A REVIEW OF HEALTH HAZARDS FROM HAM
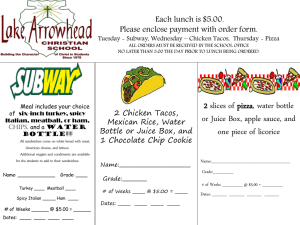
advertisement

A REVIEW OF THE POTENTIAL HEALTH HAZARDS OF HAM C. B Garvan MVB, PGCertFoodSafety Department of Food Science, Dublin Institute of Technology, Dublin1, Ireland Objective: To review the literature regarding health hazards of ham Time scale and design: The review was completed in January 2005. Relevance: To bring together under one source the hazards of ham Previous experience of theory: Change to existing theory or practice; Claim: The first compilation of microbiological and chemical hazards relating to ham. Impact: - ABSTRACT The microbiological and chemical hazards associated with ham have been compiled to give a comprehensive overview of the risk posed to the consumer by this foodstuff. The epidemiological factors of food borne diseases due to ham, as well as symptoms and outbreaks are also discussed. The predominant microbial hazards are Salmonella spp., E. coli, Staphylococcus aureus, Campylobacter spp., Listeria monocytogenes, Clostridia spp., Yersinia enterocolitis, Aeromonas spp., Norwalk-like virus and endoparasites. In terms of chemical hazards: nitrites, antimicrobials, environmental and industrial contaminants are detailed along with their side effects and levels of detection in ham. KEYWORDS: Ham, Health, Hazards INTRODUCTION Food borne disease is perhaps the most widespread health problem in the contemporary world and an important cause of reduced economic productivity (W.H.O., 1992). Consumers are becoming more informed on food safety issues so that food poisoning is at the forefront of publicity campaigns on health. Clinically healthy pigs may carry a range of human pathogens including, Salmonella, Campylobacter, Escherichia coli and Yersinia, which may be transferred during slaughter from the porcine skin, tonsils and intestinal tract onto the carcasses and ultimately onto the meat cuts. International food poisoning data suggests that pork is an important source of food borne pathogens. The average incidence in The Netherlands, for example, is about 450 per 100,000 of the population, with an estimated 15% of these being associated with pork consumption (Berends et al., 1998b). REVIEW OF HAZARDS (a) Salmonella Salmonella is found in the entire digestive tract and lymphatic tissue of pigs. They are asymptomatic carriers and acquire infection from other carriers or contaminated feed. Transfer between pigs is particularly associated with stressful and crowded conditions eg: transport to factory and when in the lairage. Salmonellosis is a zoonotic infection where the major source of human illness is infected animals. Transmission is by the faecal -oral route and symptoms include fever, nausea, vomiting and diarrhoea, usually self-limiting and lasting a few days but in susceptible groups such as the young and elderly, it can be more severe. Some special risk groups are: persons with underlying disease such as cancer or diabetes mellitus, persons who use excessive antacids or have been recently been treated with antibiotics that disturb the normal gut flora. Live animals that carry Salmonella spp. are 3-4 times more likely to end up as positive carcass than Salmonella-free animals (Berends et al., 1997). It has been suggested that 90% of cross-contamination that occurs in cutting plants is unavoidable as long as contaminated carcasses are being processed. Furthermore 10% of butcher's shops or kitchen's of restaurants may become colonized for several weeks or months with their own endemic "house flora" of Salmonella spp., introduced via contaminated products of animal origin (Berends et al., 1998). Therefore, as pigs are the only important source for Salmonella contamination of the line and the carcasses produced, it can also be concluded if Salmonella-free pigs were produced, consumers could be provided with Salmonellafree pork (Berends et al., 1997). In Denmark, pork is the second highest food source of Salmonella spp., with approximately 15% of the 95 cases per 100,000 attributed to pork consumption (Hald and Wegener, 1999). In 1993 an outbreak in Copenhagen resulted in 550 people becoming ill (Bager et al., 1995). In June 1998, an outbreak of multi-resistant Salmonella Typhimurium DT 104 resulted in 25 culture-confirmed cases and 2 deaths (Baggesen et al., 1999). The source of infection was traced back to a local pork abattoir. In a small study at one Irish pork plant the incidence of Salmonella on pigs immediately after bleeding ranged from 2% to 60% (Bolton et al., 2001), Salmonella spp. isolated included S. Typhimurium, S. Hadar S. Infantis and S. Derby. The National Food Centre in Ireland found that 9.9% of pork samples in a small survey in retail outlets in the Dublin region were contaminated with Salmonella spp. (Duffy et al., 1999). In the past few years in Ireland there have been several outbreaks of Salmonella Typhimurium with high levels of human morbidity and mortality resulting from the consumption of contaminated ham according to the annual report of Food Safety Authority of Ireland (2002). Oosterom et al., (1985) reported an incidence of 21% Salmonella spp. in Dutch pigs while D'Aoust (1989) in a study encompassing several countries, found that pork carcass contamination ranged from 0.4% to 76.3% with an average of 16.2%. Salmonella spp. can exist for many months in the environment especially if protected from extremes of temperature and sunlight, therefore recycling through the environment is an important route for animal and human infection. An epidemic of Salmonella Typhimurium associated with traditional salted, smoked and dried ham leading to gastroenteritis after a family party was documented in Holland in 1999. Of the 109 people who attended the party 35% were affected and conclusions were that the preservative methods were not sufficently effective to eliminate or reduce Salmonella to non-infective levels (Mertens et al., 1999). An outbreak of Salmonella Typhimurium infection affected 39 people over a wide area in North-West England and North Wales in April and May 1991. The cause of the outbreak was a particular cooked ham from a small local producer and the Salmonella phage type was identified using antibiotic resistance patterns (Thornton et al., 1992). An epidemic of restaurant associated illness involving 120 people, was seen in Arkansas in 1982 , where the source of the pathogen was ham or pork sandwiches. Faecal samples and culture of sliced ham were positive for Salmonella Newport (Narain et al., 1989). A food-borne outbreak of gastroenteritis occurring in Finland and the United Kingdom was traced back to cured ham, the causal agent was Salmonella Enterica serovar newport (Lyytikainen et al., 2000). (b) Escherichia coli Enterohaemorrhagic Escherichia coli (EHEC) is the most common food borne coliform and the illness it causes can range from a non-bloody diarrhoea, through haemorrhagic colitis, to the life-threatening conditions haemolytic uraemic syndrome (HUS) and thrombotic thrombocytopaenic purpura (TTP).The Coliforms are inhabitants of the gastro-intestinal tract of humans and animals, as harmless commensals, but some are opportunistic pathogens. Escherichia coli make up a large proportion of the intestinal micro flora of pigs. E. coli O157:H7, the verotoxigenic E coli most commonly associated with food poisoning in Europe and the U.S.A. , has been isolated from pork retail meats (Doyle and Schoeni,1987) . Korsak et al. (1998) isolated EHEC from from 14% of Belgian pork carcass samples. In Ireland, the number of reported cases of E. coli food poisoning has increased from 8 in 1996 to 76 in 1998. The incidence in 1998 of 2.1 per 100,000 is high in comparison with other European countries (F.S.A.I. ,1999 ). Bouvet et al. (2002) found that the porcine VTEC strains isolated in french pork probably did not present a hazard since although all strains harboured a stx gene, they did not have other virulence genes. Therefore general hygiene measures were sufficient so as not to warrant specific hygiene for VHEC. Heuvelink et al., (1999), found E. coli O157 in 1.3% of raw minced pork and 0.3% of other raw pork products and concluded that raw meat contaminated with VTEC O157 will remain a hazard even if the meat is held at freezing temperatures. It was found that E coli O157: H7 can survive and grow in reconditioned pork processing wastewater, suggesting a potential hazard if this water becomes contaminated with this pathogen. E. coli O157:H7 outbreaks of food poisoning have mostly involved undercooked meat products, it is a surface contaminant. Four cases of haemolytic uraemic syndrome and seven cases of haemorrhagic diarrhoea associated with verocytotoxin producing E. coli O157 was reported in 1996. It occurred in Warwickshire in England and the vehicle of infection was thought to be home- cooked ham from a butcher's shop (Gammie et al., 1996). (c) Staphylococcus aureus In many countries, Staphylococcus aureus is considered to be the second or third most common pathogen causing outbreaks of food poisoning, only outnumbered by Salmonella spp., and in competition with Clostridia perfringens (Atanassova et al., 2001). Food poisoning by Staph. aureus is characterized by a short incubation period . Ham is frequently implicated as the source of the staphylococcal enterotoxins. It is the presence of the preformed enterotoxin in the in the ham. Symptoms of illness include nausea, vomiting, diarrhoea , headache and fever, although it is usually relatively mild and short-lived. Ham was the most common vehicle of staphylococcal enterotoxin (Bryan 1988). Contamination of the ham by food handlers would be the most common cause of infection as the micro-organism is found on the skin and mucous membranes, particularly the nasal tract of healthy individuals. Ham may be contaminated by infected skin lesions, or coughing or sneezing. Staphylococcus aureus is salt tolerant and can tolerate lower water availability than other bacteria, so it survives well in ham. However a higher salt content and lower water availability of country cured ham reduced growth and toxin production of Staphylococcal aureus (Portocarrero et al., 2002). An outbreak occurred aboard an aircraft in 1975, where 57% of 344 passengers developed gastrointestinal illness. Inappropriate preparation of the food as well as contamination from lesions on the cook's fingers lead to detection of S. aureus (Eisenberg et al., 1975). Another outbreak of food poisoning involving 17 people who consumed cooked ham occurred in Florida 1997. Staphylococcal enterotoxin Type A was identified from a sample of the ham (Ward et al., 1997 ). An outbreak in an elementary school in Rhode Island, U.S.A. was caused by improper refrigeration, prolonged handling and inadequate reheating. Large amounts of preformed enterotoxin A was found in the leftover ham (Richards et al., 1993). (d) Campylobacter Campylobacter jejuni and Campylobacter coli are a major cause of diarrhoeal illness. Symptoms include an acute enterocolitis, with malaise, fever, severe abdominal pain and diarrhoea. Vomiting is a less common feature, complications are rare although reactive arthritis can develop also the serious neurological disease, Guillain-Barre syndrome. Campylobacter spp. cannot survive cooking or pasteurization temperatures, they do not grow below 28C and survive poorly at room temperature. Campylobacter spp are sensitive to drying and acidic conditions. They are commensals in the gastrointestinal tract of pigs and occur on meat due to carcass contamination during slaughter. Numbers are greatly reduced during the chill process in the abattoir, a survey in the United Kingdom found a decrease from 59% to 2% (Adams and Moss, 2000). Reported levels of this organism on pork ranges from 10% (Epling et al., 1993), to 56% (Bolton et al., 1996). However . a small survey failed to detect Campylobacter in pork at Dublin retail outlets (Cloak, 1999). A study done between March 2001 and October 2002 found 5.1% of raw pork was Campylobacter positive with 84% being Campylobacter jejuni (Whyte et al., 2004). Arcobacter is a Campylobacter-like genus frequently associated with enteritis in pigs. Two species, Arcobacter butzleri and Arcobacter cryaerophilus have been linked to diarrhoea and bacteraemia. Studies in the United States and Europe have isolated Arcobacter species from pork but figures vary from 0.5 to 97%. This may be due to confusion between Arcobacter and Campylobacter identification (Adams and Moss, 2000). (e) Listeria monocytogenes Listeria are ubiquitous in the environment, Listeria monocytogenes is the only important human pathogen in the genus. Incidence of infection is low as a susceptible individual needs to be exposed to a high dose of a virulent strain. Symptoms can vary from a mild, flu-like illness to meningitis, meningoencephalitis, septicaemia and endocarditis. In pregnant women, listeriosis can result in abortion, stillbirth, or premature labour. In newborns it can cause pneumonia, septicaemia and disseminated abscesses. The persistent existence of selected strains of L. monocytogenes over long periods of time in meat-processing plants despite cleaning and disinfection procedures, has been described by several authors ( Szymanska and Medrala, 2003). It is relatively resistant to curing ingredients used in ham production, and so represents a risk to the consumer (Portocarrero et al., 2002). It can grow in refrigerated conditions and can adapt to an acidic environment. If vacuum-packed ham is already contaminated and left in the fridge, L. monocytogenes can multiply. In Britain in 1989/90 high levels of L. monocytogenes on vacuum-packed ham prompted recall of the product from the market. It does not produce slime or a smell like spoilage bacteria, so if other spoilage bacteria are eliminated it has no competition. There is competitive inhibition of L. monocytogenes in ham by lactic acid bacteria (Amezquita et al., 2000), but Beumer et al., (1996) had suggested it is slight. An Irish study done in 1994 found that 45% of pork samples at retail level in Dublin were contaminated with Listeria (Sheridan et al., 1994). Heat-survivors appear to be the main cause of post-process survivors. There was a major outbreak of listeriosis in France in 1992, in which 249 people were infected (Rocourt et al., 1993). In this case the major causes of contamination identified were contact of cooked products with soiled surfaces, cross-contamination between " raw" and "cooked" channels, and the inadequacy of cleaning and disinfection procedures (Salvat et al., 1995). (f) Clostridium perfringens Clostridium perfringens food poisoning is generally a self-limiting, non-febrile illness characterised by nausea, abdominal pain, diarrhoea and less commonly vomiting. Recovery is usually within 1-2 days, although occasionally it can be fatal in the very old or debilitated. The species is classified into five types, A-E, based on production of exotoxins. Clostridium perfringens Type A is responsible for food poisoning and produces alpha major toxin. Clostridium perfringens Type C which produces alpha and beta toxins, causes enteritis necroticans, a more severe, but far more rare enteric disease seen in Papua New Guinea (Adams and Moss, 2000). Most outbreaks of food poisoning due to Clostridium perfringens, occur in institutions such as old people's homes, hospitals and schools. Cured ham is rarely involved due to the combined effect of salt content, nitrite content and heat processing, to control growth of Clostridium perfringens. An outbreak occurred in a large hospital in England in 1977, affecting one third of the patients, one frail patient died. A minced ham dish was found to be the vehicle of transmission of the food poisoning (Noah, 1977). (g) Clostridium botulinum Botulism is the form of bacterial food poisoning which has the earliest reports, due to the severe and distinctive symptoms. Botulism results from ingestion of an exotoxin produced by C. botulinum growing in the food. The toxins are neurotoxins, and affect the peripheral nervous system. Initial symptoms include vomiting, constipation, urine retention, double vision, dysphagia, dry mouth and difficulty in speaking. The patient remains conscious until the progressive weakness results in respiratory or heart failure. Infant botulism, which occurs in babies aged 2 weeks to 6 months, particularly at time of weaning, differs from the classical syndrome in that it results from colonization of the child's intestines with C. botulinum and toxin production in situ. Two outbreaks of food-borne botulism involving 16 cases in Croatia, occurred in 1985. Epidemiologic studies implicated smoked home-made ham as the possible vehicle of transmission. The clinical manifestation of these cases was milder than generally reported, and none of the patients died or required respiratory assistance (Brncic-Dabo et al., 1987). An outbreak in Istria, in 1985, involved 13 people who ate home-cured ham. Toxin B was identified (Terlevic et al., 1988). Smoked ham was responsible for some of the 13 outbreaks of food-borne botulism that occurred in Portugal between 1970 and 1984 (Lecour et al., 1988). Data from Yugoslavia in the period from 1994-1999 showed 87 cases of botulism due to home-made dry ham (Vukovic, 2000). France appears to have a lot of reported outbreaks of botulism, with 108 cases recorded in Poitiers from 1965 to 1990, in 83% of patients the food responsible was home-cured ham (Roblot et al., 1994). Home-cured ham, was found to be contaminated with C. botulinum in cases of food poisoning occurring during 1998-2000 (Carlier et al., 2001). Further data on 2001/2002 showed 35 outbreaks with 62 people affected, no deaths. Most outbreaks involved home-cured hams and were caused by type B toxin (Haeghebaert et al., 2003). (h) Yersinia Yersinia enterocolitica is another member of the enterobacteriaceae family. Yersinia is a water and food-borne enteropathogen, it has been isolated from ham, and has caused a broad range of diseases. Illness includes gastroenteritis, arthritis and uveitis, a self-limiting enterocolitis is most commonly seen in children under seven years old. Pigs are chronic carriers of this microorganism, Yersinia is spread from the intestines, tonsils, and tongue during slaughter. Two surveys, one in Norway (Nesbakken et al.,), and another in Japan (Fukushima et al.,1987), found that 27% and 97.5% of pork products were contaminated at retail level. A survey in the Dublin area (Duffy et al.,1999), showed 100% incidence. (i) Aeromonas Aeromonas hydrophila has the ability to grow at chill temperature, reportedly as low as -0.1C. Its principal reservoir is water and it can grow in potable water as it is resistant to chlorine. Gastroenteritis associated with Aeromonas, commonly occurs in young children. It does not survive even mild cooking procedures, but can be introduced as a result of under-cooking, or use of contaminated water. In Sweden, Aeromonas was implicated in an outbreak of food poisoning linked to boiled ham (Krovacek et al., 1995). (j) Spoilage Bacteria The predominant bacteria associated with spoilage of refrigerated ham are, Bronchotrix thermosphacta, Carnobacterium spp., Enterobacteriaceae, Lactobacillus spp., Pseudomonas spp., Leuconostoc spp. and Shewanella putrefaciens. The main defects are off-odours and off-flavours (Borch et al., 1996). Lactic acid bacteria are commonly found in vacuum-packed ham stored at chill temperatures, they have already been mentioned in relation to Listeria monocytogenes. Vacuum and modified-atmosphere packing of ham changes the meat microflora, and the type of spoilage bacteria that predominate. Restriction of Pseudomonads leads to microflora dominated by gram positive bacteria, particularly lactic acid bacteria. These microorganisms cause slime formation, greasing and souring of ham. Lactic acid bacteria can be used to inhibit growth of Listeria monocytogenes and Escherichia coli 0157:H7 in cooked ham products. After storage for 21 days at 8C cooked sliced vacuum-packaged ham, inoculated with strains of lactic acid bacteria, still had acceptable sensory properties (Bredholt et al., 1999). Ham et al., (2003) suggests that some of the lactic acid bacteria, on the basis of their ability to inhibit pathogenic microbes, such as S. Typhimurium, E. coli and L. monocytogenes, could be used as probiotics and reduce use of in-feed antibiotic. (k) Norwalk-Like Virus A number of viruses have been implicated in gastroenteritis incidences; however, in relation to ham it is the Norwalk-like (Noro) viruses which are most often responsible for food poisoning. Contamination generally occurs during handling, preparation and serving. An outbreak of acute gastroenteritis at a Texas university in 1998, was traced back to deli-ham contaminated by a food handler whose child was positive for Norovirus (Daniels et al., 2000). Two other outbreaks of gastroenteritis illness which occurred after a hotel banquet in England, was also traced back to consumption of cold cooked ham, contaminated by a food handler who was excreting the virus, and a poor standard of hygiene in the kitchen (Riordan et al., 1984). (l) Trichinella spiralis Trichinella spiralis are roundworms that are found in the muscle of the pig. Ingestion of heavily infected meat leads to nausea, diarrhoea and abdominal pain, which usually occurs within a few days, or up to a month later, if only a few larval cysts are ingested. The second stage of disease results in muscle pain and fever, as the larvae invade and encyst in the muscle tissue. Trichenellosis is a severe disease, and often fatal. Trichinella spiralis is generally tested for in the meat at slaughter in the abbatoir, however pork which is rapidly frozen in accordance with Annexe IV of Directive 77/96/EEC, which is exempt from examination (Bolton and Sheridan, 2001). Smoked ham was responsible for an outbreak of trichinellosis in Slovakia (Dubinsky et al., 2002). Two outbreaks occurred involving fourteen people living in France in 1993. Four people were infected via smoked ham, tan from salami, both from two wild boars (Bernard et al., 1995). Smoked ham was also responsible for an outbreak affecting three people in Yugoslavia in 1995. In France, thirty nine cases occurred at a restaurant in October and November 1985, due to ham from a wild boar that was incorrectly prepared without pickling in brine. Eighty wild boars were subsequently killed, all negative for trichinella (Ancelle et al., 1989). (m) Chemical Hazards associated with ham There is growing consumer resistance to the presence of unwanted residues in food generally. The principal consumer concerns are drug resistance, toxicity and potential allergy eg: penicillin. The first source of a chemical hazard in the production process would be the raw pork. A chemical residue may be a natural contaminant arising from feed, eg: mycotoxins. Mycotoxins are metabolites of moulds which may contaminate foods, or animal feeds, and are toxic to humans. Ochratoxin A may occur as a contaminant of cereals used for pig feed. It is produced by Penicillium verrucosum, when it contaminates cereals in countries with a temperate climate. Ochratoxin A causes kidney disease in pigs and may be passed to meat products (Adams and Moss, 2000). There have been suggestions of a link to testicular cancer due to exposure to ochratoxin A in utero or early childhood.Studies done by National Food Centre in Ireland showed that pork products may be contaminated but levels in 1999 were significantly lower than other countries. Ochratoxin A works synergistically with citrinin, (mycotoxin produced by P. citrinum) and has an additive effect in terms of toxicity. Citrinin has been detected in country -cured ham (Wu et al.,1974). Zearalenone is an oestrogenic mycotoxin which has adverse side effects on fertility in pigs. This mycotoxin has an anabolic or growth-promoting activity, and is banned in some countries. It can be detected in ham, and there would be concern voiced regarding long term exposure to such an oestrogen. Zearalenone is common in cereals such as maize, wheat and barley. A pesticide arising from feed or from indirect or direct exposure of animals is also a potential chemical residue. The two main classes of pesticides are organochlorine (OC) and organophosphorous (OP) pesticides. A study done in 1997 by National Food Centre in Ireland showed that pork fat in 97% of 128 saples taken showed no measurable residues of (OC) pesticdes (O'Keefe et al., 2001). Two samples showed Dieldrin (OP) at 20 times lower than the maximum residue level (MRL) for that pesticide (0.2 mg/kg fat). Two further samples contained Lindane at levels 40 times lower than the recommended maximum residue limit (1.0 mg/kg fat). Results from this study indicated that there was not a problem with residues of OC and OP pesticides in pork. However studies by the Pesticide Control Service of the Irish Department of Agriculture, Food and Rural Development found 3 samples with residues of the pesticide dicofol above the MRL. Chemical substances such as dioxins, heavy metals or polycyclic aromatic hydrocarbons which are environmental and industrial contaminants also pose a chemical hazard to the consumer. Dioxins and planar polychlorinated biphenyls (PLBs) are carcinogenic and may have adverse effects on reproduction; they are fat soluble chemicals that are by-products of chemical processes from combustion. PCBs have been shown to be present in high levels in ham that is smoked (Esposito et al., 2001). The European Commission suggested maximum permissible level for dioxin of 1pg TEQ/g fat for pork. Studies in 2000 on Irish pork have shown levels of dioxin and planar PCB residues less than or equal to 1pg TEQ/g fat (O'Keefe et al., 2001). Heavy metals occur as natural constituents of meat (eg: zinc, copper, selenium) or as contaminants from industry or the environment (eg: lead, tin, cadmium, mercury and arsenic). From numerous surveys heavy metals in ham are at expected levels for natural constituents and are low or non-measurable for contaminants. Polycyclic aromatic hydrocarbons (PAH) are industrial contaminants which may occur as products of food processing operations involving heating or smoking. These may be carcinogenic and the most common PAH benzopyrene is used to check for contamination. Any Irish studies done of cured or smoked ham, have yielded results well below E.U. permissible levels (O'Keefe et al.,2001). Veterinary drugs also pose a potential chemical hazard particularly prohibited substances such as growth promoters or certain antibiotics eg: chloramphenicol or nitrofurans. Other veterinary drugs are permitted for use, but dosage is regulated and residue levels in pork at time of slaughter are monitored to check for compliance with legislation. If residues of antibiotics occur at unacceptable levels in the meat this may give rise to the potential for toxic effects in susceptible individuals. A further sequellae to unnecessary widespread use of antibiotics is the development of resistant strains of bacteria eg Methicillin-resistant Staphylococcus aureus (M.R.S.A.). An outbreak of gastroenteritis caused by Salmonella typhimuriun DT 193 was identified based on it's antibiotic resistance to sulphonamides, trimethoprim and furazolidone (Thornton et al.,1992). A study done to detect naturally occurring Salmonella spp. in Irish retail meats including pork, as well as finding it in 31% of pork, the antibiotic resistance pattern was as follows: riampicin (100%), tetracycline (92.2%), oxytetracycline (86.26%), sulphamethoxazole (86.25%) and streptomycin (80.92%) (Duffy et al., 1992). In Austria in 2003, Campylobacter spp., Salmonella spp. and pathogenic E. coli were enteric isolates, resistance to quinolones and tetracyclines. However food isolates of Y. enterocolitica and L. monocytogenes were rarely resistant (Mayrhofer et al., 2004). Results of a study done by National Food Centre in Ireland show that 30% of pork samples taken during 1996/1997 showed residues of chlortetracycline with 5% above the Maximum residue levels (MRL), however, a second study in 1997/1998 showed all samples to be free of measurable residues or had levels much lower than the MRL. In general residue levels do not occur above MRL values but positive samples have occurred with beta-lactams (penecillin/cephalosporin) and sulphonamides. Sulphonamides are one of the antimicrobials used at sub-therapeutic concentrations as a growth promoter; tylosin is also commonly used to treat swine dysentry and ileitis. Carbadox is another growth promoting antibacterial drug which is used to treat swine dysentery, the use of carbadox could pose a hazard to human health if MRL's are exceeded. Therefore, while antibiotics help ensure control of diarrhoea outbreaks and mortality caused by bacterial infections in pigs, a risk of developing cross-resistance of pathogens to antibiotics used in human therapy is becoming more evident. In Denmark, the public have called for pig producers to stop including antibiotic growth promoters in the rations of pigs weighing more than 30kg. Potassium nitrite and Sodium nitrite have a long history of use as curing agents; nitrate must be converted to nitrite for the curing process to proceed. Nitrite is inhibitory to a range of bacterial pathogens eg: E. coli, and most importantly, spore-forming bacteria such as Clostridium botulinum, which will survive the heat process applied to many cured meats . The antimicrobial effect of nitrite is related to the presence of iron which can bind to Clostridium botulinum and inactivate it. Nitrite also functions as an anti-oxidant in cured meats but there is concern that residual nitrite in the meat poses a risk to human health. In the 1950's it was discovered that N-nitrosamines, formed by the reaction of nitrite with secondary amines, especially at low pH, can be carcinogenic (Adams and Moss, 2000). An increased risk of glioma, and to a lesser extent of meningioma, has been associated in Germany, with cooked ham (Boeing et al., 1993). A case study in Northern Italy also showed a positive relationship between consumption of ham and gastric cancer (La Vecchia et al., 1987). Sodium nitrite is a toxic substance, and at sufficient dose levels is toxic in humans, whose estimated lethal dose is 1g in adults (Ellenhorn et al.,1988). Children are more susceptible to nitrites toxic effects of reduced blood pressure and methaemoglobinaemia. Modern day cured meats have a residual content of 10ppm (Cassens, 1997), however if there is an error in the amount added during production this poses a health threat to the consumer. Other antimicrobials, including anthelminthics such as ivermectin, are used in pigs and as long as withdrawal periods are observed, the muscle concentrations are negligible. Water used in the production process could contain chemical residues eg: chlorine, as could packaging material if there was inaccurate labeling by supplier of non-food grade packaging material. Finally chemical contamination of ham can be caused by cleaning chemicals inadvertently coming into contact with food, or indeed of carcasses from chemicals used on slaughter line i.e. cleaning and maintenance chemicals. A typical example being failure to rinse cleaning chemicals from surfaces or equipment, other examples include spillage or incorrect storage of chemicals. CONCLUSION As the literature review has shown, there are numerous potential hazards associated with ham. However as long as production and processing of pork is carried out with adherence to recognized food safety standards and prerequisites it is still a safe product to consume. In the final analysis, the consumer must be able to trust the producer and ultimately the government agencies responsible for enforcement of the relevant legislation. Consumer confidence is essential to maintain ham at the forefront of the ready-to-eat luncheon meat market. ASKNOWLEDGEMENTS Dr Amalia Scannell, Department of Food Safety, University College Dublin, Dublin 4. Ireland. REFERENCES Adams, M.R. and Moss, M.O. (2000). The Microbiology of Food Preservation. IN: Food Microbiology, Royal Society of Chemistry, Cambridge, U.K. 105-107, 199. Ancelle, T., Dupouy-Camet, J. and Bresson, C. (1989). Study of 39 outbreaks of trichinosis due to consumption of wild boar meat in the Cher ( France ). Bulletin Epidemiologique Hebdomadaire, No. 1, p1-3. Amezquita, A. and Brashears, M.M. (2002). Competitive Inhibition of Listeria monocytogenes in ready-to-eat meat products by lactic acid bacteria. Journal of Applied Bacteriology. 65 (2): 316-325. Atanassova, V., Meindl, A. and Ring, C. (2001). Prevalence of S. aureus and staphylococcal enterotoxins in raw pork and uncooked smoked ham. International Journal of Food Microbiology. 68, (1/2): 105-113. Bager,F., Emborg, H. D., Sorensen, L. L., Haigaard, C. and Jensen, P. T. (1995). Control of Salmonella in Danish pork. Fleischwirtschaft , 75 (8): 1000-1001. Baggensen, D.L., Aarestrup, F. and Molbak, K. (1999). The emergence of nalidixic acid resistant, multiresistant S. typhimutium DT104 in Denmark. An outbreak in humans traced back to pork. Proceedings of the third International Symposium on the Epidemiology and Control of Salmonella in Pork, 191-193. Berends, B.R., Van Knappen, F. and Snijders, J.M.A. (1998a). Salmonella spp. on pork at cutting plants and at the retail level and the influence of particular risk factors. International Journal of food Microbiology, 44, 207-217. Berends, B.R., Van Knappen, F., Mossel, D.A.A., Burt ,S.A. and Snijders, J.M.A. (1998b). Impact on human health of Salmonella spp. on pork in The Netherlands and the anticipated effects of some currently proposed central strategies. International Journal of Food Microbiology, 44, 219-229. Berends, B. R., Van Knapen, F., Snijders, J.M.A. and Mossell, D.A.A. (1997). Identification and quantification of risk factors regarding Salmonella spp. on pork carcasses. International Journal of Food Microbiology, 36, 199-206. Bernard, E ., Ozouf, N., and Marty, P. (1995). Two familial epidemics of trichinosis . Medicine et Maladies Infectieuses. 25 (4): 611-614. Beumer, R. R. and De Boer, E. (1996). Growth of Listeria monocytogenes in sliced cooked meat products. Food Microbiology. 13 (4): 333-340. Boeing , H ., Schlehefer , B., Blettner , M. and Wahrendorf , J. (1993) Dietary carcinogens and the risk for glioma and meningioma in Germany . International Journal of Cancer 20; 53 (4): 561-5 . Bolton, F. J., Dawkin, H. C., Hinchcliff, D. M. and Robertson, L. (1982). Campylobacter jejuni/coli in abbatoirs and butcher shops. Journal of Infection, 4, 243-245. Bolton, D .J ., Pearce, R. and Sheridan, J. J. (2001). Risk-based determination of animal slaughter and food processing critical control points to provide the scientific basis of HACCP. The National Food Centre Research Report (5-7). Bolton, D. J. and Sheridan, J. J. (2001).Pork Slaughter HACCP. HACCP For Irish Pork Slaughter, The National Food Centre, Castleknock, Dublin 15, Ireland. 10-12. Borch, E., Kant-Muermans, M. L. and Blixt, Y. (1996). Spoilage of meat and cured neat products. International Journal of Food Microbiology 33 (1): 103120. Bouvet, J. ,Montet, M. P. and Rossel, R. (2002). Prevalence of verotoxin-producing Escherichia coli VTEC and Escherichia coli O157:H7 in meats obtained from retail outlets in The Netherlands. The Journal of Food Protection 62 (10): 1115-1222. Bredholt, S., Nesbakken, T., Holck, A. (1999).Protective cultures inhibit growth of Listeria monocytogenes and Escherichia coli 0157:H7 in cooked, sliced, vacuum- and gas-packaged meat. International Journal of Food Microbiology, 1: 53(1): 43-52. Brncic-Dabo, N., Rahelic, V. and Vucemilovic, A . (1987). Botulism report of two Outbreaks. Medicina-Rijeka, 23 (2): 65-68. Bryan, F. (1988). Risks Associated with Vehicles of Foodborne Pathogens and Toxins. Journal of Food Protection, 51 (6): 498-508. Carlier, J. P. ,Henry, C., Lorin, V. and Popoff, M. R. (2001). Botulism in France at the end of the second millenium ( 1998-2000 ). Bulletin Epidemiologique Hebdomadaire, ( 9 ): 37-40. Cassens, R. G. (1997) Residual Nitrite in Cured Meat. Food Technology, 51, 53. Cloak, O.M. (1999). The development of rapid methods for the detection of pathogens in meat and poultry. D. Phil. Thesis, University of Ulster. Daniels, N.A Bergmine-Sweat, D.A. and Schwab, K.J. (2000). Foodborne outbreak of gastroenteritis associated with Norwalk-like viruses: first molecular traceback to deli- sandwiches contaminated during preparation. Journal of Infectious Disease 181 (4): 1467 – 70. D’Aoust, J.Y., (1989) Salmonella. Foodborne Bacterial Pathogens. M. P. Doyle (ed). Marcel Dekker Inc., New York. 327-445. Doyle, M.P. and Schoeni, J.L. (1987). Isolation of Escherichia coli O157:H7 from fresh retail meats and poultry. Applied and Environmental Microbiology, 53 (10): 2394 – 2396 . Dubinsky, P., Tomasovicova, O., Turek, P. and Juris, P. (2002). The risk of Trichinella infection due to consumption of meat products. Slovensky Veterinarsky Casopis, 27 (5): 34-37. Duffy, G., Cloak, O.M., O’Sullivan, M.G., Guillet, A., Sheridan, J.J., Blair, I.S. and McDowell, D.A. (1999). The incidence and antibiotic resistance profiles of Salmonella spp. on Irish retail meat products, Food Microbiology, 16: 623-631. Eisenberg, M.S., Gaarslev, K., Brown, W. and Horwitz M. Staphy;ococcal food poisoning aboard a commercial aircraft. The Lancet, 306 (7935): 595-599. Ellenhorn, M.J. and Barceloux, D.G. (1988). Nutritional toxicology. IN: Medical Toxicology . Elsevier, New York, U.S.A. 88-92. Epling, L.K., Carpenter, J.A. and Blakenship, L.C. (1993). Prevalence of Campylobacter spp. and Salmonella spp. on pork carcasses and the reduction effected by spraying with lactic acid. Journal of Food Protection, 56 (6): 536537. Esposito, M., Imporoto, E., Castellero, V. and Serpe, L. Distribution of polychlorinated biphenyls in contaminated swine tissue. Veterinary and Human Toxicology, 43 (2): 97-98. Food Safety Authority of Ireland, (1999). The prevention of Escherichia coli O157:H7 infection. IN: VTEC –An Emerging Threat, Food Safety Authority of Ireland, Dublin, Ireland. 8-10. Food Safety Authority of Ireland, (2003). National microbiology surveillance programme. IN: Annual Report 2002, Food Safety Authority of Ireland, Dublin, Ireland. 10-12. Fukushima, H., Hoshina, K., Nalamura, R. and Ito, Y. (1987 ). Occurrence of Yersinia spp. in raw beef , pork and chicken. Zentralblatt fur Bakteriologie Mikrobioogie un Hygiene, 184, 50-59. Gammie, A.J., Mortimer, P.R , Hatch, L., Brierley, A.F.M. and Wallers, J.B. (1996). Outbreak of verocytotoxin-producing Escherichia coli O157 associated with cooked ham from a single source. PHLS Microbiology Digest, 13( 3): 142-145. Haeghebaert, S. ,Carlier, J.P. and Popoff, M. (2003). Epidemiological characteristics of human botulism in France, 2001 and 2002. Bulletin Epidemiologique Hebdomadaire. (29): 129-130. Hald, T. and Wegener, H.C. (1999). Quantitative assessment of the sources of human salmonellosis attributable to pork. Proceedings of the Third International Symposium on the Epidemiology and Control of Salmonella in Pork. Urbana-Champaign (IL) : University of Illinois, Washington D.C.,U.S.A. 4-7 August, 200-205. Ham, J.S., Kim, H.J., Hong, K.H. and Kim, J.G. (2003). Inhibitory activity of lactic acid bacteria against hazardous microbes. Asian-Australian Journal of Animal Science, 16(10): 1550-1554. Heuvelink, A.E., Zwartkruis–Nahuis, J.T.M., Beumer, R.R. (1999). Occurrence and survival of verocytotoxin-producing Escherichia coli O157 in meats obtained from retail outlets in The Netherlands. Journal of Food Protection, 62 (10): 115-122 . Korsak, N., Daube, G., Ghafir, Y., Chahed, A., Jolly, S. and Vindevogel, H. ( 1998) An efficent sampling technique used to detect four foodborne pathogens on pork and beef carcasses in nine Belgian abbatoirs. Journal of Food Protection, 61 (5): 535-541. Krovacek, K.. Dumantet, S., Eriksson, E. and Baloda, S.B., (1995 ). Isolation and virulence profiles of Aeromonas hydrophila implicated in an outbreak of food poisoning in Sweden. Microbiology Immunology, 39 (9): 655-61. La Vecchia, C., Negri, E., Decarli, A., D’Avanzo, B. and Franceschi, S. (1987). A case-control study of the diet and gastric cancer in northern Italy. International Journal of Cancer, 40(4): 484-9. Lecour, H., Ramos, M.H., Almeida, B. and Barbosa, R. Food-borne botulism: a review of 13 outbreaks. Archives of Internal Medicine, 148 (3): 578-580. Lyytikainen, O., Koort, J., Ward, l., Schildt, R., Ruutu, p., Japisson, E., Timonen, M. and Siitonen, A. (2000). Molecular epidemiology of an outbreak caused by Salmonella enterica serovar Newport in Finland and the United Kingdom. Epidemiology Infections, 124 (2): 185-92. Mayrhofer, S., Paulsen, P., Smulders, F.J.M. and Hilbert, F. (2004). Antimicrobial resistance profile of five major foodborne pathogens isolated from beef, pork and poultry. International Journal of Food Microbiology (article in press ). Mertens, P.L., Thissen, J.F., Houben, A.W. and Sturmans, F. (1999). An epidemic of Salmonella typhimurium associated with traditional, salted, smoked and dried ham. Ned Tydschr Geneeskd. 143 (20): 1046-9. Narain, J.P. and Lofgren, J.P. (1989). Epidemic of restaurant associated illness due to Salmonella newport. South Medical Journal, 82 (7): 837-40. Nesbakken, T., Nerbrink, E., Rotterud, O.J. and Borch, E. (1994 ). Reduction of Yersinia enterocolitica and Listeria spp. on carcassses by enclosure of the rectum during slaughter. International Journal of Food Microbiology, 23 (3): 197-208. Noah, T.M. (1997). Hospital outbreak poisoning. Lancet, 1 (8020): 1046-8. of Clostridium perfringens food Oosterom, J., Den Uyl, C.H. Banffer, J.R.J., Lauwers, S., Huisman, J., Busschbach, A.E., Porlma, F.G.J. and Bellmans, R. (1985). Evaluation of an enzyme linked immunosorbent assay for the detection of Campylobacter jejuni antibodies and comparison with a complement fixation test (CFT). Antonie van Leeuwenhoek, 51: 321-331. O’Keefe, M., Kennedy, O., Farrell, F., Nolan, M., Dooley, M., Byrne, P., Nugent, A., Cantwell, H., Nelson, V., McGrath, D., (2001). Polycylic Aromatic Hydrocarbons IN: Food Residue Database, The National Food Centre, Dunsinea, Castleknock, Dublin15, Ireland. 6, 9-17. Portocarrero, S.M., Newman, M., Mikel, B. (2002a). Reduction of Listeria monocytogenes, Salmonella spp., and Escherichia coli O157:H7 during processing of country-cured hams .Journal of Food Science. 67(5): 1892-1898. Portocarrero, S.M., Newman, M. and Mikel, B. (2002b). Staphyloccocus aureus survival, staphyloccocal enterotoxin production and shelf stability of countrycured hams manufactured under different processing procedures . Meat Science, 62 (2): 267-273. Rajkowski, K.T., Rice, R.W. (1999). Recovery and survival of Escherichia coli O157:H7 in reconditioned pork-processing wastewater. Journal of Food Protection, 62 (7) : 731-734. Richards, M.S., Goarslev, K., Brown, W. and Harwitz, M. (1993). Investigation of a staphyloccocal food poisoning outbreak in a centralized school lunch program. Public Health Reports, 108(6): 765-771. Riordan,T., Craske, J., Roberts, J.L. and Curry, A. (1984). Food-borne infections by a Norwalk-like virus (small round structured virus ). .Journal Clinical Pathology, 37(7): 817-20. Roblot, P. , Roblot, F. and Fauchere, J.L. (1994). Retrospective study of 108 cases of botulism in Poitiers, France. Journal of Medical Microbiology, 40 (6): 379. Rocourt, J., Goulet, V. and Lepoutretouleman, A. (1993). Outbreak of Listeriosis in France, 1992. Medicines et Maladies Infectieuses, 23: 481-484. Salvat, G., Toquin, M.T. and Michel, Y. (1995). Control of Listeria monocytogenes in the delicatessen industries: the lessons of Listeriosis outbreak in France. International Journal of Food Microbiology, 25(1): 75-81. Sheridan, J.J., Duffy, G., McDowell, D.A. and Blair, I.S. (1994). The occurrence and initial numbers of Listeria in Irish meat and fish products and the recovery of injured cells from frozen products .International Journal of Food Microbiology, 22: 105-115. Szymanska, L., and Medrala, D. (2003). Listeria monocytogenes in meat , meat products and meat processing environment. Medycyna Weterynaryjna, 59(1): 7581. Terlevic, E., Maretic, Z. and Beus, I. (1998). Botulism epidemic in Istria in 1985. Giornale di Malattie Infettive e Parassitarie, 40(4): 300-303. Thornton, L., Gray, S., Bingham, P., Hutchinson, D.N., Rowe, B., Newton, D. and Syed, Q. (1993). The problems of tracing a geographically widespread outbreak of Salmonellosis from a commonly eaten food-Salmonella Typhimurium DT193 in North-West England and North Wales in 1991. Epidemiology and Infection, 111(30): 465-471. Ward, K., Hammond, R., Katz, D. and Hallman, D. (1997). Outbreak of Staphyloccocal food poisoning associated with pre-cooked ham – Florida 1997. Morbidity and Mortality Weekly Report, 46(50): 1189-1191. Whyte, P., McGill, K., Cowley, D. and Madden, R.H. (2004). Occurrence of Campylobacter in retail foods in Ireland. International Journal of Food Microbiology, 9(2): 111-118. World Health Organisation (W.H.O.),(1992). Report of the Panel on Food and Agriculture. WHO commission on Health and Environment, 92(2): 191-193. Wu, M. T., Ayres, J.C. and Koehler, P.E. (1974) Production of Citrinin by Penicillium viridicatum on Country-cured Ham. Applied Microbiology, 27(20): 427-428. Vukovic, I. (2000). Botulism in Yugoslavia and possibilities of prevention. Tehnologija Mesa, 41(113): 19-29.