This is a 36 years old female patient
advertisement
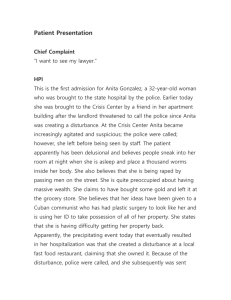
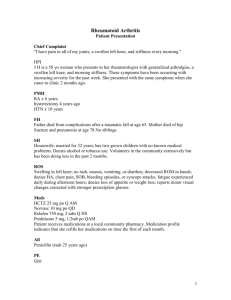
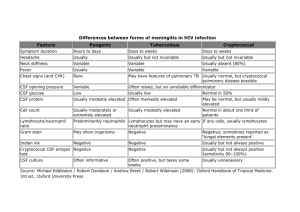
感染科 範例一 Dengue fever This is a 36-year-old woman who had generally been in her usual state of heath without any systemic disease. She is a housewife. At this time, she visited the Emergency Department of Chi Mei Medical Center with a chief complaint of fever with skin rashes for five days on 19 May 2009. The patient also complained general malaise, retro-orbital pain, pruritus, headache, abdominal pain, and arthralgia. Many maculopapular rashes were developed on her four limbs first, then to the trunk gradually. There was no petechiae, no shortness of breath, no palpitation, no cyanosis. There is no travel history. She recalled a mosquito bite three days earlier. She lives in Annan district of Tainan city. On physical examination, her blood pressure was 112/70 mm Hg; body temperature, 38.6℃; pulse, 112 beat/minute; respiration, 18/minute. Blood tests showed a WBC count of 2,000μm/mm3 with 76% segmented forms, 11% lymphocytes, and 8% monocytes; a RBC count of 4.53 x106μm/mm3; hemoglobin of 14.2 g/dL; platelet counts of 80,000 μm/mm3; hematocrit of 44.6 %. Biochemical tests revealed a sodium level of 140.7 mEq/L; potassium of 3.36 mEq/L; aspartate aminotransferase (AST or GOT) of 18 IU/L; analine aminotransferase (ALT or GPT) of 14 IU/L. Electrocardiogram (EKG) showed sinus tachycardia. Chest film was normal. Tourniquet test was negative. The patient was admitted to the Infection unit for further evaluation and management. 感染科 範例二 Meningitis This is a 66 years old man who has significant underlying diseases as follows: 1) Diabetes mellitus type 2 routinely treated with oral hypoglycemic agents (OHA) for 20 years; 2) hypertension routinely treated for 13 years. The patient, a retired farmer, was brought to the Emergency Department of Chi Mei Medical Center with a chief complaint of fever with headache and progressive alteration of consciousness for five days. His wife stated that her husband had got a common cold presenting with productive cough and rhinorrhea a week earlier, and also been troubled with throbbing headache, nausea, and photophobia. Most of time, the patient stayed in bed and was seemingly lethargic. On examination, his blood pressure was 140/78 mm Hg; temperature, 38.4℃; pulse, 110 beat/minute; respiration, 16/minute. On neurologic examination, Kernig’s and Brudzinski’s signs were negative. His neck was stiff. Fundoscopy showed the presence of papilledema. Brain computed tomography (CT) scan revealed no intracranial hemorrhage and no occupying lesion. Blood tests showed a white blood cell (WBC) count of 14,200μm/mm3 with 80% segmented forms, 11% lymphocytes, and 2% monocytes; a red blood cells (RBC) count of 3.51 106μm/mm3; hemoglobin of 15.5 g/dL; platelet counts of 330,000μm. Biochemical tests were as follows: C-reactive protein (CRP), 78 mg/L; fasting glucose, 224 mg/dL; sodium, 135.5 mEq/L; potassium, 3.78 mEq/L; blood urea nitrogen (BUN), 12 mg /dL; creatinine, 1.3 mg/dL; aspartate aminotransferase (AST or GOT), 34 IU/L; analine transferases (ALT or GPT), 12 IU/L. Roentgenogram showed the presence of increased infiltration over bilateral lung fields. Electrocardiogram (EKG) showed sinus tachycardia. Two samples of blood were drawn for culture. Lumbar puncture was performed for cerebral spinal fluid analysis, and the results were as below: opening pressure, 22 cm H20; appearance, cloudy; color, yellowish; RBCs, 760 /mm3; WBCs, 1,632/mm 3; lymphocytes, 3%; neutrophils, 97%; total protein, > 500 mg/dL; glucose, 118 mg/dL; Gram stain, Gram-negative bacilli 3+; acid-fast stain, negative; India ink stain, negative; fungal stain, negative; VDRL, non-reactive; and cryptococcal antigen, negative. The patient was admitted to the Infection unit for further evaluation and management. 感染科 範例三 Necrotizing fasciitis This 46 year-old man was brought to the Emergency Department of Chi Mei Medical Center with a chief complaint of rapid swelling and pain in his right hand. He has alcoholic liver cirrhosis, but has not been treated regularly. He works as a deliveryman. The day before arrival at the ER, he went fishing at the nearby seashore. During that time, his right-hand finger was accidentally stabbed with a fish fin. His ipsilateral hand and arm then developed a rapidly enlarging swelling, accompanied with reddish change of his right hand from distal to proximal and purple hemorrhagic bullae. He did not complain of fever, chills, diarrhea or abdominal pain but had shortness of breath and palpitation. He was brought to our emergency department by his friend. On physical examination, blood pressure was 90/45 mm Hg; temperature, 35.6℃; pulse, 110 beats/minute; and respiration, 19 breaths/minute. The patient looked like he was suffering from excruciating pain. His right hand was warm, swollen, and red, with three hemorrhagic bullae and crepitus. Blood tests showed a white cell counts (WBCs) of 14,800/mm3 with 3% band forms, 80% segmented cells, 11% lymphocytes, and 2% monocytes; a red blood cells (RBCs) counts of 4.53×106 /mm3; hemoglobin of 14.5 g/dL; platelets of 230, 1000/mm3. Biochemical tests revealed a C-reactive protein level of 13.3 mg/L; a fasting glucose of 225 mg/dL; sodium of 127.5 mEq/L; potassium of 3.78 mEq/L; BUN of 9 mg /dL; creatinine of 0.8 mg/dL; aspartate aminotransferase (AST or GOT) of 114 IU/L; analine aminotransferase (ALT or GPT) of 94 IU/L. Chest film was essentially negative. Electrocardiogram revealed sinus tachycardia. X-ray of the right hand showed the presence of numerous gases inside the soft tissues. Two samples of blood were drawn for bacterial culture. The patient was treated with emergency fasciotomy two hours after arrival at ED; after that, he was admitted to the Infection unit for further evaluation and management.