A histopathologic study of arthropod bite reactions in 20 patients
advertisement
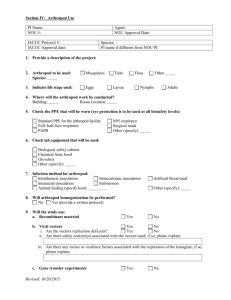
A histopathologic study of arthropod bite reactions in 20 patients highlights relevant adnexal involvement Maria Miteva 1 , Peter Elsner 1 Mirjana Ziemer 1 1 Department of Dermatology, Friedrich-Schiller-University, Jena, Germany Correspondence to Mirjana Ziemer, MD, Department of Dermatology and Allergology, Friedrich-Schiller-University. Erfurter Strasse 35, 07743 Jena, Germany Tel: +493641937441 Fax: +493641937423 e-mail: mirjana.ziemer@derma.uni-jena.de Copyright © 2008 John Wiley & Sons A/S Miteva M, Elsner P, Ziemer M. A histopathologic study of arthropod bite reactions in 20 patients highlights relevant adnexal involvement. J Cutan Pathol 2009; 36: 26–33. © 2008 John Wiley & Sons A/S. ABSTRACT Background: Insect bites produce diverse skin reactions. Although quite common, the histopathologic features of arthropod assaults have not ever been studied systemically. Materials and methods: Twenty biopsies from cases, clinically diagnosed as arthropod bite reactions between January 2003 and June 2007 were reviewed retrospectively. The aim of the study was to verify as to whether reliable histopathologic criteria could be established based on the frequency of findings observed. Results: Epidermal spongiosis (present in 16 of 20 cases), in particular spongiosis of the infundibular epithelium and acrosyringia as well as eosinophilic spongiosis, emerge as relevant diagnostic clues. A moderately dense, superficial and deep infiltrate consisting mainly of lymphocytes and eosinophils was prevalent in the dermis, with eosinophils tending to interstitial and periadnexal distribution. Of note, 19 of 20 (95%) cases revealed periadnexal involvement, whereas 16 of 20 (80%) had the infiltrate extending particularly along the sweat ducts and the coiled glands. In three biopsies, concomitant involvement of sweat glands, hair follicles and sebaceous glands was noted. Conclusion: A practical histopathologic algorithm of arthropod bite recognition is proposed. The involvement of the sweat glands in the pattern of arthropod bite reaction is suggested as a new reliable diagnostic clue. Accepted for publication January 2, 2008 DIGITAL OBJECT IDENTIFIER (DOI) 10.1111/j.1600-0560.2008.00992.x About DOI Article Text Insect bites and stings to humans are relative common events. Four principal arthropod classes can be differentiated, i.e. Crustacea (shrimps, prawns, crabs and lobsters), Myriapoda (centipedes, millipedes), Arachnida (spiders, ticks, scorpions) and Insecta (flies, mosquitoes, midges, beetles, fleas, bugs, wasps, bees, ants, cockroaches, etc.).1,2 However, apart from ticks, assaults by insects in particular by mosquitoes, fleas, and bugs as well as wasps, and bees are most commonly encountered within our latitudes. However, bee and wasp stings are rarely biopsied as they hardly ever raise diagnostic difficulties. Various cutaneous lesions (maculae, urticae, papules, vesicles, pustules, bullae, nodules, erosions and excoriations) could be observed in response to insect bites.3,4 As these reactions are not highly specific for a particular arthropod and vary from one person to another,5 the distinction from other cutaneous diseases might be difficult based on clinical grounds alone. Hence, a histologic examination may be of diagnostic help. However, the histopathology of insect bites may also vary significantly as it depends on many factors, such as the nature of the arthropod, the duration of the lesion, the immunological reaction, the presence of arthropod parts and the discharge of toxins.3,6 Therefore, a unifying concept of the most relevant histomorphologic phenomena is hardly realistic. The histopathologic features of arthropod reactions are insufficiently documented and have not been studied systemically. Descriptions in textbooks are brief, further not congruent3,4,6–8 (Table 1). Table 1. Histopathologic findings in arthopod bite reactions retrieved from textbooks References Histopathologic findings Ackerman et Early al. 3,7 Wedge-shaped perivascular (lymphocytes and eosinophils) and interstitial infiltrate (of scattered eosinophils), a few neutrophils may be discernible Slight edema of the papillary dermis (A discrete) focus of spongiosis at the very site of the bite, directly above the apex of the wedge infiltrate Spongiotic infundibulitis in the center of the wedge-shaped infiltrate Fully developed Denser and deep inflammatory infiltrate; the subcutaneous fat may be affected More marked edema and spongiosis (multiloculated vesicles, becoming smaller the farther they are) Late 8 Elder et al. Erosion, ulceration or crust likely to occur, secondary to scratching Mosquitoes Many neutrophils during the early toxic response and a mononuclear infiltrate of lymphoid cells and plasma cells during the later response; lack of eosinophils or few of them present In papular urticaria Edema and spongiosis in stratum malpighii Kerl et al.4 Inflammatory infiltrate around the vessels of the dermis, extending into the lower dermis (containing eosinophils) Superficial and deep, perivascular and interstitial infiltrate (lymphocytes and eosinophils) Wedge-shaped form of the infiltrate Focal spongiosis (with vesicles, becoming smaller the farther they are) The spongiosis is mostly pronounced directly above the apex of the wedge infiltrate Weedon et al.6 Edema in the papillary dermis In papular urticaria Edema in the papillary dermis Superficial and deep infiltrate with perivascular accentuation and usually some interstitial eosinophils Neutrophils in the early biopsies lesion (especially in flea bites) In persistent insect bites – plasma cells may be prominent, particularly in the deep dermis; pseudoepitheliomatous hyperplasia; atypical dermal infiltrates Focal epidermal necrosis is possible Besides, there is a lack of evidence-based data in the literature, dealing with the particular nature of the infiltrate in arthropod bites. To our knowledge, there is only one study aimed at the evaluation of morphologic and immunohistochemical properties of the lesions in papular urticaria (a kind of reaction to certain bites).9 However, the immediate aim of that study was rather to analyze the phenotype of the infiltrate and the role of the type I hypersensitivity reaction in the pathogenesis of papular urticaria, than to evaluate the main characteristics of its histopathologic pattern. This is the first study aimed at investigating the particular histomorphological features in arthropod bite lesions. Several previous studies have been focused on the histologic hallmarks in biopsies of patients who experienced assaults by particular arthropods, such as fleas,10 ticks and mites,11–16 sea urchins17 and spiders.18 Others have studied the predominant morphologic changes caused by insect bites, yet only in particular populations such as patients with concomitant neoplasms,19–21 positive for the human immunodeficiency virus 22 or with various other diseases.23 Series of biopsies obtained from patients with a clinical presentation of arthropod assaults (mosquitoes, fleas, bugs and ticks) who passed through our department recently, histologically revealed a mixed infiltrate with special predilection to the adnexal structures. On this empirical basis, we assumed that the involvement of the adnexa is a rather 'natural phenomenon' than a casual finding in cutaneous reactions to arthropod bites, a fact previously vaguely reported. We reinvestigated 20 biopsy specimens diagnosed clinically and pathologically as insect bite reactions. The aim of the study was to verify and update the morphologic criteria established as well as to specify new helpful clues. Materials and methods Twenty-one biopsy specimens obtained from 21 patients diagnosed clinically and histologically with arthropod bite reactions between January 2003 and June 2007 were studied. One biopsy was discarded because only superficial epidermal substrate was present, thus realizing a total of 20 biopsies. Clinical data were retrieved from the file register of the Department of Dermatology (Friedrich-Schiller-University, Jena, Germany). Special attention was paid to patient's age, sex, complete medical history, clinical symptoms and morphology of the lesions. The biopsy specimens comprised 4- to 6-mm punch biopsies (n = 14) and excisional biopsies (n = 6). They had been fixed in 4% buffered formalin and processed further according to the routine methods. A mean number of 3 sections stained with hematoxylin and eosin were examined in all cases. To assess the specificity of criteria for histopathologic diagnosis of arthropod reactions and to achieve compelling results, only cases with a documented clinical presentation of an arthropod assault (Figs. 1a and 2a) were included. Furthermore, we employed a provisional set of criteria to allow for the thorough evaluation of the samples including the already established morphologic criteria for insect bite reactions (Table 1). All slides were studied for the presence of the following features. Fig. 1. 1A) Urticarial papules on erythematous ground are distributed in a random pattern on the trunk. This clinical manifestation is consistent with an arthropod-bite reaction. 1B and 1C (from patient on figure 1A). A moderately dense, superficial and deep, perivascular, periadnexal and interstitial infiltrate composed of lymphocytes and eosinophils (hematoxylin and eosin; 1B, original magnification ×40; 1C, original magnification ×200). [Normal View ] Fig. 2. 2A) Urticarial papules on erythematous ground are distributed in a random pattern on the trunk. This clinical manifestation is consistent with an arthropod-bite reaction. 2B, 2C (from patient on figure 2A). A moderately dense, superficial and deep, perivascular, periadnexal and interstitial infiltrate composed of lymphocytes and eosinophils (hematoxylin and eosin; 2B, original magnification ×40; 2C, original magnification ×200). [Normal View ] 1. Epidermal changes: presence of crust, erosion/ulceration, ortho/hyperkeratosis, parakeratosis, acanthosis, lichen simplex chronicus-like-features (concomitant presence of acanthosis, hypergranulosis and hyperorthokeratosis) and spongiosis. 2. Spongiosis of follicular infundibula and acrosyringia. 3. Edema in the papillary dermis. 4. Cell composition, density, depth and distribution of the inflammatory infiltrate. 5. Wedge-shaped form of the infiltrate, defined as V-shaped arrangement of the inflammatory cells in the dermis with the apex toward the subcutaneous fat and a focus of spongiosis/erosion/crust situated directly above the apex of the wedge. 6. Flame figures (clusters of eosinophils around bundles of degenerated collagen). 7. Extravasations of erythrocytes. 8. Signs of vasculitis. Statistical analysis was carried out on a descriptive and analytical basis. Results The sample consisted of biopsies obtained from 12 men and 8 women, with a mean age of 51 years (range 4–89 years). The histopathologic features observed are summarized in detail in Table 2. Table 2. Evaluated histopathologic features Histopathologic features Epidermal changes Number of biopsies (%) Spongiosis 18 (90) Within the epidermis 16 (80) Spongiotic infundibulitis/spongiotic acrosyringitis 15 (75) Epidermal and adnexal 5 (25) Accompanied by vesicles/vesiculopustules 4 (20) Eosinophilic spongiosis 3 (15) Erosion/ulceration 5 (25) Scale-crust with neutrophils 7 (35) Mild acanthosis 7 (35) Ortho/hyperkeratosis 9 (40) Focal parakeratosis 6 (30) LS-like features 7 (35) Dermal changes Subepidermal edema 7 (35) Inflammatory infiltrate 20 (100) Components of the infiltrate Lymphocytes 20 (100) Eosinophils 20 (100) Neutrophils 11 (55) Macrophages 11 (55) Plasma cells 0 (0) Depth of the infiltrate Superficial and deep 19 (90) Superficial 1 (5) Density of the infiltrate Moderately dense 17 (75) Dense 1 (10) Sparse 2 (10) Distribution of the infiltrate Perivascular, periadnexal and interstitial 16 (80) Perivascular and periadnexal 4 (20) Perivascular and interstitial 0 (0) Involvement of the adnexal structures 19 (95) Sweat glands 16 (80) Hair follicles 8 (40) Sebaceous glands 6 (30) Wedge-shaped form of the infiltrate 7 (35) Other features Extravasations of erythrocytes Flame figures Swollen vessel walls and/or dilated vessels Eosinophilic panniculitis 4 (20) 3 (15) 2 (10) 1 (5) Epidermal changes were determined in most biopsies (n = 18, 90%). Spongiosis was the most relevant finding as it was apparent in 18 biopsies (90%). Within the epidermis, it was determined in 15 cases (75%), whereas spongiotic infundibulitis and/or spongiotic acrosyringitis (spongiosis in the acrosyringeal portion of the eccrine duct) were available in five biopsies (25%). Epidermal as well as adnexal spongiosis was present in four biopsies (20%). Exocytosis of eosinophils into the epidermis with particular accumulation within intraepidermal vesicles – a phenomenon referred to as eosinophilic spongiosis – was displayed in five biopsies (25%) (Fig. 3). Fig. 3. Focal accumulation of neutrophils and in particular eosinophils within a spongiotic epidermis. (hematoxylin and eosin, original magnification ×200). [Normal View ] Most biopsies were characterized by a moderately dense (n = 17, 75%), superficial and deep inflammatory infiltrate (n = 19, 90%). In the majority of the biopsies (16 biopsies, 80%) it was distributed in a perivascular, periadnexal and interstitial pattern (Figs. 1b, 2b and 4a). Features of periadnexal involvement (either of the sweat glands, hair follicles or sebaceous glands) were displayed in 19 of 20 biopsies (90%). The sweat glands seemed to be completely implicated in the inflammatory process because infiltration was observed in the acrosyringeal portion, around and within sweat ducts as well as in the deep dermis/subcutis affecting the coiled gland (Fig. 1c, 2c and 4a–c). Through analyzing consecutive biopsy sections, in 16 of all slides (80%) sweat gland involvement extending along the entire structure of the glands was noted. In eight cases (40%), the infiltrate involved the hair follicles (perifollicular/folliculocentric infiltrate) and in six (30%), the sebaceous glands. Lymphocytes and eosinophils were the fundamental components of the infiltrate as both were present in all biopsies examined (n = 20, 100%); in five (25%) of them eosinophils predominated. The latter could be noted within the epidermis as well as in the reticular dermis, scattered interstitially among the collagen fibers and accounting occasionally for the development of flame figures (n = 3, 15%), and/or descending toward the deeper parts of the dermis. Neutrophils were additionally present in 11 specimens (55%), being the predominant cell component in two of them (10%). The infiltrate was estimated as wedge shaped (V-shaped, with the base of the V in the direction of the subcutaneous fat) in seven cases (35%). However, the small size of biopsy material did not allow for the assessment of this peculiar form in most cases. Fig. 4. A, B, C) Involvement of the sweat glands – from the acrosyringeal portion, along the sweat ducts downwards to coiled glands in the deep dermis. Note also the interstitial distribution of the eosinophils in (B) (hematoxylin and eosin, original magnification ×40, ×100, ×200 accordingly). [Normal View ] Extravasated erythrocytes (four biopsies, 20%) and swollen vessel walls and/or dilated capillaries (n = 2, 10%) were recognized as consistent with the arthropod bite pattern because they represent a further sign of external insult to the skin. Although nuclear dust and extravasated erythrocytes occurred, microthrombi and fibrinoid necrosis of the vessel walls were absent and leukocytoclastic vasculitis was not a feature (0 biopsies, 0%). The subcutis was particularly involved in one case (10%), showing a mixed infiltrate of lymphocytes, macrophages and numerous eosinophils, extending both within septa and lobules, a pattern referred to as 'eosinophilic panniculitis' (Fig. 5). Fig. 5. A mixed infiltrate of lymphocytes and numerous eosinophils, extending into the subcutaneous fat (eosinophilic panniculitis) (hematoxylin and eosin, original magnification ×200). [Normal View ] Discussion The histopathologic findings presented here emphasize and enhance the spectrum of knowledge about arthropod reactions. Spongiosis was the predominant feature characterizing the epidermal changes. Keeping in agreement with previous data (Table 1), we observed two patterns of spongiosis – an early discrete focus of spongiosis present in the epidermis at the very site of the insect bite and a more extending pattern accompanied by the formation of multiloculated vesicles/vesiculopustules. An interesting observation was the relatively high number of biopsies disclosing spongiotic infundibulitis and/or spongiotic acrosyringitis (25%). An ostium of an infundibulum is sampled frequently by the insects as a site for biting because it harbors delicacies loved by them (bacteria, yeasts, mites and lipids from the sebaceous glands).3,7 Moreover, because of the effects of the microorganisms 'residing' in the follicle, an odor is emitted that seems to attract the arthropods. Hence, spongiosis is formed within the infundibulum, thus specifying insect bites as foliculocentric.7,9 The involvement of the acrosyringium in arthropod bites has been reported in one study only,9 yet providing no evidence about the pathogenesis of this phenomenon. Exocytosis of eosinophils in the spongiotic foci (eosinophilic spongiosis) was presented in 25% of all cases revealing spongiosis,3,6,7,24 and therefore, if present, should be considered as a sensitive clue to the diagnosis. However, eosinophilic spongiosis could be observed in heterogeneous group of dermatoses,6 the bullous diseases being among the most common to differentiate from. Of help is the fact that in arthropod reactions, the eosinophilic spongiosis occurs only focally and the eosinophils predominate usually in the deeper parts of the biopsy, whereas in urticarial stages of bullous dermatoses, an extended distribution of eosinophils in particular along the epidermal-dermal junction is expected.4 Other epidermal changes, such as the presence of a crust, erosion/ulceration, mild acanthosis, ortho/hyperkeratosis, parakeratosis and features of lichen simplex chronicus were determined in less of the half of our biopsy specimens. They usually occur as a secondary phenomenon in the course of the bite reaction because of energetic scratching on the site of the assault. They, therefore, should be applied as a diagnostic criterion with the reservation that a relatively old lesion has been biopsied. A helpful clue might be the presence of eosinophils within the serum crust. Of note, eosinophils attribute a constant feature to the inflammatory infiltrate in insect bite reactions as they were present in all cases regardless of their amount. Apart from forming collections in spongiotic vesicles, they determine the appearance of other three phenomena – their interstitial distribution, the formation of flame figures and eosinophilic panniculitis. Flame figures are considered commonly a helpful clue to the diagnosis of an insect bite reaction.3,6 We identified them only in four of our biopsies. Degeneration of the dermal collagen may result from the degranulation of the lysosomal enzymes in the eosinophils as well as from those released by the neutrophils.3 Hence, flame figures are of minor help to the diagnosis. Moreover, because in 50% of the cases macrophages are available, there might be a shortage of time for the granules to act upon the collagen as the macrophages ingest the degranulated eosinophils greedily. Besides, flame figures are considered a peculiar response to multiple factors and therefore do not label a specific etiology.3,6,25 'Eosinophilic panniculitis' can be found as a histopathologic pattern in erythema nodosum, vasculitis, parasitic infection, drug injections, Wells' syndrome, leukemia and in arthropod bites.6 As the coiled glands, embedded in the subcutis, seem to be implicated considerably in arthropod bite reactions, panniculitis may ensue. However, the presence of eosinophilic panniculitis should be considered a helpful clue to the diagnosis only in cases of a clinical history for arthropod bites and/or in the presence of the other relevant criteria. In accordance to previous data (Table 1), a moderately dense superficial and deep inflammatory infiltrate was observed in most of the biopsies revised. Most authors proclaim a perivascular and interstitial pattern of the infiltrate's distribution.3,6–8 However, the most prevalent type of infiltrate observed in our sample revealed perivascular, periadnexal and interstitial distribution (80%). The periadnexal distribution of the infiltrate as a feature of an insect bite reaction has been already alluded by Ackerman et al.3,7 who suggested that some insects (mosquitoes) seem to bite at the site of an ostium of a hair follicle thus inducing a folliculocentric infiltrate.9 However, the probable involvement of the sweat glands has been mentioned only twice in the available literature. Jordaan and Scheider recognized spongiotic acrosyringitis as the only pattern of sweat gland affection,9 whereas Schaffer et al.26 remarked on the perivascular and periappendiceal disposal of the infiltrate in the middle and lower thirds of the corium, concentrated chiefly about the sweat glands. About 80% of the slides in our sample disclosed sweat gland involvement extending along the entire structure of the glands as not only the acrosyringial portion, but also the sweat ducts and the coiled glands were implicated in the inflammation. It might be assumed that the orifice of a sweat gland is another attractive site for arthropod assaults. Evidence exists that mosquitoes, for example, use physical, visual and olfactory cues to locate their blood hosts,27 whereas human temperature, moisture, carbon dioxide in the exhaled breath and body emanations are the crucial attractants.27–31 Sweat is a major source of human volatile emissions in which carboxylic acids and Z-3-methyl-2hexenoic acid and 7-octenoic acid are key substances.32 The olfactory tissues of the insect recognize such kairomones and info-chemicals. However, when comparing different body regions from a naked motionless human host, the head and feet have been defined the most preferred sites for biting because they possess a particular combination of skin temperature and sweat gland density.33 We, therefore, suggest that the orifices of the sweat glands are preferred by the mosquitoes. Regarding the further involvement of the lower part of the gland, we assume that the intraepidermal duct and the secretory sweat gland coil both act as a penetration pathway (canal) through which substances are transported.34 Arthropods while assaulting the acrosyringia probably release toxic or irritating substances which diffuse further into the lumen of the gland and the surrounding tissue, thus resulting in a persistent inflammatory reaction. This condition can be referred to as eosinophilic hidradenitis because eosinophils are strongly involved in the inflammatory infiltrate enveloping the gland structures. The wedge shape of the infiltrate is considered usually a criterion of major importance in arthropod bite reactions.3,7 It occurs probably as a consequence of the frontal assault as the insect charges headlong at nearly a right angle into the skin. The infiltrate was wedge shaped in 35% of our specimens. Nevertheless, its diagnostic value renders mistrust as its appearance is a rather subjective and speculative phenomenon arising from the V-form of most of the biopsy specimens obtained. Furthermore, superficial sections or small punch biopsies do not enable the accurate assessment of the wedge shape of the infiltrate.4 Histopathologic features of arthropod bite reactions are diverse and depend on numerous factors. Distinction and observation of major and minor histopathologic criteria (specified according to the relevance of their occurrence) might be of help for the evaluation of arthropod reactions (Table 3). We provide morphologic evidence that the involvement of the adnexal structures, particularly the acrosyringia, the sweat ducts and the coiled glands, should be considered a new reliable diagnostic tool. Table 3. Histopathologic criteria for arthropod bite reactions Histopathologic clues Epidermal spongiosis (eosinophilic spongiosis particularly) Spongiotic infundibulitis and/or spongiotic acrosyringitis Scale-crust with neutrophils and eosinophils Moderately dense/dense, superficial and deep infiltrate with perivascular, periadnexal and interstitial distribution Extention of the infiltrate along the sweat ducts and the coiled glands Interstitially distributed eosinophils Involvement of the hair follicles and/or the sebaceous glands Histopathologic criteria of minor relevance Mild acanthosis, focal parakeratosis, scale crust, ulceration Edema in the papillary dermis Wedge-shaped form of the infiltrate Extravasations of erythrocytes/swollen endothelia and/or dilated vessels Flame figures Neutrophils in the infiltrate and/or minor leukocytoclasia Eosinophilic panniculitis" References 1. Bircher AJ. Systemic immediate allergic reactions to arthropod stings and bites. Dermatology 2005; 210: 119. Links 2. Steen CJ, Carbonaro PA, Schwartz RA. Arthropods in dermatology. J Am Acad Dermatol 2004; 50: 819. Links 3. Ackerman BA. Atrhropod bite and analogous reactions. In Ackerman BA, Chongchitnant N, Sanchez J, Guo J, Bennin B, Reichel M, Randall MB, eds. Histologic diagnosis of inflammatory skin disease: an algorithmic method based on pattern analysis. Baltimore: Williams & Wilkins, 1997; 202. 4. Kerl H, Garbe C, Cerroni L, Wolff HH. Arthropodenreaktion In Kerl H, Garbe C, Cerroni L, Wolff HH, eds. Histopathologie der Haut. Berlin, Heidelberg, New York: Springer Verlag, 2003. 5. Zhu YI, Stiller MJ. Arthropods and skin diseases. Int J Dermatol 2002; 41: 553. Links 6. Weedon D. Arthropod-induced diseases. In Weedon D, ed. Skin pathology. London: Churchill Livingstone, 2002; 744. 7. Ackerman BA, Böer A, Bennin B, Gottlieb G. Histologic diagnosis of inflammatory skin diseases. An algorithmic method based on pattern analysis. 3rd ed. New York: Ardor Scribendi, 2005. 8. Elder D, Elenitsas R, Jaworsky C, Johnson B Jr. Parasitic infestations of the skin. In Elder D, Elenitsas R, Jaworsky C, Johnson Jr B., eds. Lever's histopathology of the skin. Lippincott Philadelphia-New York: Williams & Wilkins, 1997; 565. 9. Jordaan HF, Scheider JW. Papular urticaria: a histopathologic study of 30 patients. Am J Dermatopathol 1997; 19: 119. Links 10. Garcia E, Halpert E, Rodriguez A, Andrade R, Fiorentino S, Garcia C. Immune and histopathologic examination of flea bite-induced papular urticaria. Ann Allergy Asthma Immunol 2004; 92: 446. Links 11. Cho BK, Kang H, Bang D, Kim SN, Hwang S, Song ES. Tick bites in Korea. Int J Dermatol 1994; 33: 552. Links 12. Falk ES, Eide TJ. Histologic and clinical findings in human scabies. Int J Dermatol 1981; 20: 600. Links 13. Fernandez N, Torres A, Ackerman AB. Pathologic findings in human scabies. Arch Dermatol 1977; 113: 320. Links 14. Hejazi N, Mehregan AH. Scabies: histological study of inflammatory lesions. Arch Dermatol 1975; 111: 37. Links 15. Galaria NA, Chaudhary O, Magro CM. Tick mouth parts occlusive vasculopathy: a localized cryoglobulinemic vasculitic response. J Cutan Pathol 2003; 30: 303. Links 16. Stefanato CM, Phelps RG, Goldberg LJ, Perry AN, Bhawan J. Type-Icryoglobulinemia-like histopathologic changes in tick bites: a useful clue for tissue diagnosis in the absence of tick parts. J Cutan Pathol 2002; 29: 101. Links 17. De la Torre C, Toribio J. Sea-urchin granuloma: histologic profile. A pathologic study of 50 biopsies. J Cutan Pathol 2001; 28: 223. Links 18. Elston D, Eggers JS, Scmidt WE, et al. Histological findings after brown recluse spider envenomation. Am J Dermatopathol 2000; 22: 242. Links 19. Khamaysi Z, Dodiuk-Gad RP, Weltfriend S, et al. Insect bite-like reaction associated with mantle cell lymphoma. Clinicopathological, immunopathological and molecular studies. Am J Dermatopathol 2005; 27: 290. Links 20. Pederson J, Carganello J, Van-Der Weyden MB. Exaggerated reaction to insect bites in patients with chronic lymphocytic leukemia. Pathology 1990; 22: 141. Links 21. Rosen LB, Frank BL, Rywlin AM. A characteristic vesiculobullous eruption in patients with chronic lymphocytic leukemia. J Am Acad Dermatol 1986; 15: 943. Links 22. Diven DG, Newton RC, Ramsey KM. Heightened cutaneous reactions to mosquito bites in patients with acquired immunodeficiency syndrome receiving zidovudine. Arch Intern Med, 1988; 148: 2296. Links 23. Kunzig M, Steigleder GK. Histological study of the mosquito-bite infiltrate in patients with various underlying diseases and different medications. Z Hautkr 1977; 52: 37. Links 24. Ruiz E, Deng JS, Abell EA. Eosinophilic spongiosis: a clinical, histologic, and immunopathologic study. J Am Acad Dermatol 1994; 30: 973. Links 25. Schorr WF, Tauscheck AL, Dickson KB, Melski JW. Eosinophilic cellulitis (Wells' syndrome): histologic and clinical features in arthropod bite reactions. J Am Acad Dermatol 1984; 11: 1043. Links 26. Schaffer B, Jacobsen C, Beerman H. Histopathologic correlation of lesions of PU and positive skin test reactions to insect antigens. Arch Dermatol Syphiol 1954; 70: 437. Links 27. Takken W. Malaria mosquitoes favor the human skin and not expired air. Int J Dermatol 2000; 39: 180. Links 28. Mukabana WR, Takken W, Coe R, Knols BGJ. Host-specific cues cause differential attractiveness of Kenyan men to the African malaria vector Anopheles gambiae. Malaria J 2002; 1: 17. Links 29. Stibich AS, Carbonaro P, Schwartz RA. Insect bite reactions: an update. Dermatology 2001; 202: 193. Links 30. Lindsay SW, Adiamah JH, Miller JE, Pleass RJ, Armstrong JR. Variations of attractiveness of human subjects to malaria mosquitoes (Diptera: Culicidae) in The Gambia. J Med Entomol 1993; 30: 368. Links 31. Enserink M. What mosquitoes want: secrets of host attraction. Science 2002; 298: 90. Links 32. Constantini C, Birkett MA, Gibson G, et al. Electroantennogram and behavioural responses of malaria vector Anpheles gambiae to human-specific sweat components. Med Vet Entomol 2001; 15: 259. Links 33. De Jong R, Knols BG. Selection of biting sites on man by two malaria mosquito species. Experientia 1995; 15: 80. Links 34. Wilke K, Wepf R, Keli FJ, Wittern K-P, Wenck H, Biel SS. Are sweat glands an alternate penetration pathway? Understanding the morphological complexity of the axillary swaet gland apparatus. Skin Pharmacol Physiol 2006; 19: 38. Links