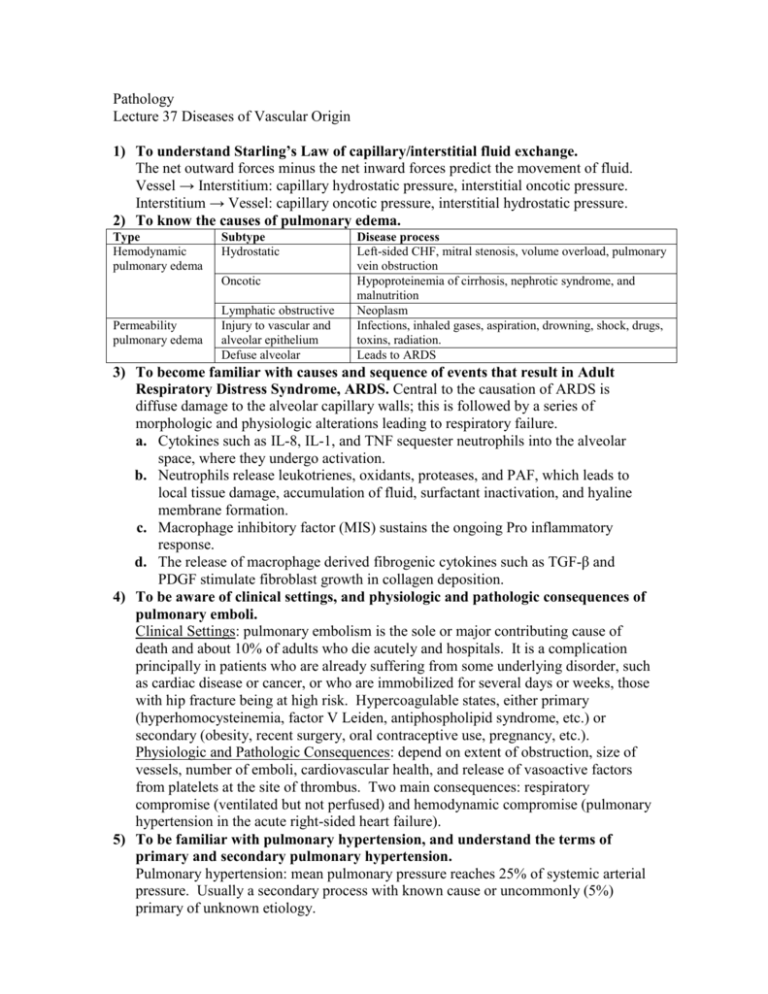
Pathology Lecture 37 Diseases of Vascular Origin 1) To understand Starling’s Law of capillary/interstitial fluid exchange. The net outward forces minus the net inward forces predict the movement of fluid. Vessel → Interstitium: capillary hydrostatic pressure, interstitial oncotic pressure. Interstitium → Vessel: capillary oncotic pressure, interstitial hydrostatic pressure. 2) To know the causes of pulmonary edema. Type Hemodynamic pulmonary edema Subtype Hydrostatic Oncotic Permeability pulmonary edema Lymphatic obstructive Injury to vascular and alveolar epithelium Defuse alveolar Disease process Left-sided CHF, mitral stenosis, volume overload, pulmonary vein obstruction Hypoproteinemia of cirrhosis, nephrotic syndrome, and malnutrition Neoplasm Infections, inhaled gases, aspiration, drowning, shock, drugs, toxins, radiation. Leads to ARDS 3) To become familiar with causes and sequence of events that result in Adult Respiratory Distress Syndrome, ARDS. Central to the causation of ARDS is diffuse damage to the alveolar capillary walls; this is followed by a series of morphologic and physiologic alterations leading to respiratory failure. a. Cytokines such as IL-8, IL-1, and TNF sequester neutrophils into the alveolar space, where they undergo activation. b. Neutrophils release leukotrienes, oxidants, proteases, and PAF, which leads to local tissue damage, accumulation of fluid, surfactant inactivation, and hyaline membrane formation. c. Macrophage inhibitory factor (MIS) sustains the ongoing Pro inflammatory response. d. The release of macrophage derived fibrogenic cytokines such as TGF-β and PDGF stimulate fibroblast growth in collagen deposition. 4) To be aware of clinical settings, and physiologic and pathologic consequences of pulmonary emboli. Clinical Settings: pulmonary embolism is the sole or major contributing cause of death and about 10% of adults who die acutely and hospitals. It is a complication principally in patients who are already suffering from some underlying disorder, such as cardiac disease or cancer, or who are immobilized for several days or weeks, those with hip fracture being at high risk. Hypercoagulable states, either primary (hyperhomocysteinemia, factor V Leiden, antiphospholipid syndrome, etc.) or secondary (obesity, recent surgery, oral contraceptive use, pregnancy, etc.). Physiologic and Pathologic Consequences: depend on extent of obstruction, size of vessels, number of emboli, cardiovascular health, and release of vasoactive factors from platelets at the site of thrombus. Two main consequences: respiratory compromise (ventilated but not perfused) and hemodynamic compromise (pulmonary hypertension in the acute right-sided heart failure). 5) To be familiar with pulmonary hypertension, and understand the terms of primary and secondary pulmonary hypertension. Pulmonary hypertension: mean pulmonary pressure reaches 25% of systemic arterial pressure. Usually a secondary process with known cause or uncommonly (5%) primary of unknown etiology. 6) To be aware of the disease Wegener’s granulomatosis. Wegener 's granulomatosis is an immunologically mediated disease were anti-neutrophil cytoplasmic antibodies (ANCA) in serum correlate with disease activity and may protect proteases from inactivation by binding to their natural inhibitors. It presents as nodular densities on chest x-ray, hemoptysis, chest pain, fever, dyspnea, chronic sinusitis, and evidence of renal disease. Acute necrotizing granulomas of upper respiratory tract and lungs, focal necrotizing vasculitis of lungs, and necrotizing glomerulitis. 7) To answer all questions posed in the Directed Reading. 1. According to Starling’s Law of capillary interstitial fluid exchange, which forces move fluid out of the vessel into the interstitial space, and which forces move fluid from the interstitial space into the vessel? Vessel → Interstitium: capillary hydrostatic pressure, interstitial oncotic pressure Interstitium → Vessel: capillary oncotic pressure, interstitial hydrostatic pressure 2. Name the most common hemodynamic cause of pulmonary edema, and three other causes. Hydrostatic (left-sided CHF). Other causes: mitral stenosis, volume overload, pulmonary vein obstruction. 3. Describe the histologic appearance of pulmonary edema. Alveolar capillaries are engorged, and an intra-alveolar granular pink precipitate is seen. Alveolar microhemorrhages and hemosiderin-laden macrophages ("heart failure" cells) may be present. 4. In long-standing pulmonary congestion, which cells are responsible for the brown discoloration of the lungs? Hemosiderin-laden macrophages. 5. What is the initial injury in course of events which lead to ARDS? Diffuse alveolar capillary damage. 6. What is the most common source of pulmonary thromboemboli? 95% rise from deep veins of the legs and pelvis. 7. What is the mechanism of sudden death associated with large pulmonary emboli such as saddle emboli? Sudden-death, right heart failure (cor pulmonale), or cardiovascular collapse occurs with 60% or more of the pulmonary circulation is obstructed with emboli. 8. Describe the gross histologic appearances of an acute pulmonary infarct. Acute pulmonary infarcts extend to the periphery of the lung substance as a wedge with the apex pointing toward the hilus of the lung. It is classically hemorrhagic and appears as a raised, red-blue area in the early stages. The opposed pleural surface is covered by a fibrinous exudate the red cells begin to lyse within 48 hours, and the infarct becomes paler and eventually red-brown as hemosiderin is produced. Fibrous replacement begins at the margins as graywhite peripheral zone and eventually converts the infarct to a contracted scar. 9. What two factors determine the clinical significance of pulmonary infarct? The size of the embolic mass and the general state of the circulation. 10. What substances other than thrombi may embolize to the lung? Air, bone marrow (after trauma and bone marrow necrosis in sickle cell patients), fat (trauma and surgery), amniotic fluid (during parturition), and foreign bodies (in IV drug abusers). 11. Name at least one cause of secondary pulmonary hypertension that act by each of the following mechanisms? a) Increased pulmonary blood flow: left to right shunt associated with congenital heart disease. b) Increased resistance: vasospasm, mechanical obstruction, and destruction of vascular bed. c) increased pulmonary venous pressure: left heart failure, acquired heart diseases, mitral stenosis. 12. What mechanism is currently thought to cause primary pulmonary hypertension? Molecular studies have shown mutation in bone morphogenic protein receptor type 2 gene (BMPR2) in 50% of familial and 26% of sporadic cases. Normal BMPR2 signaling causes inhibition of proliferation and favors apoptosis of vascular smooth muscle. Loss of signaling promotes proliferation. Additional genetic or environmental insults are required to produce disease. 13. What changes are seen in the main elastic pulmonary arteries with pulmonary hypertension? Presence of many organizing or recanalized thrombi favors recurrent pulmonary emboli as the cause, and the coexistence of diffuse pulmonary fibrosis, or severe emphysema and chronic bronchitis, points to chronic hypoxia as the initiating event. 14. In which form of pulmonary hypertension are plexiform arterial lesions present? Plexogenic pulmonary arteriopathy occurs in primary pulmonary hypertension or congenital heart disease with left to right shunts, the name comes from a tuft of capillary formations producing a network, or Web, that spans the lumens of dilated thin walled, small, arteries. 15. What is Wegener's granulomatosis? An autoimmune disease most often involving the upper respiratory tract and/or the lungs, with hemoptysis being the most common presenting symptom. 16. What organs are involved in Goodpasture syndrome? The kidneys and the lungs.