MED - Department of Surgery - University of Minnesota Twin Cities
advertisement

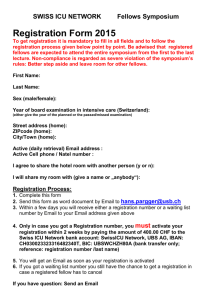
UNIVERSITY OF MINNESOTA GRADUATE MEDICAL EDUCATION 2011-2012 FELLOWSHIP POLICY & PROCEDURE ADDENDUM Department of Surgery Surgical Critical Care Fellowship Program Websites: www.med.umn.edu/gme/central www.surg.umn.edu www.surg.umn.edu/surgery/Divisions/SICU/home.html Orig. 5/9/11 Confirmation of Receipt of your Fellowship Addendum for Academic Year 2011-2012 By signing this document you are confirming that you have received and reviewed your Fellowship Addendum for this academic year. This policy manual contains policies and procedures pertinent to your training program. This receipt will be kept in your personnel file. Fellow Name (Please print) _______________________________________________ Fellow Signature ________________________________________________________ Date __________________ Coordinator Initials ________________ Date __________________ 2 Table of Contents INTRODUCTION Introduction ......................................................................................................................................6 Department of Surgery Mission Statement ......................................................................................7 Surgical Critical Care Fellowship Program Mission Statement ......................................................7 SECTION 1. STUDENT SERVICES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Academic Health Center (AHC) Portal Access; Child Care; Computer Discount/University Bookstore; Credit Union; Disability Accommodations; Legal Services; Library Services; Medical School Campus Maps; Nursing Mothers Resources; Resident Assistance Program; University Card (UCard); University Events Box Office; University Recreation Sports Center(s)) Universal University Pagers ............................................................................................................8 Email and Internet Access ...............................................................................................................8 University Mailboxes and Campus Mail .........................................................................................9 Laboratory Coats ..............................................................................................................................9 UMMC-F Photo ID Badge...............................................................................................................9 HIPAA Privacy Regulations ............................................................................................................9 SECTION 2. BENEFITS (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Insurance: Dental Insurance; Health Insurance; Life Insurance; Voluntary Life Insurance; Long-Term Disability; Short-Term Disability; Insurance Coverage Changes; Immunization Services; Exercise Room at UMMC-FV; Bereavement Leave; Family Medical Leave Act (FMLA); Holidays; Medical Leave; Military Leave; Parental Leave; Personal Leave; Professional Leave; Vacation/Sick Leave; Witness/Jury Duty; Effect of Leave for Satisfying Completion of Program; Loan Deferment; Loan Program: Emergency Loan Program through Minnesota Medical Foundation; Minnesota Medical Association Membership; Professional Liability Insurance; Stipends; Veterans Certification for Education Benefits; Workers’ Compensation Benefits). Stipends ................................................................................................................................... 10 Health and Dental Insurance Coverage....................................................................................10 Long Term Disability Insurance ..............................................................................................11 Short Term Disability Insurance ..............................................................................................11 Professional Liability Insurance ..............................................................................................11 Life Insurance ..........................................................................................................................11 Meal Tickets.............................................................................................................................11 Parking .....................................................................................................................................11 Policy on Effect of Leave for Satisfying Completion of Program...........................................12 Vacation Policy ........................................................................................................................12 Professional and Academic Leave .....................................................................................12 Parental Leave ....................................................................................................................12 Sick Leave Policy ..............................................................................................................12 SECTION 3 - INSTITUTION RESPONSIBILITIES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: ACGME Resident Survey Requirements; ACGME Site Visit Preparation 3 Services; Master Affiliation Agreements or Institution Affiliation Agreements; Program Letters of Agreement; Confirmation of Receipt of Program Policy Manuals; Designated Institution Official Designee Policy; Duty Hour Monitoring at the Institution Level Policy and Procedure; Experimentation and Innovation Policy; Funding; GME Competency Teaching Resources and Core Curriculum; Graduate Medical Education Committee (GMEC) Responsibilities; Graduate Medical Education Committee Resident Leadership Council Responsibilities; Institution and Program Requirements; Internal Review Process; International Medical Graduates Policy; New Program Process; Orientation; Visa Sponsorship Policy). ...................................................................................... 13 SECTION 4 - DISCIPLINARY AND GRIEVANCE PROCEDURES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Discipline/Dismissal/Nonrenewal; Conflict Resolution Process for Student Academic Complaints; University Senate on Sexual Harassment Policy; Sexual Harassment and Discrimination Reporting; Sexual Assault Victim’s Rights Policy; Dispute Resolution Policy) 13 SECTION 5 - GENERAL POLICIES AND PROCEDURES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Academic Health Center (AHC) Student Background Study Policy; Background Study Policy and Procedure; Academic Incivility: Resources for Dealing with Harassment; Applicant Privacy Policy; Appointment Letter Policy and Procedure; Blood Borne Pathogen Exposure Policy; Certificate of Completion Policy; Classification and Appointment Policy; Compact for Teaching and Learning; Disability Policy; Disaster and Local Extreme Emergent Situation Planning Policy and Procedure; Documentation Management Requirements Policy; Dress Code Policy; Duty Hours/On-Call Schedules; Duty Hours Policy; Duty Hours/Prioritization of On-Call Room Assignments; ECFMG/J1 Visa Holders: Documentation Required for FMLA; Effective Date for Stipends and Benefits Policy; Eligibility and Selection Policy; Essential Capacities for Matriculation, Promotion and Graduation for U of M GME Programs; Evaluation Policy; Health Insurance Portability and Accountability Act; Immunizations and Vaccinations; Immunizations: Hepatitis B Declination Form; Impaired Resident/Fellow Policy and Procedure; Licensure Policy: Life Support Certification Policy; Moonlighting Policy; National Provider Identification (NPI) Policy and Procedure; National Residency Matching Program (NRMP) Fees Policy; Nepotism Policy; Observer Policy; Post Call Cab Voucher Policy (UMMC-F; HCMC); Registered Same Sex Domestic Partner Policy; Release of Contact Information for Solicitation Purposes Policy; Residency and Fellowship Agreement Policy and Procedure; Residency Management Suite (RMS): Information Maintenance for Participating Hospitals; Residency Management Suite (RMS): Updating and Approving Assignments and Hours in the Duty Hours Module of RMS; Restrictive Covenants; Social Networking Policy; Standing and Promotion Policy; Stipend Level Policy; Stipend Funding from External Organizations Policy; Supervision Policy; Trainee File and Document Retention Policy; Training Program and/or Institution Closure or Reduction Policy; Transitional Year Policy; USMLE Step 3 Policy; Vendor and Conflict of Interest Policy; Verification of Training and Summary for Credentialing Policy; Without Salary Appointment Policy ). Program Goals and Objectives.................................................................................................14 Training and Graduation .................................………………………………………………14 Residency Program Curriculum ...............................................................................................15 ACGME Competencies ...........................................................................................................16 Duty Hours Policy....................................................................................................................19 Resident Duty Hours and the Working Environment ..............................................................19 On-Call Schedules ...................................................................................................................21 Resident Supervision Policy ....................................................................................................21 Graded Responsibility..............................................................................................................24 Support Services (Facilities & Resources) ..............................................................................24 UMMC On Call Rooms ...........................................................................................................25 UMMC Resident Lounge .........................................................................................................25 Laboratory/Pathology/Radiology Services ..............................................................................25 Medical Records ......................................................................................................................26 Security/Safety .........................................................................................................................26 4 Monitoring of Resident Well-Being ........................................................................................26 Communication Policy.............................................................................................................27 Grand Rounds Compliance ......................................................................................................27 Dress Code Policy ....................................................................................................................27 Moonlighting............................................................................................................................28 American Board of Surgery - Requirements for Certification in Surgery ...............................28 Evaluations and RMS ..............................................................................................................29 Patient Log ...............................................................................................................................29 Resident Rotation Dates ...........................................................................................................31 SECTION 6 - ADMINSTRATION (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: GME Administration Contact List, GME Administration by Job Duty; GME Organization Chart) Administrative Contact List ...........................................................................................................31 5 Introduction This Fellowship Addendum refers to policies and procedures specific to your training program. Please refer to the Institution Manual and the Program Policy Manual for your Department for further policies and procedures on the following: Student Services; Benefits; Disciplinary and Grievance Procedures; General Policies and Procedures; Administration. For information that applies to all residency/fellowship training programs at the University of Minnesota, please consult the Institution Manual. Information in the Institution Manual takes precedence over that in the Program Manual and Fellowship Addendum, in cases where there is conflict. All manuals are available online: Institution Manual: http://www.med.umn.edu/gme Program Manual & Addendum: www.surg.umn.edu/surgery/Divisions/SICU/home.html 6 Department of Surgery Mission Statement The mission of the Department of Surgery is teaching, research, and provision of excellent clinical service. The primary academic mission is to teach medical students, residents and fellows, and advanced degree candidates with the focus of developing academic surgeons and advancing knowledge in surgical specialties through scientific and clinical research endeavors. Surgical Critical Care Fellowship Program Mission Statement Provide high quality, humane care to critically-ill surgical patients. Provide a high quality educational experience for residents and medical students in the care of the critically-ill surgical patient. Continue the tradition of excellence in the training and continuing education of physicians with a special interest in critical care. Provide an environment for performance of high quality research designed to improve our understanding of the pathophysiology of the critically-ill surgical patient and the treatment and care of this patient population. 7 SECTION 1 - STUDENT SERVICES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Academic Health Center (AHC) Portal Access; Child Care; Computer Discount/University Bookstore; Credit Union; Disability Accommodations; Legal Services; Library Services; Medical School Campus Maps; Nursing Mothers Resources; Resident Assistance Program; University Card (UCard); University Events Box Office; University Recreation Sports Center(s) Universal University Pagers Your UMMC-F pager assigned to you remains the same for the duration of your training. Do not turn it in when you rotate off site. For malfunctioning pagers please contact Debbie in the Surgical Critical Care Office or during off hours go to the UMMC-Fairview main Information Desk for assistance. New batteries can be obtained from the Surgical Critical Care Office, 11-115 PWB Bldg. E-mail and Internet Access To set up e-mail account: Check to make sure you are registered as a student (all surgical residents are registered students at the University of Minnesota). You can do this by going to the U of MN-Twin Cities home page at http://www1.umn.edu/twincities/. Click on Search icon. Under search for people, type in your name and click on search. If you are not registered, you won’t be in the system. If you are not registered, please contact the Surgical Education Office at 612-625-3926 to make sure all of your paperwork is complete. Call the e-mail helpline at 612-301-4357, or go to the Computer Information Services Office in Room 152 Shepherd Laboratories, 100 Union Street, to set up your account and password. To access your e-mail account: Any computer with Internet access can be used to access your email. (See below for setting up access from home.) Go to http://www.mail.umn.edu/ (if you forget this address, there is a link to this page on the Department of Surgery home page at http://www.surg.umn.edu ). Click on Check your e-mail via your Web browser. Enter your X500 ID, NOT YOUR EMAIL ADDRESS. Ex: If your e-mail address is smith999@ umn.edu, your X500 ID is smith999. Enter your password. Click on Login. To set up Internet access from home: - Faculty, staff, and students at the University of Minnesota can purchase internet kits from any of the three walk-in locations of the Academic & Distributed Computer Services: 152 Shepherd Labs (East Bank), 93 Blegen Hall (West Bank), or 50 Coffey Hall (St. Paul), or from the Bookstore Computer Store in Coffman Memorial Union. - You will need to bring a photo ID with you, preferably your U Card. - The cost of the kits is $6.00, and they accept cash or checks only. 8 - The kits are available on CD. - The Internet kit on CD contains software and installers for Windows 95/98/NT4, Windows 2000, XP and Macintosh, as well as other useful programs and utilities. More information about the internet kits can be found at http://www1.umn.edu/adcs/help/kits.html University Mailboxes and Campus Mail Mailboxes have been assigned to you. They are located in the Fellows cubicle in 11-115 PWB. It is essential that you pick up your mail at least weekly. These boxes are not locked. Your campus mail address is 420 Delaware St. SE, MMC 11, Minneapolis, MN 55455. Laboratory Coats and Laundry Service Lab coats can be purchased through the University of Minnesota Bookstore, located in Coffman Memorial Union, or from an outside agency. Be sure to have your name and department stitched over the breast pocket if coats will be laundered by the hospital. Soiled coats can be dropped off in the hamper near the Surgery Department on the 11th floor PWB, not in the hospital. Christine Vincent has the key to the closet. Clean coats may be picked up one to two weeks later from the Labcoat Closet. To comply with Fairview requirements, lab coats should not contain any other institution name. UMMC-F Photo ID Badge You can obtain a UMMC-F photo ID badge on either the Riverside campus or the University campus. To obtain a badge on the Riverside campus go to the Main Security Office, M141 East Building. They are open 24 hours a day, 7 days a week. To get there, board the Fairview shuttle to the Riverside campus--you may obtain the schedule from the UMMC-F Information Desk. The shuttle drops you off at the East Building. Go in the entrance and follow the signs to the Main Security Office. The office will have a list of Department of Surgery residents. You will be required to fill out a form giving your name, address, Social Security Number, etc. On the University campus, go to B-340 Mayo. They are open Thursdays from 12:00 PM to 5:00 PM and Fridays from 7:00 AM to 12:00 PM. You must have either a driver’s license or state ID AND a resident verification form. You will receive your badge right away if you go to the Riverside campus. If you go to the University campus, it will be sent to you. For further information, call 612-672-4544. HIPAA Privacy Regulations In order to be in compliance with HIPAA privacy regulations, every University of Minnesota student, faculty member, researcher, and staff person are required to complete at least four on-line courses about privacy and data security. To access training, log on to http://www.myu.umn.edu . Everyone will need to complete the following three courses: The Video Awareness course The Privacy and Confidentiality in the Clinical Setting course The Privacy and Confidentiality in Research course Accessing the Online HIPAA Courses 1. Go to http://www.myu.umn.edu 9 2. Select “Click here to Sign-in”, located in the upper left hand corner of the portal homepage. 3. Authenticate using your U of M Internet ID and password. 4. Confirm that authentication was successful by looking for the “Signed in as (your name)” in the upper left hand corner where you selected “Click here to Sign-in”. 5. Select my Toolkit. 6. Go to the section titled “(Your Name) Projects To Do lists”. 7. Look for the title of the training course that you need to complete. Select the course and a new window will open up. You can begin taking the course. 8. After you complete the course, close the window to return to your To Do list. You can then proceed with the next course or if you are finished, you can log out of the portal. 9. If you have to quit the training in the middle of a course that is in WebCT, you can go back into the course and select the “Resume Course” button in the upper navigation to get back to the page you were on. 10. You will receive an email confirming your completion of the course. Print out the confirmation for your records. Your completion of the courses will be tracked electronically. 11. Please remember to LOG OUT of the portal when you are finished. If you leave the computer while you are logged in, others could use your log in to access your private information such as HR information SECTION 2 - BENEFITS (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Insurance: Dental Insurance; Health Insurance; Life Insurance; Voluntary Life Insurance; Long-Term Disability; Short-Term Disability; Insurance Coverage Changes; Immunization Services; Exercise Room at UMMC-FV; Bereavement Leave; Family Medical Leave Act (FMLA); Holidays; Medical Leave; Military Leave; Parental Leave; Personal Leave; Professional Leave; Vacation/Sick Leave; Witness/Jury Duty; Effect of Leave for Satisfying Completion of Program; Loan Deferment; Loan Program: Emergency Loan Program through Minnesota Medical Foundation; Minnesota Medical Association Membership; Professional Liability Insurance; Stipends; Veterans Certification for Education Benefits; Workers’ Compensation Benefits). Stipends Resident/fellows will be paid a yearly stipend as stated in the offer letter and in the Program Manual. Residents/fellows will receive a paycheck biweekly. Residents/fellows are encouraged to use the direct-deposit system, as paychecks have the potential of being lost or delayed in the mail. University of Minnesota Medical School, Graduate Medical Education 2011-2012 Base Stipend Rates Level: G6 Annual Base Stipend: $57,620 The University of Minnesota payroll is a 10-day delayed start system, paid every 2 weeks. Health and Dental Insurance Coverage See the Institution Manual. Benefits are handled by the Office of Student Health Benefits. Their website is http://www.shb.umn.edu . They can be reached at 624-0627. 10 Long Term Disability Insurance See the Institution Manual. Benefits are handled by the Office of Student Health Benefits. Their website is http://www.shb.umn.edu . They can be reached at 624-0627. Short Term Disability Insurance Short Term disability insurance is offered as an optional coverage. The cost is based on the amount of coverage elected. Coverage may be applied to in increments of $100 from a minimum of $300 to a maximum of $5000, but not to exceed 2/3 of the fellow’s monthly gross salary. Benefits are effective the first day of a disability due to an accident or the eighth day of disability due to sickness or pregnancy and, if certified, can continue for up to 26 weeks. Professional Liability Insurance See the Institution Manual for information. The web address is http://www.med.umn.edu/gme/residents/instpolicyman/home.html for contact information.. Life Insurance See the Institution Manual. Benefits are handled by the Office of Student Health Benefits. Their website is http://www.shb.umn.edu . They can be reached at 624-0627. Meal Tickets Meal Tickets will be provided for you on all regular rotations (excludes elective rotations). Meal tickets are electronic in the UMMC and Riverside cafeteria and can be obtained from Debbie in the critical care administrative office 11-115b; at the VA, the kitchen has a list of who is on call; and at Regions, the Surgical Education Office will provide you with preprogrammed meal cards. At all other sites, the on-site Education Office will provide you with the details of your meal allowances. Parking Paid parking is provided to fellows while they are officially rotating at the site. Paid parking may or may not be available while participating in an elective rotation at the U. Fellows rotating at the University of Minnesota site are provided with a parking card for the Oak St. ramp to use during their rotation. The card must be turned in to Debbie or Colleen in the administrative office on the last day of the University SICU rotation so it is available for the next fellow. There are two options for parking at the V.A. Medical Center. There is an open employee lot and a gated physician parking area. The VA ID badge allows access to parking in the gated lot. At Regions Hospital, ID badges are obtained the first day of rotation. The badge allows free parking in the ramp or open lot and can be retained for the duration of the fellowship year. The Regions’ badge should be turned in to Debbie in 11-115b PWB Bldg. on the last day in the fellowship program. At HCMC, fellows should contact Phyllis Squiers to obtain a parking pass for the hospital ramp at the corner of 8th and Chicago. 11 At NMMC, free parking is provided to fellows in the Oakdale Parking Ramp (off Hwy 81 and Abbott). When not on service at UMMC, parking is provided for you in the Washington Avenue Ramp when attending SICU Journal Clubs and Quarterly Educational Meetings. Policy on effect of Leave for Satisfying Program Requirements ACGME requirements state that an accredited surgical critical care program shall be 12 months, of which two months may be elective rotations. Any leave that results in an educational experience of less will need to be extended in order to successfully complete the program and be eligible to take the exam for Added Qualifications in Critical Care. Vacation Requests Three weeks of vacation per year are allowed for fellows. Fellows must complete an “SICU Fellow Vacation Request” form which can be obtained from the Critical Care website www.surgery.umn.edu/Divisions/SCC and receive approval from the Site Director at the location they are rotating at and the Director of the Program. Every effort will be made to accommodate reasonable requests. Vacations are discouraged during the last two weeks of the fellowship. Professional and Academic Leave Fellows are required to attend the Society of Critical Care Medicine’s annual meeting. Currently, funding is provided for reasonable travel related expenses. Please contact Debbie in 11-115b PWB Bldg. for assistance in making travel arrangements and completing the necessary paperwork. Funded travel for other meetings is on a per case basis and at the discretion of the Fellowship Director. Family Medical Leave Policy/Childbirth or Adoption A leave of absence for serious illness of the resident/fellow, serious health condition of a spouse, parent, or child, or birth or adoption of a child, shall be granted through formal request to the program director. The length of the leave will be determined by the program director based upon an individual’s particular circumstances and the needs of the department, not to exceed 12 weeks in any 12-month period. The resident/fellow shall be granted, upon request, up to 6 weeks paid maternity leave for birth or 2 weeks paid leave for adoption. After using paid maternity leave and all unused vacation, any additional leave will be without pay. Two weeks paid paternity leave will be granted upon request to the program director. Estimated periods for Family Leave must be submitted to the Surgical Education Office at the time the circumstances necessitating leave arise. Nursing mothers have access to lactation rooms on both the University and Riverside campuses. If rotating at another site, contact the Medical Staff office for locations. Riverside: East Bldg., 5th floor, Room M555 University: Main Hospital, 4th floor, Room 4-106 Sick Leave Policy In the event of illness, the affected resident/fellow is personally responsible for notifying the faculty member of the affected service and the Surgical Education Office or Fellowship Director’s Office as soon as the resident/fellow knows that the illness will cause an absence from clinical responsibilities. Sick leave will be approved only for legitimate illness. A physician’s note may be requested to support the resident/fellow’s request for sick leave. If the above policy is not followed, the absence will be counted as vacation time. It is the responsibility of the resident and the program director to ensure that Board eligibility requirements are met within the original residency period or alternative arrangements are made. 12 SECTION 3 - INSTITUTION RESPONSIBILITIES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: ACGME Resident Survey Requirements; ACGME Site Visit Preparation Services; Master Affiliation Agreements or Institution Affiliation Agreements; Program Letters of Agreement; Confirmation of Receipt of Program Policy Manuals; Designated Institution Official Designee Policy; Duty Hour Monitoring at the Institution Level Policy and Procedure; Experimentation and Innovation Policy; Funding; GME Competency Teaching Resources and Core Curriculum; Graduate Medical Education Committee (GMEC) Responsibilities; Graduate Medical Education Committee Resident Leadership Council Responsibilities; Institution and Program Requirements; Internal Review Process; International Medical Graduates Policy; New Program Process; Orientation; Visa Sponsorship Policy). SECTION 4 - DISCIPLINARY AND GRIEVANCE PROCEDURES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Discipline/Dismissal/Nonrenewal; Conflict Resolution Process for Student Academic Complaints; University Senate on Sexual Harassment Policy; Sexual Harassment and Discrimination Reporting; Sexual Assault Victim’s Rights Policy; Dispute Resolution Policy) SECTION 5 - GENERAL POLICIES AND PROCEDURES (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: Academic Health Center (AHC) Student Background Study Policy; Background Study Policy and Procedure; Academic Incivility: Resources for Dealing with Harassment; Applicant Privacy Policy; Appointment Letter Policy and Procedure; Blood Borne Pathogen Exposure Policy; Certificate of Completion Policy; Classification and Appointment Policy; Compact for Teaching and Learning; Disability Policy; Disaster and Local Extreme Emergent Situation Planning Policy and Procedure; Documentation Management Requirements Policy; Dress Code Policy; Duty Hours/On-Call Schedules; Duty Hours Policy; Duty Hours/Prioritization of On-Call Room Assignments; ECFMG/J1 Visa Holders: Documentation Required for FMLA; Effective Date for Stipends and Benefits Policy; Eligibility and Selection Policy; Essential Capacities for Matriculation, Promotion and Graduation for U of M GME Programs; Evaluation Policy; Health Insurance Portability and Accountability Act; Immunizations and Vaccinations; Immunizations: Hepatitis B Declination Form; Impaired Resident/Fellow Policy and Procedure; Licensure Policy: Life Support Certification Policy; Moonlighting Policy; National Provider Identification (NPI) Policy and Procedure; National Residency Matching Program (NRMP) Fees Policy; Nepotism Policy; Observer Policy; Post Call Cab Voucher Policy (UMMC-F; HCMC); Registered Same Sex Domestic Partner Policy; Release of Contact Information for Solicitation Purposes Policy; Residency and Fellowship Agreement Policy and Procedure; Residency Management Suite (RMS): Information Maintenance for Participating Hospitals; Residency Management Suite (RMS): Updating and Approving Assignments and Hours in the Duty Hours Module of RMS; Restrictive Covenants; Social Networking Policy; Standing and Promotion Policy; Stipend Level Policy; Stipend Funding from External Organizations Policy; Supervision Policy; Trainee File and Document Retention Policy; Training Program and/or Institution Closure or Reduction Policy; Transitional Year Policy; USMLE Step 3 Policy; Vendor and Conflict of Interest Policy; Verification of Training and Summary for Credentialing Policy; Without Salary Appointment Policy ). Introduction Welcome to the University of Minnesota Surgical Critical Care Program. Your educational experience will be based on several approaches to give you the background necessary to complete a fellowship in surgical critical care: 1. 2. 3. 4. Organized didactic experiences Self study of core materials Directed and self-study of current critical care literature Patient care experience at an advanced level 13 Specific learning objectives are addressed in each site’s “specific goals and objectives”. Each of these topics will be addressed by didactic teaching, self-study, and teaching on rounds. You will be evaluated during each rotation and overall in several ways: 1. You are expected to display mastery of the material as evidenced by its accurate application in the patient care setting; 2. You are expected to be able to teach mastered material to residents and students during clinical teaching rounds; 3. You are expected to perform at least at the 50th percentile on the critical care in-service exam (MCCKAP). 4. You are expected to pass the American Board of Surgery exam in Surgical Critical Care. The core Surgical Critical Care core curriculum is based on literature readings and Abrams’ Surgical Critical Care, 2nd edition. This book is available as an e-book through the University Library System SURGICAL CRITICAL CARE FELLOWSHIP TRAINING PROGRAM A. Goals and Objectives: Fellowship requirements are outlined below and correspond with the requirements of the ACGME, “Program Requirements for Residency Education in Surgical Critical Care” and “Program Requirements for Residency Education in the Subspecialties of General Surgery”, and “Common Program Requirements”. In addition, site specific requirements are outlined in the handouts entitled, “SICU Fellows: U of M Rotation, “SICU Service – University of Minnesota Medical Center - Fairview”, “SICU Fellows: VA Rotation”, “Regions Medical Center Surgical ICU Service: Goals and Objectives”, “Hennepin County-SICU Service”, and “NMMC TNICU Goals and Objectives”. Fellows are required to take the Multidisciplinary Critical Care Assessment Program (MCCKAP) exam during the last half of their fellowship year. This exam is used as a tool to assist fellows in preparation for the American Board of Surgery’s Surgical Critical Care Exam. B. Training/Graduation Requirements 1. The subspecialty program in surgical critical care medicine is 1 year in duration (with an optional additional research year) and contains all of the educational experiences and program content required for an accredited training program. A certificate of completion is awarded to all fellows who successfully complete their clinical year as determined by evaluations assessing their organizational, technical, clinical, interpersonal/communication, and administrative/management skills. Upon completion, board certified fellows are eligible to take the exam for Added Qualifications in Critical Care. 2. The clinical experience includes opportunities to manage inpatients with a wide variety of diseases. The trainee will assume continuing responsibility for acutely and chronically ill patients. 3. There are 12 months of direct patient care responsibility in critical care units. You will spend 3 months at critical care units at University of Minnesota Medical Center, 2 months at Regions Hospital (a Level I trauma center), 2 months at Hennepin County Medical Center (a Level I trauma center), 2 months at North Memorial Medical Center, and 1 month at the V.A. Medical Center. 14 4. There is the option of 2 months of elective time during the 12-month clinical year. This elective time may consist of electives in medical critical care, research, pediatric critical care, neonatal intensive care, echocardiography, trauma, and burn care. 5. The primary training site for the University of Minnesota program is the University of Minnesota Medical Center. This site features accredited subspecialty programs in pulmonary critical care, cardiovascular surgery, transplantation and surgical infectious diseases, as well as general surgery. There will be extensive formal and informal interactions among trainees in these accredited programs and the Surgical Critical Care Program. 6. The trainees will have extensive exposure to the care of surgical patients at all sites and trauma patients, at Regions Medical Center, North Memorial Medical Center and Hennepin County Medical Center, during their training program. 7. The University of Minnesota has policies in place that ensures appropriate educational resources will be devoted to surgical critical care training. C. Curriculum/Specific Program Content Didactic Teaching Didactic conferences consist of site-specific conferences (outlined in each site description) and programwide conferences. Program-wide Conferences a. At the Tuesday ICU Conference, speakers cover specific critical care topics and highlight areas where fellows have scored lower on the MCCKAP exam in previous years. b. Monthly journal club occurs the 1st Wednesday of the month. Articles are assigned for review by critical care fellows. Topics and cases are also presented. (Topics are chosen based on identified need, as mentioned above.) c. Quarterly ICU meetings involve a forum for program issues to be presented and program suggestions/improvements discussed. Meetings are hosted by a different site each time, except for the last meeting in June. The June meeting is split into two parts. The first part includes the fellows and consists of a review and evaluation of the year. The second half is without the fellows and consists of a review of faculty evaluations completed by the fellows and a review of the entire program by the faculty. Any changes for the following year are discussed. d. SCCM Annual Meeting: Fellows must attend; critical care section will usually sponsor fellows. e. The last Wednesday of the month is a combined Pulmonary/Surgical Critical Care Conference: The conference covers RRC required topics and is directed by faculty from UMMC-F, HCMC, Regions, NMMC and the MINNEAPOLIS VA HEALTH CARE SYSTEM. Fellows will be expected to do a case presentation approximately every 6 months for this conference. Self Study The textbook used for this fellowship is Abrams’ Surgical Critical Care, 2nd edition (available either at the University Bookstore or as an e-book from the University Library). In addition, each site has specific readings (included in syllabus from each site) of current literature. 15 Teaching An important part of education is the combined education of residents and students at a less advanced stage of training. You will teach residents and students during your rotations as appropriate. You may be assigned specific lecture topics at each site for presentation to medical students and/or residents. We will frequently use you to teach and evaluate in the simulation lab (SimPORTAL). Research An important part of your critical care training is at least an exposure to clinical research. You will attend research meetings at each site, participate in project development, screening, and patient enrollment in clinical protocols, and write up research experiences as assigned. An optional additional experience of from 6 months to one year is available to ICU fellows either before or after their clinical rotations. This experience requires advanced planning. If you are interested, contact the program director for further information. Administrative Each critical care trainee is expected to acquire those skills required to organize, administer, and direct a critical care unit and work effectively as a member of an interdisciplinary team. In order to do this, each trainee will be given graded responsibility, as their level of competence dictates, for making decisions about admissions to the critical care unit, appropriateness of care plan, and discharge from the critical care unit. Each trainee will accompany the critical care staff physician to the monthly critical care committee and quality improvement committee meetings at each site where these issues are reviewed and the process of continuous quality improvement is implemented. Each trainee is expected to understand the quality improvement process and to actively participate in it as their level of competence dictates throughout their clinical training. Attendance at these meetings is very important and will be monitored. D. ACGME Competencies All University of Minnesota Medical School Residency/Fellowship training programs define the specific knowledge, skills, attitudes, and educational experiences required by the RRC to ensure its residents/fellows demonstrate the following: Patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Fellows will gain competence in the performance and application of the following critical care skills: a. Respiratory: airway management, including endoscopy and management of respiratory systems b. Circulatory: invasive and noninvasive monitoring techniques, including trans-esophageal and pericardial cardiac ultrasound and application of transvenous pacemakers; computations of cardiac output and of systemic and pulmonary vascular resistance; monitoring electrocardiograms and management of cardiac assist devices c. Neurological: the performance of complete neurological examinations; the use of intracranial pressure monitoring techniques and of the electroencephalogram to evaluate cerebral function; application of hypothermia in the 16 management of cerebral trauma d. Renal: the evaluation of renal function; peritoneal dialysis and hemofiltration; knowledge of the indications and complications of hemodialysis e. Gastrointestinal: utilization of gastrointestinal intubation and endoscopic techniques in the management of the critically ill patient; application of enteral feedings; management of stomas, fistulas, and percutaneous catheter devices f. Hematologic: application of autotransfusion; assessment of coagulation status; appropriate use of component therapy g. Infectious disease: classification of infections and application of isolation techniques, pharmacokinetics, drug interactions, and management of antibiotic therapy during organ failure; nosocomial infections; indications for applications of hyperbaric oxygen therapy i. Nutritional: application of parenteral and enteral nutrition; monitoring and assessing metabolism and nutrition ii. Monitoring/bioengineering: use and calibration of transducers, amplifiers, and recorders iii. Miscellaneous: use of special beds for specific injuries; employment of pneumatic antishock garments, traction, and fixation devices Medical knowledge of established and evolving biomedical, clinical, epidemiological and socialbehavioral sciences and the application of this knowledge to patient care. Fellows to acquire advanced knowledge of the following aspects of critical care, particularly as they relate to the management of patients with homodynamic instability, multiple system organ failure, and complex coexisting medical problems: a. Cardiorespiratory resuscitation b. Physiology, pathophysiology, diagnosis, and therapy of disorders of the cardiovascular, respiratory, gastrointestinal, genitourinary, neurological, endocrine, musculoskeletal, and immune systems, as well as of infectious diseases c. Metabolic, nutritional, and endocrine effects of critical illness d. Hematologic and coagulation disorders e. Critical obstetric and gynecologic disorders f. Trauma, thermal, electrical, and radiation injuries g. Inhalation and immersion injuries h. Monitoring and medical instrumentation i. Critical pediatric surgical conditions j. Pharmacokinetics and dynamics of drug metabolism and excretion in critical illness k. Ethical and legal aspects of surgical critical care l. Principles and techniques of administration and management m. Biostatistics and experimental design Practice-based learning and improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care based on constant 17 self-evaluation and life-long learning. Fellows are expected to develop skills and habits to be able to meet the following goals: a. Identify strengths, deficiencies, and limits in one’s knowledge and expertise b. Set learning and improvement goals c. Identify and perform appropriate learning activities d. Systematically analyze practice using quality improvement methods and implement changes with the goal of practice improvement e. Incorporate formative evaluation feedback into daily practice f. Locate, appraise, and assimilate evidence from scientific studies related to their patients’ health problems g. Use information technology to optimize learning, and h. Participate in the education of patients, families, students, residents and other health professionals.. Interpersonal and communication skills that result in effective information exchange and teaming with patients, their families, and other health professionals. Fellows are expected to: (1) communicate effectively with patients, families, and the public, as appropriate, across a broad range of socioeconomic and cultural backgrounds; (2) communicate effectively with physicians, other health professionals, and health related agencies; (3) work effectively as a member or leader of a health care team or other professional group; (4) act in a consultative role to other physicians and health professionals; and, (5) maintain comprehensive, timely, and legible medical records, if applicable. Fellows must demonstrate professionalism as manifested through a commitment to carrying out professional responsibilities and an adherence to ethical principles. Fellows are expected to demonstrate: (1) compassion, integrity, and respect for others; (2) responsiveness to patient needs that supersedes self interest; (3) respect for patient privacy and autonomy; (4) accountability to patients, society and the profession; and, (5) sensitivity and responsiveness to a diverse patient population, including but not limited to diversity in gender, age, culture, race, religion, disabilities, and sexual orientation. Systems-based practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system for health care and the ability to effectively call on system resources to provide care that is of optimal value. Fellows must demonstrate the ability to: (1) work effectively in various health care delivery settings and systems relevant to their clinical specialty; (2) coordinate patient care within the health care system relevant to their clinical specialty; (3) incorporate considerations of cost awareness and risk benefit analysis in patient and/or population-based care as appropriate; (4) advocate for quality patient care and optimal patient care systems (5) work in interprofessional teams to enhance patient safety and improve patient care quality; and (6) participate in identifying system errors and implementing potential systems solutions. 18 E. Duty Hours Duty Hours are defined as all clinical and academic activities related to the training program, ie, patient care (both inpatient and outpatient), administrative duties related to patient care, the provision for transfer of patient care, time spent in-house during call activities, and scheduled academic activities such as conferences. Duty hours DO NOT include reading and preparation time spent away from the duty site. Duty hours are limited to 80 hours per week, averaged over a four-week period, inclusive of all inhouse call activities. Residents/Fellows are provided with 1 day in 7 free from all educational and clinical responsibilities, averaged over a 4-week period, inclusive of call. The training program provides adequate time for rest and personal activities, which consists of a 10hour time period provided between all daily duty periods and after in-house call. Surgical Critical Care fellows currently rotate at five sites: the UMMC, Regions Hospital, the V.A. Medical Center, North Memorial Medical Center and Hennepin County Medical Center. There is no in-house call for ICU fellows at any of the sites. There is no cross-coverage of surgery resident and ICU fellow call. Current assignments at each site are as follows: UMMC-F: ICU fellows are on home call 1 to 2 weeks per month as first call. When on call, they round in the ICU daily (including Saturday and Sunday) and receive calls from the in-house resident regarding issues with the ICU patients. On average, fellows return from home to the hospital once weekly. Regions: ICU fellows are on home call every other week as first call in the ICU. When on call, they round in the ICU daily (including Saturday and Sunday) and receive calls from the in-house resident regarding issues with the ICU patients. On average, fellows return from home to the hospital once weekly. There is a trauma attending in house at night to provide backup assistance in the ICU if necessary. MINNEAPOLIS VA HEALTH CARE SYSTEM: ICU fellows are on first call from home during the week as first call in the ICU. They alternate weekends on call with attendings at the VA Hospital. It is infrequent for fellows to have to return to the hospital after regular duty hours. HCMC: ICU fellows are on home call every other week as first call in the ICU. When on call, they round in the ICU daily (including Saturday and Sunday) and receive calls from the in-house resident regarding issues with the ICU patients. On average, fellows return from home to the hospital once weekly. NMMC: .ICU fellows are on home call for operative trauma 3-4 days per week. They round in the TNICU daily and on weekends when on weekend call. Justification for an extension of duty are limited to reasons of required continuity for a severely ill or unstable patient, academic importance of the events transpiring, or humanistic attention to the needs of the patient or family. Under these circumstances the fellow must hand over care of all other patients and document the reasons for remaining to care for the patient in question and submit that documentation in every circumstance to the program director through the RMS system. 19 Duty Hours Tracking 1. All Resident/Fellows* will accurately log their duty hours into the Residency Management System Duty Hours Tracking Module. The website address is https://www.new-innov.com/Login/Login.aspx?Hospital=MMCGME 2. Data must be entered and updated weekly. Time reports to date show that ICU fellows are well within the ACGME requirements (Weekly hours range from 50 on elective rotations to 55-65 on the above rotations). At least one day in seven is free of patient care responsibilities. To use Residency Management Suite: You will need to use an IBM compatible computer. 1. To access RMS, open your Internet browser to access RMS. Website: www.new-innov.com/login.htm Institution’s login: mmcgme Username: user specific 2. Password: user specific **If you do not remember your username and/or password, contact the Surgical Education Office, Michelle Lunden directly at 612-626-2590 or the Surgical Administrative Center RMS coordinator at 612-626-4959. 3. It is highly recommended to bookmark this page. By doing that, you will not have to enter mmcgme every time. 4. Once in the system, you will see a menu on the top of the screen for your options. Under Main choose Duty Hours. Once to the Duty Hours main page there will be a bold header saying Logging Hours. Click on the My Duty Hour link under that. On this screen you will see 4 Data Entry Views to choose from. PLEASE NOTE: You can choose whatever method you want; however, it has been found that the Graphical entry screen is the best for your specific specialty. Because of this, only directions on Graphical and Vacation/Leave are outlined below. Graphical The screen that RMS defaults to is the graphical data entry screen. Pick the day to log hours off the calendar then click the continue button. From this screen you will see the full week around the day you picked. Choose the appropriate Assignment Definition from the drop down box and fill in duty hours by color coding the daily hours. You can fill in multiple days and multiple assignments all on one screen. Click on save when done. You can also edit in bulk here if changes need to be made to past assignments. This will be used most often to log hours after they have happened. Vacation/Leave This screen allows you to pick the correct Time Away designation to track vacation and leave. Make sure you have the correct Assignment Definition chosen and then simply click on the first day of vacation in the first calendar and the last day of vacation in the second calendar. Usually vacation time will be marked as: Time Away-Does NOT Extend TrainingShort. This Assignment Definition should be chosen if you will be gone for 14 days or less. 20 Once hours have been logged on the system, it is important to make sure there are no conflicts and that all hours are approved. To do this scroll over My Duty Hours and click on Approve My Hours. You can also click on the blue Approve Existing Hours link on the main Duty Hour page. After picking the appropriate date range the only hour that will show up are hours either not approved or in conflict (these will be marked with an asterisk). To clear up conflicts either edit the entries or mark the incorrect one with Did Not Work. Make sure to approve all hours worked with Approve Selected Entries. Make sure to logout of the system until you are ready to log more hours. F. On Call Schedules Call schedules for all sites are distributed on the first day of rotation at each site. In-house call is defined as those duty hours beyond the normal work day when residents/fellows are required to be immediately available in the assigned institution. In-house call must occur no more frequently than every third night averaged over a four hour period. Continuous on-site duty, including in-house call, must not exceed 24 consecutive hours. Residents/fellows may remain on duty for up to 6 additional hours to participate in didactic activities, transfer care of patients, and maintain continuity of medical and surgical care. G. Supervision, Faculty and Organization of the Staff 1. The training program is directed by Dr. Jeffrey Chipman who is certified in Surgical Critical Care by the American Board of Surgery. 2. The faculty at UMMC-F, the primary training site, consists of 8 individuals. Each devotes at least 20 hours/week to teaching, research, administration, and the critical evaluation of the performance and progress of our critical care trainees. The faculty to trainee ratio is always greater than 2 to 1. At all times there are two or more faculty based at the University of Minnesota who provide didactic support to the training program. Faculty in anesthesiology, pulmonary medicine, medicine, neurology, and pharmacy also participate in our educational program. 3. Critical care teaching staff have privileges to admit, treat, and discharge patients from the Critical Care units. 4. A collegial relationship exists between the director of the critical care training program and teaching staff in general surgery, transplantation, neurosurgery, cardiothoracic surgery, urology, orthopedic surgery, pulmonary/critical care medicine, pediatric critical care, and obstetrics and gynecology to enhance the educational opportunity for all trainees. 21 Lines of Responsibility University of Minnesota Medical Center - Fairview ICU Site Director Jeffrey Chipman, M.D. ICU Attending On Call ICU Resident Surgical Issues Surgery Chief Res., Attending Surgery/Anesthesia Resident/Intern or Cross Cover Patient Regions Hospital ICU Site Director Bruce Bennett, M.D. ICU Attending On Call ICU Resident Surgical Issues Surgery/Anesthesia Resident/Intern or Cross Cover Patient 22 Surgery Chief Resident Attending V.A. Medical Center ICU Site Director Roderick Barke, M.D., Ph.D. ICU Attending On Call ICU Resident Surgical Issues Surgery Chief Resident/Staff Surgery Resident/Intern or Cross Cover Patient Hennepin County Medical Center ICU Site Director Robert Quickel, M.D. ICU Attending On Call ICU Resident Surgical Issues Surgery Resident/Intern or Cross Cover Patient Specific duties of the ICU resident are outlined in each site rotation description. - 23 Surgery Chief Resident, Attending North Memorial Medical Center TNICU Site Director Alan Beal, M.D. ICU Attending On Call ICU Resident Surgical Issues Trauma Attending Patient Specific duties of the ICU resident are outlined in each site rotation description. G. Graded Responsibility 1. Fellows are encouraged to assume increasing levels of responsibility commensurate with their progress in experience, skill, knowledge and judgment. Upon successful completion of the fellowship program, residents have the skills necessary to assume a lead role in a Surgical Critical Care unit. H. Facilities and Resources 1. Modern facilities are available at each of the primary training sites to support the Surgical Critical Care training program. These include the University of Minnesota Medical Center - Fairview, the VA Medical Center, Regions Hospital, North Memorial Medical Center and Hennepin County Medical Center. 2. Critical care units at each training site are located in designated areas within the hospital and are designed specifically for the care of critically ill patients. Each hospital has the equivalent of a medical intensive care unit, a surgical intensive care unit and a coronary care unit. These facilities are judged adequate by the appropriate hospital accreditation organizations to care for patients with acute myocardial infarction, severe trauma, shock, open heart surgery, major thoracic or abdominal surgery, and severe neurological and neurosurgical conditions. 3. In each unit where a critical care trainee is assigned, the average daily census is greater than six patients per trainee. Each unit consists of specially trained nurses and technicians who are skilled in critical care instrumentation, respiratory function, and laboratory medicine. At each facility, a supporting laboratory is available to provide complete and prompt laboratory evaluation. Modern imaging services and an active emergency service are available as well as nutritional support services. - 24 UMMC-F On Call Rooms The University of Minnesota Medical Center - Fairview has 18 on-call rooms located on the 4th floor of the Mayo building. All rooms have punch code security access which is changed daily, and a security monitor on duty from 2:00 pm-8:00 am, and contain a desk, TV, radio clock, and air conditioning. On-call Residents, on-call Medical Students, on-call fellows, on-call attending physicians and certain on-call hospital staff are eligible to check-in to a call room. Check-in can only occur during the designated check-in hours of 2:30 pm until 7:00 am. To check-in, go to the check-in desk located in the Resident Lounge (Mayo C-496). The check-in desk is staffed by a security monitor during set hours 7 days/week and will require you to present your hospital ID badge. The security monitor will assign you a room, the access code, and the locker room and lounge access codes. All individuals must be out of their rooms by 8:00 am. Housekeeping will come to begin cleaning by 7:00 am. If you wish to sleep until 8:00 am, make sure your DO NOT DISTURB sign is indicated on your door. No room is checked out to the same service two days in a row. Belongings left in room past noon will be removed and kept in a security locker. Belongings can be picked up anytime after 2:30 pm from the security monitor. Any questions, call 612-273-7497. UMMC-F Resident Lounge The Resident Lounge at University of Minnesota Medical Center - Fairview is located in Room 6501 in Unit J and is available 24 hours per day for residents from all specialties. The room is accessible by punch code access, which is changed weekly, or by open door when security monitor is on duty. TV/VCR, computers, and phones with access to the main hospital are available. There is also a partially stocked kitchen with refrigerator, coffee/tea makers, microwave, and toaster. I. Laboratory/Pathology/Radiology Services Laboratory, pathology, and radiology services are readily available through University of Minnesota Medical Center - Fairview. Below is the contact information and location of each of these medical services: Fairview Diagnostic Laboratories Mayo Medical Building, Room D-293 420 Delaware Street SE, MMC 198 Minneapolis, MN 55455 Tel: 612-273-7838, Fax: 612-273-0183 Pathology Pathology Department (also, Pathology Surgical, May Room 422, MMC 76) Mayo Medical Building, Room C-477 420 Delaware Street SE, MMC 609 Minneapolis, MN 55455 Tel: 612-273-5920 Fax: 612-273-1142 Radiology Radiology Department (also, Reading Rooms, Registration) Harvard at East River Road (UH), Room 2-300 (all divisions: MMC 292) Minneapolis, MN 55455 Tel: 612-273-6004, Fax: 612-273-8954 - 25 Interventional CV Radiology, UH-2-300 Tel: 612-273-5040 Fax: 612-273-7500 Radiology Engineering, UH 2-493 Tel: 612-273-6801 Fax: 612-273-6887 Radiology Film Desk Hospital, UH 2-403 Tel: 612-273-5777 Fax: 612-273-7515 J. Medical Records Patient records can be accessed either via EPIC, PACS and Eclipsis Electronic Medical Records (EMR) systems, or by calling University of Minnesota Medical Center – Fairview’s (UMMC-F) Health Information Management (HIM) offices at 612-626-3535. For official medical record retrieval, patients are to contact the UMMC’s HIM offices at: University of Minnesota Medical Center ATTN: Release of Information 420 Delaware Street SE, MMC 601 Minneapolis, MN 55455 Tel: 612-626-3535 Fax: 612-273-2345 K. Security/Safety The Security Monitor Program (SMP) is a branch of the University of Minnesota Police Department. SMP offers a walking/biking escort service to and from campus locations and nearby adjacent neighborhoods. This service is available completely free to students, staff, faculty, and visitors to the University of Minnesota – Twin Cities campus. To request an escort from a trained student security monitor, please call 624-WALK shortly before your desired departure time and walk safe. University of Minnesota Medical Center – Fairview also employs security officers who are on duty 24 hours a day to respond to emergencies and to escort persons to and from the parking facilities. Call 612-273-4544 if you wish to have an escort, and a security officer will meet you at your location. L. Monitoring of Physician Well Being The Surgical Critical Care Program is committed to monitoring the well being of the fellows in the training program. Daily contact between faculty and fellows provides opportunities to observe fellows on a regular basis. Faculty observe for signs of fatigue, distraction, tardiness, or other signs that could indicate overwork or personal problems. The GME office provides an orientation for all incoming residents and fellows which includes the topic of Physician Well Being. During this orientation, fellows are made aware of the confidential Resident Assistance Program that is available for resident/fellows and their families should they require outside assistance. The University of Minnesota Medical School has contracted with Sand Creek to provide services including mental or emotional conditions inhibiting performance or learning, and drug or alcohol related dysfunction for you or anyone in your family. Sand Creek’s counselors have particular expertise - 26 in dealing with the needs of individuals in their residency training programs. In contacting them, you will receive confidential help in determining the problem, what should be done, and how to go about it. Your privacy is a primary concern. That is why an outside firm provides your RAP services. Your counselor will keep everything strictly confidential. Nothing is disclosed to your faculty or to others without your written consent. The RAP services cost you nothing for the initial assessment. Depending on your needs, you may be referred to outside sources of help. If so, you will receive assistance in finding an appropriate, affordable resource. Your health insurance does provide portions of coverage for personal counseling, psychiatric care, chemical dependency and drug treatment. Whether you have an emergency on your hands or you simply need someone to help you sort things out, there is help. A counselor will quickly respond to your call. When the Sand Creek’s office is closed, an answering service will take your call and relay your message. In an emergency, a counselor will contact you immediately. You may discuss your concerns with a counselor at the Sand Creek Office or a counselor will meet you at your hospital. The RAP is designed to be flexible and to accommodate your busy schedule. Sand Creek 333 North Main Street, Suite 203 Stillwater, MN 55082 Tel: 651-430-3383 or 1-800-632-7643 http://www.med.umn.edu/gme/residents/rap M. Communication Policy 1. All general announcements and information will be disseminated via e-mail. 2. Residents/Fellows are required to maintain an active e-mail address and access it at least twice weekly. 3. Resident/Fellows may use a personal e-mail address in lieu of their University X.500 address but must forward their University address to their personal address. Notifications from systems such as RMS must use the U of M address. N. Grand Rounds Compliance Attendance at Grand Rounds is mandatory for Surgical Critical Care Fellows while rotating at the University of Minnesota Medical Center unless involved in emergent patient care or on vacation. O. Dress Code Policy All Department of Surgery Residents and Fellows will comply with the University of Minnesota, Medical School, Graduate Medical Education Committee Dress Code Policy listed below. In addition, all Department of Surgery Residents and Fellows will dress appropriately such that while attending conferences and when participating in all training activities shirts/ties and business attire are worn. Post call residents must be neatly groomed and clean. - 27 University of Minnesota Medical School, Graduate Medical Education Committee Dress Code Policy Resident/fellows are expected to be neat, clean, and orderly at all times during the performance of training program activities. Jewelry, clothes, hairstyle, and fragrances should be appropriate of duties in the hospital or clinic. The resident/fellow’s identification badge is to be worn whenever the resident/fellow is involved in clinical and administrative duties. Residents/fellows are expected to dress accordingly to generally accepted professional standards appropriate for their training program. Each training program may set more specific guidelines for dress code standards in its program. Where safety is a factor, resident/fellows should use common sense in choosing clothing and shoes for training activities. Scrub suits are appropriate for designated area, e.g. Operating Room, Labor & Delivery. In all other areas, a white coat must be worn over the scrub suit. P. Moonlighting The ACGME and the University of Minnesota allows an experience in moonlighting for SICU fellows in our program in approved circumstances. 1) The moonlighting workload should not interfere with your duties and learning experience as a Surgical ICU fellow and you should be appropriately credentialed at the institution where you are moonlighting. Moonlighting must take place outside of your regular duty hours and you must ensure adequate transition of patient care to a responsible attending physician after your moonlighting “shift”. While we have no established maximum number of hours worked per week, we ask you to use common sense in your moonlighting experience, as your education will suffer if you are fatigued during your fellowship hours. If you elect to moonlight, you must request and receive approval in writing from the Program Director. The request must include the location of the moonlighting activity and the expected number of hours per month. Hours spent moonlighting must be included in duty hours logged. Q. American Board of Surgery – Requirements for Certification in Surgical Critical Care Certification of Added Qualifications in Surgical Critical Care by the American Board of Surgery attests that one has acquired a detailed knowledge of the discipline and has developed technical and other skills to the degree that the individual may be judged to deserve recognition as a Specialist in Surgical Critical Care with the ability to provide that care to patients. Fellows who have not yet completed their residency may take the exam after successfully completing the fellowship, but will not receive a certificate until completion of their residency. General Requirements for Certification of Added Qualifications: -Be a Diplomate of the American Board of Surgery. -Have a currently registered full and unrestricted license to practice medicine in the United States or Canada. -Must have successfully completed a Surgical Critical Care fellowship accredited by the ACGME. - 28 -Successfully complete an examination process in Surgical Critical Care administered by the American Board of Surgery. R. Evaluations: The Surgical Critical Care Fellowship Program utilizes a 360˚ evaluation system for the fellows. Fellows evaluate their own progress after each core rotation, and are evaluated by faculty, residents and nursing staff from their rotation site. These evaluations are reviewed by the fellowship director or designee and discussed with each fellow during their midyear and end of year evaluation meetings.. Upon completion of the fellowship year, evaluations from the entire year as well as rotation and program evaluations are reviewed with each fellow during their exit interview. We are currently using a combination of hard copy evaluations(nursing staff & self evaluation) as well as online evaluations through the New Innovations RMS website. The program, rotation, and faculty are in turn evaluated by the fellows. The program evaluation occurs at the completion of the fellowship year, while the rotation and faculty evaluations are performed at the end of each rotation. Our program uses Residency Management Suite (RMS) to complete evaluations. The Education Office will train you on the system and provide you with your login and password. For any questions related to this system, contact either Education Office (626-4959) or Debbie (625-2684). S. Patient Log Fellows are required to keep a log of patients they see at each of the sites. The ACGME requires fellows to maintain a list of all patients. In addition, patients that meet specific criteria (see following page) should be indicated in the log as “Include in SCCIC log”. At the end of the fellowship year a report can be generated of all patients and also the subset for the SCCIC log. This must be turned in to the administrative office as a requirement for completion of the Surgical Critical Care fellowship. Keep a copy of all your patient lists for completing the application form for ABS certification in Surgical Critical Care. Log-ins and passwords will be giving to you during the SICU orientation. The ACGME website is www.acgme.org. Click on Data Collection on the left side and you will get to the log-in screen. - 29 SURGICAL CRITICAL CARE LOG Please insert the operative log for each SCC resident. Essentials in Critical Care Management Select the patients who best represent all the essential aspects of intensive care unit management. Each resident is to develop a Surgical Critical Care Index Case (SCCIC) log of twenty patients who best represent the full breadth of critical care management. At least two out of the seven categories listed below should be applicable to each chosen patient. The completed SCCIC log should include experience, with at least one patient, in each of the following essential categories: ventilator dependent, hemorrhage, hemodynamic lability, multiple organ failure, dysrhythmia, and nutritional support. 1. 2. 3. 4. 5. Diagnosis: Pick list by ICD 9/10 Code Ventilator: yes/no Hemorrhage: yes/no Hemodynamic lability requiring vasoactive/inotropic agents: yes/no Organ failure a. Renal: yes/no b. Hepatic: yes/no c. Endocrine: yes/no d. CNS: yes/no 6. Dysrhythmia: yes/no 7. Invasive monitors a. Pulmonary Artery Catheter: yes/no b. Central Venous Line: yes/no c. Arterial line: yes/no d. Intracranial Pressure monitor/continuous EEG/Lycox/Jugular Bulb oximetry: yes/no 8. Nutritional support a. Enteral: yes/no b. Parenteral: yes/no 9. Procedures (ICU-specific) a. Airways management: i. Endotracheal intubation: yes/no ii. Tracheostomy: yes/no 1) Percutaneous 2) Open b. Placement of vascular lines: i. Central Venous Line: yes/no ii. Pulmonary Artery Catheter: yes/no iii. Peripheral Artery Catheter: yes/no c. Tube thoracostomy: yes/no d. Bronchoscopy: yes/no e. Enteral access: i. Transnasal gastric feeding tube: yes/no ii. Transnasal small bowel feeding tube: yes/no iii. Endoscopically assisted small bowel feeding tube access: yes/no iv. Percutaneous endoscopic gastrostomy/jejunostomy: yes/no 10. Operations: list by CPT code all operations performed by the Critical Care Resident - 30 T. Rotation Schedules Rotation schedules are distributed during orientation. Elective Rotations Elective rotations from 1-2 months are available in several different areas of specialized training. Possibilities include pulmonary critical care, pediatrics, NICU, burn, trauma, echocardiography, anesthesia, interventional radiology, research, or other approved self designed elective. Electives must be selected at the beginning of July in order to ensure placement. Fellows should discuss their options for electives with the program director early in July if they have any questions. SECTION 6 - ADMINSTRATION (Please refer to Institution Policy Manual at http://www.med.umn.edu/gme/residents/instpolicyman/home.html for Medical School Policies on the following: GME Administration Contact List, GME Administration by Job Duty; GME Organization Chart) Surgical Critical Care Sites and Contact List **From University Phones, Dial “8” for an outside line; From Hospital Phones, Dial a “9”** University of Minnesota Medical Center - Fairview: PWB Bldg. Room 11-115 Delaware St. SE, Minneapolis, MN 55455 Office Phone: 612-625-7911 Office Fax: 612-626-0439 Director Faculty Jeffrey G. Chipman, M.D. Assoc. Prof. of Surgery, 11-114 PWB Bldg. 612-626-5622 612-899-8771 Pager Greg J. Beilman, M.D.,. Prof. of Surgery 612-625-7911 612-899-7108 (Pager) Martin Birch, M.D., Asst. Prof. of Anesthesiology 612-624-9990 612-899-6019 Matthew Byrnes, M.D., Asst. Professor of Surgery 612-626-6840 612-899-7023 James Harmon, M.D., Asst. Professor of Surgery 612-899-8116 Mollie James, D.O., Asst. Professor of Surgery 612-899-2905 Kaysie Banton, M.D., Asst. Professor of Surgery 612-899-7169 Melissa Brunsvold, M.D., Asst. Professor of Surgery 612-899- Fellowship Coord. Debbie Bresina 612-625-2684 11-115b PWB Bldg. Salary/Benefit Info Teri Wolner 612-625-3926 11-145 PWB 4D SICU UMMC operator 612-273-3044 612-273-3000 - 31 AHC Help Desk (Computer 612-626-5100 Problems) EPIC Helpline 612-672-6805 University Information 612-625-5000 Video & photography Regions Hospital: Department of Surgery 640 Jackson St. Minneapolis, MN 55101 Office Phone: 651-254-1633 Office Fax: 651-254-1480 Director of SICU Faculty GME Jerry Vincent 612-625-9463 Bruce A. Bennett, M.D. (on military leave) North Bldg., 3rd flr, Ste. 2 651-254-1633 David J. Dries, M.D. Michael McGonigal, M.D. Gary Collins, M.D. (Interim Director) Cassandra Palmer, M.D. Deb Collier, Program Associate Graduate Medical Education MS 11501G Institute for Medical Education * Regions Hospital 640 Jackson Street St. Paul, MN 55101 651-254-1504 (office) 651-254-5044 (fax) Deb.K.Collier@HealthPartners.Com V.A. Medical Center: Department of Surgery (112) 2J100, 1 Veterans Drive Minneapolis, MN 55417 Office Phone: 612-725-2065 Office Fax: 612-725-2227 Director SICU Rod Barke, M.D., Ph.D. Rm. 2J100 612-725-2065 612-660-7166 pager SICU Faculty Jerome H. Abrams, M.D. Paul Druck, M.D. Residency Coordinator Linda Dent 612-467-3353 Orientation Lisa Loyas Lisa.Loyas@va.gov HCMC: Department of Surgery 701 Park Avenue Minneapolis, MN 55 415 Director SICU Faculty Robert Quickel, M.D. 612-873-2810 612-527-3000 pager Art Ney, M.D. Chad Richardson, M.D. Joan VanCamp, M.D. - 32 612-467-1330 Residency Coordinator Phyllis Squiers 612-873-2849 NMMC Trauma Institute North Memorial Medical Center 3300 Oakdale Ave. N. Robbinsdale, MN Director TNICU Alan Beal, M.D. 763-520-7647 612-589-7179 pager Faculty Mark Ahrendt, M.D. Kevin Croston, M.D. Eric Irwin, M.D. John Cummings, M.D. Matthew Byrnes, M.D. Medical Staff Office Deb Bement deb.bement@northmemorial.com 763-520-5848 763-520-5554 fax Tracey Worley tracey.worley@northmemorial.com 763-520-1705 Susan Adler susan.adler@northmemorial.com 763-520-1754 - 33 Department of Surgery Administrative Contact List Selwyn Vickers, M.D. Professor and Chair Program Director Director of Graduate Studies 612-626-1999 Michael A. Maddaus, M.D. Associate Program Director Chairman, Surgical Education Council 612-624-9461 Daniel A. Saltzman, M.D., Ph.D. PGY-1 Director Assistant Professor 612-626-4214 Jeffrey Chipman, M.D. Associate Residency Program Director PGY-2 Mentor Assistant Professor 612-625-7911 Greg Beilman, M.D. PGY-3 Mentor Associate Professor 612-625-7911 Todd M. Tuttle, M.D. PGY-4 Mentor Associate Professor 612-625-2991 Assistant: Cynthia Messer Assistant: Sara Kloepper Assistant: Cheryl Fish Assistant: Colleen Powers Assistant: Christine Vincent Assistant: Tina Russell - 34