lanarkshire psychiatric emergency plan
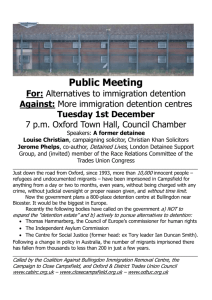
advertisement

LANARKSHIRE PSYCHIATRIC EMERGENCY PLAN Agreed document 30th September 2005 (Not yet ratified) CONTENTS SECTION PAGE NUMBER FOREWORD 3 1. BACKGROUND 4 2. PRINCIPLES 5 3. SCOPE OF PSYCHIATRIC EMERGENCY PLAN 6 4. DUTY TO INQUIRE AND WARRANTS 7 5. PLACE OF SAFETY 10 6. EMERGENCIES IN THE COMMUNITY 10 7. RISK MANAGEMENT 15 8. USE OF DETENTION (EMERGENCY AND SHORT TERM) IN THE COMMUNITY 16 9. TRANSPORT OF DETAINED PERSON TO HOSPITAL 19 10. MEDICAL TREATMENT IN EMERGENCY 21 11. ADMISSION TO HOSPITAL 22 12. USE OF DETENTION (EMERGENCY AND SHORT TERM) IN THE HOSPITAL 23 APPENDIX 1 - AVAILABILITY OF APPROVED MEDICAL PRACTITIONERS 28 APPENDIX 2 – HOW TO CONTACT AN MHO 29 APPENDIX 3 - TRANSLATION AND COMMUNICATION PROCEDURES 32 2 FOREWORD The implementation of the Mental Health (Care and Treatment) (Scotland) Act 2003 is a significant event for all those affected by mental health problems, whether service users, carers or those that work in caring services. The Act both reflects and encourages a shift in emphasis to services that are more tailored to the individual and focused on helping people with mental problems maintain or return to their normal levels of functioning in as many aspects of their lives as possible. The Lanarkshire Psychiatric Emergency Plan (PEP) has been brought together through the work of many different groups. There has been consultation about the content and form the document should take, but also an understanding that the procedures outlined, and therefore the document will have to adapt and change as circumstances alter and lessons are learned as the new act is implemented in practice. It is important to emphasise that the PEP describes procedures that will be followed in the exceptional case rather than the rule. In most situations, people with mental health problems or in crisis will seek help themselves and the issue of detention under the Act will not arise. As services for those in crisis become more comprehensive and diverse the options for offering a response other than hospital admission will improve. For those that do require admission this document should help to ensure that a difficult process is made as smooth as possible. This PEP is the first time that we are aware of, that a multi-agency document outlining the procedures to be followed in event of psychiatric emergency has been produced in Lanarkshire. Most of the procedures reflect current practice and are adapted to meet the requirements of the new Act, but some have been altered to reflect consensus on good practice. It should provide a useful guide to those involved in helping to manage what can be very difficult situations. The PEP has been produced to try and help different agencies work together to ensure that the principles and spirit of the Act can be maintained even in difficult circumstances. I trust that those involved in its production will find this document useful. Commonly used abbreviations in document. PEP MHO AMP CPN PAT SAS JLIP GP A&E The Act - Psychiatric Emergency Plan Mental Health Officer (Social Worker) Approved Medical Practitioner (Psychiatrist) Community Psychiatric Nurse Psychiatric Assessment Team (Nursing team) Scottish Ambulance Service Joint Local Implementation Plan (for mental health act) General Practitioner (family doctor) Accident and Emergency The Mental Health (Care and Treatment) (Scotland) Act 2003 3 1. BACKGROUND 1.1. The main provisions of the Mental Health (Care and Treatment) (Scotland) Act 2003 commence on 5 October 2005. As part of the implementation process in Lanarkshire a Psychiatric Emergency Plan has been agreed by the partner agencies involved in the Joint Local Implementation Plan (JLIP). 1.2. The concept of a Psychiatric Emergency Plan (PEP) was first introduced in the recommendations of the Bid 79 report drawn up by RARARI in 2003. The report dealt with the management of psychiatric emergencies in remote and rural communities and it recommended that: 1.3. “Boards should be responsible for ensuring that a Psychiatric Emergency Plan (PEP), endorsed by all appropriate agencies and professional groups, is in place for each locality. It should include statements on: the skills and competencies required of staff; minimum staffing levels, and clear arrangements on the availability of Mental Health Officers (MHOs).” 1.4. The draft Code of Practice to the mental health act, published in 2004 also stated that 1.5. “As a means of addressing all these issues comprehensively and in a manner which best reflects local circumstances, it would be good practice for the relevant local agencies and service providers who might potentially be involved in psychiatric emergencies to work together to develop and agree on a “Psychiatric Emergency Plan” (PEP). This would allow potential local difficulties to be addressed and contingency procedures put in place before they arise for real. The aim of a PEP would be to agree on procedures which would manage the transfer and detention process in a manner which minimises distress and disturbance for the patient and to ensure as smooth and safe a transition as possible from the site of the emergency to the appropriate treatment setting. The professionals involved in the drawing up of a PEP could include general practitioners, approved medical practitioners, MHOs, other social workers, social care workers, CPNs, ward nursing staff, independent service providers, police officers, and ambulance personnel. It will also be important to seek input into the preparation of a PEP from mental health service users and carers. It would be good practice to use a PEP as a basis for joint training of all those professionals named in the plan as having specific responsibilities in the transfer and detention process. Similarly, it would be good practice to ensure that the PEP is updated regularly, particularly in light of any significant incidents or specific difficulties which may have arisen since the PEP was last updated”. 4 2. PRINCIPLES 2.1. The implementation of the Mental Health (Care and Treatment) (Scotland) Act 2003 is a major advance in the legislation governing care of those with mental health problems in Scotland. The legislation is framed around a set of principles that should be applied across all aspects of this Psychiatric Emergency Plan. The principles are as follows: Non-Discrimination People with mental disorder should, wherever possible, retain the same rights and entitlements as those with other health needs. Equality All powers under the act should be exercised without any direct or indirect discrimination on the grounds of physical, disability age, gender, sexual orientation, language, religion or national, ethnic or social origin. Respect for Diversity Service users should receive care, treatment and support in manner that accords respect for their individual qualities, abilities and diverse background and properly takes into account their age, gender, sexual orientation, ethnic group social cultural and religious background. Reciprocity Where society imposes an obligation on an individual to comply with a programme of treatment of care, it should impose a parallel obligation on the health and social care authorities to provide safe and appropriate services, including ongoing care following discharge from compulsion. Informal Care Wherever possible, care, treatment and support should be provided to people with mental disorder without the use of compulsory powers. Participation Service users should be fully involved so far as they are able to be in all aspects of their assessment, care, treatment and support. Their past and present wishes should be taken into account. They should be provided with all information and support necessary to enable them to participate fully. Information should be provided in a way which makes it most likely to be understood. Respect for Carers Those who provide care to service users on an informal basis should receive respect for their role and experience, receive appropriate information and advice and have their views and needs taken into account. Least Restrictive Alternative Service users should be provided with any necessary care, treatment and support, both in the least invasive manner and the least restrictive manner and environmentally compatible with the delivery of safe and effective care, taking account, where appropriate, the safety of others. 5 Benefit Any intervention under the act should be likely to produce for the service use a benefit that cannot reasonably be achieved other than by intervention. Child Welfare The welfare of a child with mental disorder should be paramount in any interventions imposed on the child under the act. 2.2. The act also introduces provisions that allow people to nominate a “Named Person” that will act in their interests and to produce an “Advanced Statement” describing their wishes in the event that they require treatment. More details of these provisions are available elsewhere. 3. SCOPE OF PSYCHIATRIC EMERGENCY PLAN 3.1. The Lanarkshire PEP is a guide for all who are likely to be involved in the management of a crisis situation involving somebody who has, or is thought to have a mental disorder that may require intervention using the Mental Health Act. 3.2. It outlines the procedures to be followed to ensure that appropriate assessment of any given situation can be made and then the actions that will follow, if a decision is made that the situation requires the use of the Mental Health Act. 3.3. These are the normal procedures to be followed in the event of situations arising in hospital and in the community. The roles and responsibilities of the different agencies involved in such situations are described. They do not deal with every eventuality and there will be times when good sense dictates that the principles of the Act will be met by following a different course of action. 3.4. Procedures are intended to minimise distress and disturbance to those involved in what is frequently a very difficult event in a person’s life. While the plan concentrates on the procedures that will be followed in event of the powers of the Mental Health Act being used, it is important to emphasise that the principle of least restrictive alternative should be maintained. It is also important that any diverse cultural or religious requirements are recognised and met as fully as possible throughout. 3.5. Detailed documents describing the Procedures to be followed by AMPs and MHOs in event of Short Term or Emergency Detention have also been produced and should be referred to in the event of these procedures being required. 3.6. The production of the PEP has been guided by the Draft Code of Practice and may be revised when the final code is produced. The code provides a more detailed description of the various roles and responsibilities and should be consulted where questions arise. 6 4. DUTY TO INQUIRE AND WARRANTS 4.1. Warrants under the Act can only be obtained by a Mental Health Officer, or in the case of a patient who is already subject to powers under the Act, by an authorised person under the Act. Details of the range of powers that may be sought are described below: 4.2. Local Authority Duties 4.2.1. Section 33 of the Act places a duty on the local authority to make inquiries where it appears that a person aged 16 or over in their area has a mental disorder and: The person may be or may have been subject or exposed to illtreatment; neglect; or some other deficiency in care or treatment. or The person’s property may be suffering or have suffered loss or damage; or may be at risk of loss or damage or The person may be living alone or without care and unable to look after themselves or their property or financial affairs. or Because of the mental disorder the safety of some other person may be at risk. 4.2.2. Section 33 inquiries can be carried out by any suitable person appointed by the local authority. Such inquiries may therefore be carried out by a social worker or care manager or other suitable person appointed to do so by the local authority. Section 33 inquiries do not require to be carried out by a Mental Health Officer, although there may be particular circumstances where the local authority chooses this course of action for specific reasons. For example, in circumstances where it can reasonably be anticipated that a further application for a warrant under section 35 of the Act may be required. 4.2.3. Section 34 gives the local authority powers to request the assistance of a range of agencies in carrying out inquiries. These include Health Boards; the Care Commission; the Public Guardian; the Mental Welfare Commission; and a National Health Service Trust. The same section places a duty on those agencies to co-operate with such requests unless doing so would unduly prejudice the functions of that agency. 7 4.3. Mental Health Officer Duties 4.3.1. Section 35 Warrants Section 35 provides powers for a Mental Health Officer to apply to a Sheriff or Justice of the Peace for warrants to support the purposes of Section 33 inquiries, if required. These warrants can only be applied for by a Mental Health Officer. The duration of a warrant is 8 days beginning on the day it was granted. There are 3 different powers that can be requested within a Section 35 warrant. These are: To authorise entry, with the assistance of a police constable. To authorise the detention of the person in situ for up to 3 hours for the purposes of medical examination by a medical practitioner named in the warrant. To authorise a specified medical practitioner to access and inspect medical records. In addition to authorising the MHO and police constable, the warrant can authorise specified persons and this may include a medical practitioner or health staff member. If the outcome of the assessment of the medical practitioner in consultation with the MHO, is that the person requires immediate admission to hospital and this cannot be achieved with the persons consent then admission to hospital may be arranged either by a short term or emergency detention certificate, where the grounds are met. (See joint procedures for further guidance). If grounds for detention in hospital are not met but it is assessed that the person has a mental disorder and requires to be removed to a place of safety then consideration should be given to the MHO making an application for a Removal Order, as described below. 4.3.2. Removal Orders to a Place of Safety Section 293 allows a Mental Health Officer to apply to a Sheriff for a Removal Order. A Removal Order authorises a police constable to enter premises and it authorises the removal of a person aged 16 or above to a place of safety for a period not exceeding 7 days. Although the draft code of practice suggests that a Removal Order may be appropriate in situations of high risk, account needs to be taken of the fact that in general the ‘tests’ of proof are more stringent and the Sheriff is generally required to give the parties mentioned in the application the opportunity to be heard before reaching a decision. (The Sheriff may dispense with this requirement if satisfied that it would cause delay that would be likely to prejudice the person who is the subject of the application.). 8 In relation to a Section 293 application, the sheriff must be satisfied that there is mental disorder and that there is neglect or ill treatment etc, while Section 35 simply requires the it appears the person has a mental disorder and that they may be subject to ill treatment or neglect etc. In addition, under Section 295 a person subject to a Removal Order or any person claiming an interest can apply to a Sheriff to have a Removal Order varied or recalled. The MHO must implement the order within 72 hours of it being granted. Section 294 permits application for a Removal Order to be made to a Justice of the Peace, only in circumstances where it is impracticable to make the application to the Sheriff. 4.4. Attendance of Medical Practitioners In general the execution of any of the above warrants should be carried out with a medical practitioner in attendance. The grounds for such powers require a reasonable belief that the person is mentally disordered and may be in need of services, care and treatment or protection. Failure to have a medical practitioner in attendance at the time of entering premises may result in unnecessary delay and distress for the patient. It may also result in persons being placed at risk. 4.5. Authorised Persons Duties 4.5.1. Warrant to Enter Premises for the Purposes of Taking a Patient Section 292 permits any person authorised under the Act to apply for a warrant to enter premises and to take a patient who is already subject to the Act to any place or into custody. This warrant would be appropriate for example for someone who is subject to compulsory powers who has absconded or was refusing access following the granting of an order or certificate. While an application for this warrant may be made by any person authorised under the Act, when granted, it additionally authorises any Mental Health Officer and any police constable for the area to enter the premises along with the original authorised person who made the application for the warrant. 4.6. Police Constable Duties 4.6.1. Removal from a Public Place to a Place of Safety If a police constable reasonably suspects that a person in a public place has a mental disorder, Section 297 provides the power to remove the person to a place of safety for up to 24 hours, if the constable is satisfied this is necessary in the interests of the person or for the protection of others. 9 When action is taken under Section 297 the constable must notify the local authority; the person’s nearest relative, carer or care service and the Mental Welfare Commission of certain matters. These matters include: the person’s name and address date and time of removal to the place of safety circumstances giving rise to the removal the address of the place of safety when the place of safety is a police station why this was the case. 4.7. Making a Referral It is important that when someone has reason to believe that a person appears to have a mental disorder and may be in circumstances that require further inquiry under Section 33, that a referral of those concerns should be made to the local social work office during normal hours or to the out of hours service. See contact details in appendix. 5. PLACE OF SAFETY 5.1. When removing a patient under a Section 292, 293 and 294 the place of safety under the Act means: a hospital ( both acute and psychiatric) premises which are used for the purpose of providing a care home service Other suitable place (other than a police station), the occupier of which is willing temporarily to receive mentally disordered person. 5.2. In Lanarkshire the appropriate Place of Safety will be determined by the individual circumstances of the case. Where the person involved is known to services and possible need for admission has been recorded as part of relapse management section of care plan, then the appropriate Psychiatric Unit should be regarded as the Place of Safety. In most other cases the Place of Safety will be the local Accident and Emergency Department or Out of Hours Treatment Centre. A decision on appropriate place of safety should be taken after discussion with the Psychiatric Assessment Team. If the situation is one of such urgency that there is no time to discuss this with the Assessment Team then the Accident and Emergency Department is appropriate. 5.3. At the present time it is not anticipated that care homes or other suitable places will be used as a formal place of safety as defined under the Act in Lanarkshire. 10 6. EMERGENCIES IN COMMUNITY 6.1. There are a number of ways in which a person who may require emergency intervention from mental health services will come to the attention of services. In most cases the person themselves (or a relative/carer/neighbour) will contact Primary Care Services. In working hours this will be their own local GP practice and out of hours, this will be through NHS24 and the Primary Care out of hours team. The person (or a relative / carer/ neighbour on the person’s behalf) may come to the attention of services in the community including social work, care providers, housing or other support services. The person may present to Accident and Emergency directly. The person (or a relative/carer/neighbour) may call an Ambulance directly The person may be involved in a situation that requires the Police who may identify a potential mental health problem. 6.2. Where a psychiatric emergency is suspected in the community it is essential that all the available information be used to make a risk assessment of the situation in advance. If there is thought to be a risk of violence, the police should be contacted and asked to attend in a discreet manner. If the situation appears to be very urgent from the information available, it may be advisable to arrange an ambulance and nurse escort in advance of assessment. 6.3. Role of Ambulance Service if first to identify potential psychiatric emergency 6.3.1. The public, police, NHS 24, GP or any carers can access the ambulance service in an emergency. How the SAS respond to such requests will depend upon the information available. Response category will be categorised depending upon that information. Calls originating from general public are triaged via Priority Based Dispatch Protocols. Calls originating from medical practitioners and Nursing staff including PAT will be classed as emergency if requested. In such cases the ambulance will go directly to the patient’s locus. If SAS called by NHS 24, SAS will attend, assess the patient, treat as necessary and if safe will take to hospital. 6.3.2. Role of ambulance staff in emergency: Attend and assess In hours - contact GP for advice Out of hours – contact PAT directly for advice Treat as required Transport to hospital 11 6.4. Role of police if first called to emergency situation The police can be involved in crisis situations usually initiated by a 999 call from members of the public, carers and health workers requesting assistance. Upon receiving such a request the police response is as follows: Attend incident Support partner agencies Contact PAT for advice Provide control and restraint if appropriate Assist with transport and escort if required. This may mean that the police will transport the individual to the A&E dept or an agreed hospital in accordance with relapse management plan if it is felt that this is the safest option Remove to police custody if this is thought to be most appropriate response. In attending an incident the role of the police is to: Provide proportional response In partnership with other agencies assess seriousness of situation Take the lead role where there is increased risk of harm to self or others, or there is a hostage situation - actual or potential. In that particular case they will provide a negotiator and the situation will be handled by the Public Order Team. 6.4.1. Role of the police in civil detentions There may be occasions when staff will be unable to manage safely a situation within community premises or person’s home. If there is a clear threat to any person’s personal safety, the assistance of the police should be requested. Where possible the need for police assistance should be carefully considered before proceeding and suitable arrangements agreed with the police prior to commencing the assessment. However, it may not always be practical for staff directly involved in the assessment to anticipate that police assistance may be required, and the decision to involve the police may be taken by any member of the team involved in the detention at any stage. In the case of the police being called to assist in a detention: Once the police arrive at the scene they will discuss situation with staff involved and if necessary will take charge and make decisions about restraint and removal of the person to a place of safety. Frequently, the presence of the Police will be sufficient to ensure that the situation is brought under control without the Police having any direct involvement. It is not part of the role of police to restrain persons in order for them to have medication administered 12 6.4.2. In a situation where an individual is at home and access gained, police attendance will only be necessary if situation is one of potential risk and other partner agencies attending request assistance. 6.4.3. In a situation where access has been denied, entry to premises can only be obtained through the obtaining of a warrant or removal order, by a Sheriff or Justice of the Peace, granted in terms of Sections 292 and 293 of the Act outlined in Section 4. The MHO will liaise with the police in advance of making the application as per joint procedures regarding warrants and duty to inquire. Once they have obtained the relevant warrant, the MHO will liaise with the police in attendance and will report on the known circumstances of the patient at that time. The medical practitioner will advise on any known medical aspects. 6.4.4. In siege circumstances, trained Public Order Officers who have specialist equipment and training will attend and take the lead role. Depending on the circumstances the police will then convey the patient to a place of safety or hand over to the Medical Practitioner. 6.4.5. In situations where an incident occurs in a public place and a police officer reasonably suspects that a person has a mental disorder; is in immediate need of care; and considers that it is in the interests of that person or for the protection of the public, the officer under Section 297 of the Act may remove that person to a place of safety. In such a situation the police officer will contact the PAT in the first instance for information and advice. PAT will obtain any information about person available to them and advise on appropriate place of safety. If no information is available PAT will ask the officer to bring the person to Accident and Emergency for assessment. If the patient is brought to Place of Safety under Section 297 for assessment a medical practitioner must see them. The police must inform the local authority and nearest relative that they have taken this action as soon as reasonably practicable. 6.5. The Psychiatric Assessment Team (PAT) will develop and maintain close links with Police services, particularly those stations where there are custody suites. Custody officers can contact PAT by telephone when they have concerns about mental health of somebody they have detained. PAT team will be able to advise of care plan if one exists or provide advice on how to manage the situation, including bringing the person to hospital for assessment. 6.5.1. The PAT will assess as priority persons brought to A&E by the police. The police will remain with the person in the A&E department until completion of the assessment. a) If assessed as having mental disorder and requiring admission, police presence no longer required. 13 b) c) d) e) If assessed as having mental health problems a suitable assessment of need must be undertaken. Decisions should be made about any required emergency service in collaboration with other health, social work and housing services. Particular consideration must be given to whether the person is a vulnerable adult and should be dealt with in accordance with joint procedures for vulnerable adults and/or whether there are any child welfare or protection matters that require action. If needs do not require urgent action referral to routine services should be made as soon as possible. If no diagnosis of mental disorder and crime has taken place, the person will be discharged from A&E into police custody with the option of follow up and further assessment by the Forensic CPN/Court Liaison Service. The PAT nurse will ensure that information is relayed to that service in time for the next day’s court appearance. If assessment the next day suggests detention under Mental Health Act is required then the duty AMP and MHO should be contacted and will assess at the court. If no diagnosis of mental disorder, no crime committed and assessed as having no community care or other significant needs the person will be discharged from A&E. If necessary the police can assist in the person’s removal from the department. If person is intoxicated with alcohol or drugs it is likely to be difficult to make a reasonable assessment of their mental health. The value of such assessment will vary according to the degree of intoxication. If intoxication is to such a degree that a proper assessment is not possible then an appointment for an assessment the next day should be offered – either at hospital by PAT if likely to be released or by court liaison as in (c) if charged. 6.5.2. In certain circumstances the police may be involved in the transportation of patients to hospital: If the situation becomes unsafe and there is risk of harm to the patient or others If a crime has been committed If there is high level of aggression – verbal or physical – and the situation cannot be contained In such situations this would be considered as the safest and quickest way to get the patient to hospital for further assessment and treatment. 14 6.6. Co-ordination between agencies in advance of assessment In most cases situations will be resolved through intervention of medical practitioner, PAT team and MHO as outlined in sections 8 – 10 of PEP. On rare occasions where a multi-agency response is thought to be required in advance of the assessment, a lead person will be identified to co-ordinate that response. In situations where there is known or suspected violence or in a hostage situation the police will take the lead role and will involve the medical practitioner and MHO only when safe to do so. In most other cases the PAT will take lead role in co-ordinating Medical practitioner, MHO, ambulance and police response, ensuring principle of least restrictive option is maintained. If the Ambulance Service is called to a situation first, they will take lead role in requesting the presence of other agencies if required. 6.7. Information sharing in emergency situation In an emergency or potential emergency situation it is important that a balance is struck between the management of risk and the duty of confidentiality about individuals personal information. Information should be shared on a need to know basis – the information provided should be basic, but sufficient to describe any problems and identify risk. Information shared should be sufficient to assist agencies to make a decision in an emergency situation and also ensure the safety of the responding services’ personnel. Examples: Primary Carer and/or Named Person Any identified risk factors Recent contact with services Likely indicators of relapse and advice on de-escalation. Hepatitis B/C status if known Systems to improve electronic sharing of information between NHS sites and between agencies are being developed. The use of Care Plan summaries detailing agencies involved in care, named person, relapse management plan, presence of advance statement and any other needs will assist this process. These summaries will be held by service users and by all agencies involved and consent should be sought that these can be shared with other agencies at times of emergency. 7. RISK MANAGEMENT 7.1. The detention of persons in any setting can have a large element of the unknown. It is important to attempt to access records or gain as much background information as possible to assess risk. Areas of potential risk of the person to themselves or others can be influenced by a number of factors and all transfers should have any potential risk identified. 15 7.2. The following points should always be considered in identifying potential risk, but this list is not exclusive: Do the person and/or his/her family have a history of violence? Does the person have a history of dangerous impulsive acts? Does the person have a history of carrying weapons? Does the person appear to be under the influence of drink or drugs? Is the person expressing intent to harm you or others? Are there signs of anger or frustration? Is the person displaying sexually inappropriate behaviour? Are there other environmental risk factors such as aggressive pets? Good practice dictates that, in all cases, staff should refer to their own agency's policies and guidelines on, e.g. lone workers and personal safety and should have completed appropriate training. The following are examples that should be considered if the interview is being conducted in a community-based establishment: Conduct the interview in an area that is easily accessible to other staff in the event of an emergency; Try to use an interview room that has been fitted with an alarm system and use it to notify other staff should a threatening situation arise; Remove obvious hazards from the area being used to conduct the interview; Balance issues of privacy with environmental, safety and observational considerations; Always communicate an intention to detain a person to other staff within the establishment; Consider having another member of staff present during the interview; and The movement of the detained person around the interview room should be unrestricted as far as is reasonably practicable, bearing in mind the potential risk the person may pose to him or herself or others. If the interview is being conducted in a private dwelling setting: Respect disagreements with the person over detention decisions and allow for non-confrontational explanations; Staff should carry a mobile phone in the community; and Staff should ensure that they have received the appropriate management of aggression training. It is incumbent upon all statutory services to act in the best interests of persons to deliver high quality care and to treat persons with respect and dignity at all times. All procedures should be directed towards the best overall interests of the person, being based on the principle of minimum necessary force or action to achieve a desired outcome, and to be carried out in a safe, professional and competent manner. The underlying principles of the Act relating to the care of the person should be observed at all times. A pragmatic approach should also be taken to ensure the smooth running of any function discharged under the Act with good communication being fundamental. 16 8. USE OF DETENTION (EMERGENCY AND SHORT TERM) IN THE COMMUNITY 8.1. This section summarises actions to be taken in event that detention in community is considered the likely outcome of assessment. More detail is contained in the Joint Lanarkshire “Procedures for Emergency Detention” and “Procedures for Short Term Detention” and also in the Code of Practice. 8.2. Assessment and decision to use emergency or short term detention. 8.2.1. Where a potential concern has been identified in the community the first point of contact will normally be the persons Primary Care practice. In working hours a GP should make arrangements to assess the person, visiting if the person cannot or will not attend the practice. If it is clear from the nature of the information given to GP that there is a likelihood of assessment for detention they should contact the duty MHO immediately, in advance of visit. A joint visit may be made if appropriate or MHO may decide to await GP’s assessment before agreeing to visit. 8.2.2. If a situation arises out-of hours then contact will be through NHS 24 to the Lanarkshire Out-Of Hours service. The Psychiatric Assessment Team attached to the service should be involved in discussion of the situation at an early stage. If detention appears to be a possibility the duty MHO must be consulted. A joint visit involving doctor, PAT nurse and MHO may be agreed in these circumstances. 8.2.3. If a situation in community involves somebody well known to psychiatric services within normal working hours, then contact may be made directly with local mental health team who will advise appropriately. In some cases a decision may be made to request an assessment by AMP directly, particularly if duty AMP or another available AMP already knows person. Again, early contact with the duty MHO is essential. 8.3. A short-term detention certificate is the preferred “gateway order” because, as compared with an emergency detention certificate, it can only be granted by a specialist in psychiatry; the consent of an MHO is mandatory; and it confers on the patient and the patient’s named person a more extensive set of rights, including the right to make an application to the Tribunal to revoke the certificate. 17 8.3.1. During working hours (Monday to Friday 9am till 5pm) each locality will have a duty Approved Medical Practitioner who will be available to provide advice and where circumstances allow will make arrangements to examine the person after a GP assessment. (See Appendix 1 for details). The duty AMP will not have other fixed commitments and will be able to prioritise requests for assessment in the community. On most occasions the arrangements will be made to assess immediately after the GP together with MHO who may already be present. If AMP is dealing with other priority cases they will agree an appropriate time for assessment after discussion with the GP and MHO but will assess during that working day. 8.4. Use of short term detention in the community The criteria for granting a short term detention certificate are described in Section 44 of the Act. The AMP must consider it likely that the following criteria are met: The patient has a mental disorder The patient’s ability to make decisions about medical treatment is significantly impaired as a result of mental disorder. It is necessary to detain the patient in a hospital to determine what medical treatment should be given or to give the patient treatment. There would be significant risk to the health, safety or welfare of the patient or safety of any other person, if the patient were not detained Granting a short term detention certificate is necessary The onus is on the AMP to demonstrate that they consider it likely that the above criteria are met. The AMP must consult with and obtain the consent of the MHO before a short term certificate can be granted. The AMP must be satisfied that there is no conflict of interest in relation to the medical examination of the person. 8.4.1. An AMP cannot issue a short term detention certificate without the consent of an MHO. Where it is impractical to arrange a joint interview it should be borne in mind that consent and subsequent detention may occur within three days of the initial examination by AMP. 8.4.2. Procedures to be followed in event of refusal of consent by MHO are detailed in the Procedures for Short Term Detention. 8.5. Use of Emergency detention in the community The criteria for granting an emergency detention certificate are described in Section 36 of the Act. 18 The criteria are that it is likely that: The patient has a mental disorder The patient’s decision-making ability with regard to medical treatment is significantly impaired, as a result of the mental disorder. and the medical practitioner is satisfied that, It is necessary as a matter of urgency to determine what medical treatment should be provided There would be significant risk to the persons health, safety, or welfare, or safety of others Short term detention would involve undesirable delay. The doctor must consult a MHO, unless it is impracticable to do so, and must receive the consent of the MHO. There must be no conflict of interest in relation to the medical examination. 8.5.1. If the medical examination suggests the criteria of presence of mental disorder, significantly impaired judgement by reason of mental disorder, urgency and significant risk are met they should still seek to use a Short Term Detention unless this would involve undesirable delay, and there is urgent clinical necessity. 8.5.2. If this is deemed to be an undesirable delay due to clinical urgency then the GP should consult with the duty MHO about whether the issuing of an Emergency Detention Certificate may be appropriate, using form DET1. Such a consultation will involve the MHO interviewing the person and cannot be a telephone consultation unless the MHO has had very recent contact with the person involved. If the MHO agrees appropriate, they will provide consent. If not, the MHO will provide a written statement detailing the safe and viable alternative arrangements that are being put in place and why these are preferable to detention. 8.5.3. If urgency is so great that there is insufficient time to arrange a consultation with a MHO then the GP can issue emergency detention without consent, but must provide a report to relevant Hospital Managers about why no consent has been obtained. Hospital Managers will pass this report to the Mental Welfare Commission, to the relevant Local Authority, to the patients nearest relative and to the Named Person, where known. 8.5.4. Out of hours, the GP must discuss with the duty MHO and arrange a consultation if at all possible. If this is not possible then 8.5.3 applies. 19 8.5.5. It is also advised that the GP or nurse from the Psychiatric Assessment Team if involved in the assessment should contact the duty consultant for advice, if detention is being considered. If the situation is one of such urgency that this is not possible, then contact should be made after the situation has been resolved. Duty consultant will offer advice and if situation is one where Short Term Detention would be more appropriate, will make arrangements to attend. 8.5.6. If contacted by telephone, the consultant may provide advice but ultimate responsibility for decision to issue Emergency Detention Certificate lies with the attending doctor in consultation with the MHO. If the consultant decides to attend to assess the situation personally and the team agrees it is clinically safe to await their arrival, the consultant will assume responsibility for decision on arrival at scene. 8.5.7. Medical Practitioners are strongly advised to use the form provided (DET1) when using Emergency Detention. A written statement containing all the statutory information would be theoretically valid but may be open to challenge in court. The certificate must be issued on same day as examination, or within four hours if examination after 2000 hours on that day. The certificate must be presented to Hospital Managers before detention becomes valid. 9. TRANSPORT OF DETAINED PERSON TO HOSPITAL 9.1. In event of emergency or short-term detention the responsibility for making arrangements for transfer to hospital lies with the medical practitioner who has issued the certificate. The receiving service will assume responsibility for making arrangements once informed of the detention by the GP or AMP, but responsibility for the care of the detained person remains with the medical practitioner until the person is admitted to hospital. 9.2. GP or AMP should inform the duty doctor at the appropriate receiving hospital, giving patient details, confirmation of detention, and their own contact phone number as well as requesting an escort and transportation for the detained person. Duty doctor will ascertain whether there are any particular requirements or risks that will affect the arrangements for transport. 9.3. The duty doctor in turn should contact the nurse in charge of the unit passing on the contact phone details and any other information about the situation that is available. The charge nurse will organise escort and transportation and then contact the GP or AMP to confirm arrangements and timescales. 20 9.4. Responsibility for the care of the patient remains with the GP or AMP until the person is admitted to hospital. In practice in the community this will mean until the escort and transport arrive. In general they will remain at the scene until the escort and transport have arrived and the detained person has safely left the scene. GP or AMP may only normally leave the scene if they are satisfied that situation is safe and there are appropriate others prepared to take responsibility until the escorts arrive. Appropriate others would include assessment team staff or community mental health staff and would not normally include relatives or carers. 9.5. In the event of a medical practitioner being called to another emergency, they will need to make a judgement about the relative clinical risk in the two situations. If another situation requires their immediate attendance they will try to ensure that any risks in the Psychiatric emergency situation are being managed effectively and will return as soon as possible unless the person has been transported to hospital. The responsibility for care in these situations remains with the medical practitioner but it is accepted that the duty to care for others may require a judgement to be made about priority. 9.6. Transportation will normally be provided by the Ambulance Service in these circumstances. Arrangements should be made for escorts to go directly to the scene using a taxi and the Ambulance Service is asked to prioritise collection of detained person and escorts from the scene. In such circumstances the Ambulance Service will treat transport of escorted patient to hospital as an emergency. 9.7. There may be circumstances – particularly in some situations where there is less urgency – where the use of a taxi or other transport would be safe, would hasten process and be less distressing for the person involved. The responsibility for deciding whether a proposed arrangement is acceptable lies with the medical practitioner that has issued the certificate, but the decision to use an alternative transport can only be taken if all those involved (Doctor, nurse escort, relatives etc) agree. Under no circumstances will a detained person be transported to hospital by car unless somebody other than the driver is able to sit with them and is confident that they will be able to ensure the detained persons safety. 9.8. If there are no beds at the appropriate hospital the Bed Management Policy will be followed. Site page-holder will take responsibility for finding a suitable bed elsewhere. If a bed is available at an alternative site within Lanarkshire the page-holder should then pass responsibility to the admitting hospital to make arrangements for the escorts to attend from that hospital and the transport to take person directly to the place the bed is available. 21 9.9. If no bed is available within Lanarkshire and detention is an emergency completed by a GP, the site page-holder will make arrangements for the detained person to be escorted to their local hospital for examination by duty psychiatrist. If appropriate, the page-holder will then identify a bed as per Lanarkshire Psychiatric Bed Management Policy. The duty doctor or in most cases duty consultant may then need to negotiate admission with alternative site. Generally the hospital to which the person would normally have been admitted should then take responsibility for the escort and transport to the boarding hospital. 10. MEDICAL TREATMENT IN EMERGENCY 10.1. There will be very few situations where the use of emergency sedation is appropriate or justified in the community during a crisis situation. If risk is deemed high and urgent action is required then the Police should be called to assist in rapid transport to Place of Safety. 10.2. The Act does not have any provisions that allow emergency medical treatment in the community. Section 243 allows for administration of medication without consent once a person has been detained in hospital. Section 243 of the Act allows the administration of medical treatment, without consent to Save the patients life Prevent serious deterioration in the patients condition Alleviate serious suffering on the part of the patient Prevent the patient behaving violently and / or being a danger to themselves or others. Following this treatment the administering doctor has a responsibility to inform the Mental Welfare Commission of their action within 7 days. 10.3. Where the GP or AMP in consultation with nurse escort on arrival assess that there is a high level of risk of harm to patient or others through disturbed or violent behaviour and there is no alternative, a decision may be taken to administer emergency medication. Such an action will be taken as a common law decision and is not covered by the mental health act but it would be good practice to ensure that the criteria described in section 243 have been met. 10.4. Where the need to administer urgent medical treatment does arise a decision to provide urgent treatment will be based on professional judgement. However, it is important to recognise that the assessment of the likelihood of ‘serious deterioration’ and ‘serious suffering’ is a subjective process. A person who is experiencing symptoms and behaviours as a result of mental disorder can be difficult to manage and may become oppositional or verbally aggressive or abusive. It would be expected that such behaviour would not, in itself, be seen as criteria for the giving of urgent medical treatment. 22 10.5. The decision to administer urgent medical treatment should therefore be informed by the presence of the criteria listed at Section 243 of the Act rather than as a means of managing a “difficult” person. The use of sedative medication will be restricted to exceptional circumstances and will not be used as a way of subduing a person who is difficult to manage or is demanding of staff time and attention. 10.6. If sedation is required a short-acting benzodiazepine will be the drug of choice. The attending medical practitioner is responsible for prescription and administration of emergency medication. If medication is administered under common law there is no requirement to provide a report to the Mental Welfare Commission. 11. ADMISSION TO HOSPITAL 11.1. The GP or AMP must ensure the emergency or short term certificate is given to the Hospital Managers before the patient is admitted, as the patient’s detention in hospital is only authorised when the certificate is given to the Hospital Managers. 11.2. For these purposes the Nurse in charge of the admitting ward will be deemed to be acting on behalf of Hospital Managers and is authorised to receive the certificates. 11.3. Nurses providing escort may convey the certificate to hospital on behalf of the GP or AMP. 11.4. If the patient is brought to hospital by other means (e.g. Police) it remains the responsibility of GP or AMP to ensure certificate arrives before admission takes place and this will normally mean the GP or AMP delivering the certificate themselves. In such circumstances it would be good practice for the GP or AMP to attend the ward anyway to ensure effective handover of relevant clinical information. 11.5. A patient’s initial experience of hospital and detention can be influenced considerably by the procedures involved with the admission 11.5.1. Patient’s should be treated with sensitivity and respect and afforded the greatest degree of privacy achievable. 11.5.2. Wherever possible, a member of ward staff should be available to offer support and explain all relevant procedures to the patient. 11.5.3. It is good practice for the patient to be allocated a named nurse who is available to them at the time of the admission. 11.5.4. It is also good practice to provide the patient with an information pack. This is in addition to the Hospital Managers’ statutory duties under Section 260. 23 11.6. MHO actions following the Admission of a Patient. Where the MHO has given consent to a detention certificate, along with others, they will wish to take steps to ensure the following: 11.6.1. The patient is aware of their rights and status 11.6.2. The patient has access to information on representation including advocacy and where necessary is provided with assistance to contact these services. 11.6.3. The patient has access to interpretation and translation services or services that address other communication needs, as required. 11.6.4. The patient and any carers or dependants have the contact details of a MHO 11.6.5. Ward staff and the patient’s AMP have contact details for a MHO and any known details of a Named Person or Advance Statement. 11.6.6. The patient’s AMP and Hospital Managers are notified if the patient has a Financial or Welfare Attorney or Guardian and their contact details. 11.6.7. The needs of any carers or relevant family members are addressed at this time and suitable arrangements for on-going support and follow up are put in place. In particular, the MHO will wish to ensure that any carer is informed of their right to have their needs assessed and arrangements are made to undertake this where requested. 11.6.8. The needs of any children or need for child care support must be addressed and referral made to appropriate children’s services as required. 11.6.9. The MHO must consider whether any remaining adults (within the household or otherwise dependant) have become vulnerable as a result of the patient’s admission to hospital, and must take appropriate action in accordance with the Vulnerable Adults Procedure. 11.6.10. The MHO must be satisfied that the responsibilities of the local authority under the National Assistance Act 1948 are met in respect of any need to take steps to protect the patient’s property or arrange for the alternative care of pets. 11.7. Further details on procedures to be followed after admission are contained in the appropriate detailed procedure documents. 24 12. USE OF DETENTION (EMERGENCY AND SHORT TERM) IN THE HOSPITAL 12.1. This section of the PEP gives an outline of procedures to be followed when a person is deemed to meet criteria for detention but is already in hospital. It covers procedures in Psychiatric wards but can also be applied in Accident and Emergency departments and other wards of the hospital. 12.2. In a hospital situation the Short Term Detention Certificate remains the gateway order of choice for the reasons previously stated. 12.3. Any registered medical practitioner can issue an Emergency detention certificate provided the criteria outlined in section 36 (see para 8.5) are met. It is advised that they contact the duty Psychiatric team for advice before doing so. In situations of clinical urgency, a medical practitioner working at grade of SHO or more senior in Accident and Emergency or any other hospital department can issue a certificate without referral to the duty psychiatrist. They must still make every effort to consult an MHO prior to detention. If this is not possible they must provide a report detailing why to Hospital Managers who will pass this to Mental Welfare Commission and relevant Local Authority. 12.4. In most cases where detention is being considered in hospital it will be possible to seek advice of the duty psychiatrist or the Psychiatric Assessment Team. They will attend and make assessment where possible or offer advice on appropriate action if not able to attend immediately. 12.5. During working hours (mon-fri 9am –5pm) each locality will have a duty Approved Medical Practitioner who will attend in event of a potential detention. If duty AMP engaged in an assessment in the community and no other AMP immediately available then the hospital duty psychiatrist, usually and SHO or staff grade will attend and advise. 12.6. Out-of-hours, the initial referral will be to the on-call duty psychiatrist for the hospital, who may be resident or non-resident. 12.6.1. If the duty psychiatrist is resident they will be expected to attend a situation where potential detention is required immediately. 12.6.2. If the patient is in A & E or a non-psychiatric hospital ward and the duty psychiatrist is non-resident or occupied with another situation, where detention a possibility, telephone advice will be given and the Psychiatric Assessment Team will assist. 12.6.3. If the patient is in a psychiatric ward and duty psychiatrist is nonresident or occupied with another situation where detention a possibility, consideration should be given to using Section 299 of the Act – Nurses Holding Powers. 25 12.7. Nurses Holding Powers 12.7.1. Section 299 allows a nurse of prescribed class RMN & RNLD to detain a patient pending medical examination to determine whether an Emergency Detention Certificate or Short Term Detention Certificate should be granted. Form NUR1 should be completed in these circumstances. 12.7.2. The class of nurse prescribed is a nurse registered in Sub-Part of the Nurses' Part of the register established and maintained in accordance with article 5 of the Nursing & Midwifery Order 2001; entry includes an entry to indicate that: a) the nurse has a recordable qualification in mental health nursing or learning disabilities nursing; b) the nurse's field of practice is mental health nursing or learning disabilities nursing 12.7.3. They can only hold a patient who is currently in a Psychiatric ward, not A&E or any other ward of the hospital. 12.7.4. A patient may only be detained by a nurse if he/she believes it to be likely: that the patient has a mental disorder; that it is necessary for the protection of the health, safety or welfare of the patient or for the protection of the safety of any other person for the patient to be immediately restrained from leaving the hospital; that it is necessary to carry out a medical examination of the patient to determine whether an emergency or short-term detention certificate should be granted; and that the patient is not already detained that it is not practicable to have the patient examined immediately by a medical practitioner. 12.7.5. The “holding period” lasts for up to 2 hours to allow a medical practitioner to attend. 12.7.6. If the Medical Practitioner arrives during the second hour of the holding period, a further 1-hour holding period from the time of the medical practitioner arriving comes into force to allow time for examination. 12.7.7. A written record must be made in nursing notes stating why the patient was detained, the time the holding period began and the reasons for detention 26 12.8. 12.7.8. Notification of must be made to the on call Mental Health Officer and the Hospital Manager as soon as practicable after the holding power begins by the nurse applying the holding period. 12.7.9. The Hospital Managers must make notification to the Mental Welfare Commission within 14 days. Involvement of MHO in hospital detentions 12.8.1. On receipt of referral from A&E, another hospital ward or from nursing staff on psychiatric ward identifying possible requirement for detention the duty AMP or psychiatrist should contact the duty MHO and advise them of details. 12.8.2. In situation of acute risk, where for example patient is being restrained, the duty psychiatrist may decide to apply emergency detention certificate without consultation and provide report to Hospital Managers. 12.8.3. In all cases in working hours, the duty MHO will attend and assess with AMP whether a short term detention certificate should be issued. Out of hours the duty MHO must be consulted, unless it is not practicable to do so and arrangements made to assess the patient. 12.9. Decision to grant an emergency detention out-of-hours 12.9.1. If the duty psychiatrist decides to grant an emergency detention certificate in any part of the hospital, with or without consultation with MHO they must inform the duty consultant and discuss next steps. 12.9.2. Duty consultant should check that arrangements are in place so that an AMP will review detention as soon as practical. In most cases that will be the next day (including weekends). This may involve telephone “hand-over” to duty consultant at 9am the following day or to local duty AMP if next day is a working day. 12.10. Duties of AMP as soon as practical following emergency detention 12.10.1. Duty AMP (one for all Lanarkshire at weekends, one for each locality during working week) should contact duty MHO to discuss arrangements for review of any patients detained. 12.10.2. Duty AMP must ensure that any patients detained in nonpsychiatric wards are also reviewed. These patients cannot be discharged by non AMP medical/surgical consultants until their detention has been reviewed by an AMP. 27 12.10.3. Where Short Term Detention is thought necessary and MHO gives consent, AMP should complete form DET2 and pass to Hospital Managers. 12.10.4. Where emergency detention is revoked, the duty AMP should complete form REV1 and pass this to the Hospital Managers. Patient may remain in hospital as an informal patient or be discharged at this point. 28 APPENDIX 1 – AMP AVAILABILITY Approved Medical Practitioners are those approved under section 22 of Mental Health (Care and Treatment) (Scotland) Act. Consultant Psychiatrists and most staff grade psychiatrists meet criteria and will be approved once they have completed a designated training course. Short Term Detention is the preferred gateway order and requires an AMP. AMPs must also review any Emergency Detention “as soon as practicable” and a person detained as an emergency on a medical or surgical admission ward cannot be discharged until an AMP has revoked detention. Each of the three localities in Lanarkshire will therefore designate a duty AMP that will remain available to perform these duties for those aged 16-65. For advice for under 16’s contact should be with local Child and Family Clinic and for those aged over 65 with appropriate Old Age Psychiatry Team. The duty AMP will normally cover a working week from 9am till 5pm Monday to Friday. Outwith these hours the duty consultant will also be duty AMP. Rotas will be maintained by or on behalf of lead clinician on each site. On Saturdays, Sundays and on public holidays duty consultant will normally attend to review any patients admitted on emergency detention the previous night Role of duty AMP. To assess those detained as an emergency “as soon as practicable”, whichever hospital ward they are in. To be available to discuss referrals from General Practitioners where immediate detention may be considered. If appropriate to then visit within an agreed timescale – same working day is minimum standard – to assess in consultation with MHO whether short term detention appropriate. To be available to discuss cases assessed by PAT team or court liaison team where detention may be required. If necessary to visit and assess these patients along with duty MHO. . Duty AMP can be contacted using the following numbers: Monklands / Cumbernauld area Motherwell / Clydesdale Hamilton / East Kilbride 01236 748748 01698 245000 01355 585000 during working hours and on 01698 24500 out-of-hours 29 APPENDIX 2 – MHO AVAILABILITY Local authorities have a duty under Section 32 Mental Health (Care & Treatment) (Scotland) Act (2003) to ensure that Mental Health Officers (MHO) are available to discharge their duties and responsibilities in respect of the Mental Health Act (2003), Adults With Incapacity (Scotland) Act (2000) and the Criminal Procedures (Scotland) Act 1995.Mental Health Officers will play a significant role in many parts of the new Act, similar to the role they played under the 1984 Act but greatly extended. Short Term Detention is the preferred gateway order and AMP’s must consult and gain the consent of a MHO. Emergency Detention Order is an option available to medical practitioners where it is necessary as a matter of urgency to detain the person for assessment. It is no longer appropriate to seek consent from a relative and the services of a MHO should be accessed where practicable. 1 North Lanarkshire Arrangements North Lanarkshire Council has 33 MHO’s dispersed across various care setting within the council. A duty rota is in operation and each area has a worker available for interventions under the Act. From 8-45am to 4-45pm Monday to Thursday and 8-45am to 4-15pm on Friday the Duty Mental Health Officer can be accessed by contacting: Social Work Headquarters at 52-60 Merry Street, Motherwell, ML1 1JE Telephone number 01698 332662 or 01698 332299. Libby McGhie or David McLean will take all relevant details and contact the duty MHO for your area. The MHO will then contact the Medical Practitioner to discuss the referral. 30 2 South Lanarkshire Arrangements Mental Health Officer Rotas in South Lanarkshire are being circulated to all likely to require them. The co-ordinators for the rotas are the Senior Social workers in the Community Mental Health Teams details below. Anne Marie Mitchell CMHT Hamilton/Blantyre David McCorrison Clydesdale Resource Network Rosaline McGarry CMHT East Kilbride/Strathaven Gwen Scott CMHT Rutherglen/Cambuslang 3 9 High Patrick Street, Hamilton, ML3 7ES Lanark Health Centre, Woodstock Medical Campus, Woodstock Road Lanark, ML11 7DH 4th Floor, Atholl House, Churchhill Avenue, East Kilbride, G74 1LU Eastvale Resource Centre, 130A Stonelaw Road, Rutherglen, G73 2PQ Tel : 01698 455459 Mobile: 07795 090372 Tel : 01555 667159/667160 Mobile: 07795 090367 Fax : 01698 454870 Tel : 01355 233354 Mobile: 07795 090366 Fax : 01355 576524 Tel : 0141 531 4117 Mobile 07795 454719 Fax : 0141 531 4107 Fax : 01555 667180 Out of Hours services – both council areas West of Scotland Social Work Standby Service offers an emergency Social Work Service including Mental Health Officer Services. The Priority contact telephone number for Lanarkshire Health staff to access a MHO is 0141 305 6900 To access the West of Scotland Social Work Standby Service for other services please contact 0141 305 6920. . 31 DRAFT 200905 APPENDIX 3 LANARKSHIRE PSYCHIATRIC EMERGENCEY PLAN: INTERPRETATION & SUPPORTED COMMUNICATION SERVICES SUMMARY PROCEDURES 1 Introduction 1.1 The following guidelines are developed as a quick reference for staff, they do not replace any existing interpreting policy or procedures. Staff should make themselves aware of existing interpreting policies and procedures, appropriate to their respective organisations, via their line manager. 1.2 Staff should provide interpreting services appropriate to the needs of individual clients. These needs may be best met by: A signer or lip reader An interpreter 1.3 A professional/independent interpreter should be used to provide interpreting services in relation to assessment and decision about care and treatment, see section 2 to 5 below. The following information should be recorded in the person’s notes: Who provided interpretation, including interpreter’s I.D code? What method was used i.e. face to face or via a telephone interpreting service such as Language Line? 1.4 If a non-independent interpreter was used i.e. member of staff or family member, the record should note: What efforts were made to access an independent interpreter? The reason for proceeding with the assessment or interview rather than waiting for an independent interpreter? Who provided interpreting and their relationship to the person? Any conflicts of interest? Any difficulties accessing interpreting services should be brought to the attention of the appropriate head of service for the respective organisation. 1.5 To support consistency, every effort should be made to use the same interpreter throughout the duration of the persons care and treatment, if the client wishes. 1.6 Dungavel Detention Centre use Global Interpreting Services to provide interpreting for the people detained there. When a detainee requires services out-with the centre Global Interpreting Service continue to provide the interpreting. 2 Procedure 2.1 Staff may become aware of the requirements for interpretation or supported communications services: At the time of referral At the time of appointment At the point of admission or emergency assessment At the point of attendance at Hospital or Clinic 2.2 It is important that arrangements for interpretation services be put in place at as early a stage as possible. 32 3 Non-Emergency/ Non-Urgent Circumstances 3.1 In non-emergency/ non-urgent circumstances the following numbers should be contacted to arrange professional interpretation or supported communication services: ORGANISATION SERVICE NHS Lanarkshire Linkline Monday – Friday 9am – 5pm – who will secure the services of an interpreter. Where possible staff should arrange through Line manager. CONTACT 01698 855588 Out of hours answer machine available outside business hours for non-urgent requests North Lanarkshire Council South Lanarkshire Council Strathclyde Police Scottish Ambulance Service 3.2 In the event of the client’s attendance being cancelled or changed, staff must notify the appropriate organisation on the number above, immediately to enable alternative arrangements to be made. 4 Emergency/ Urgent Circumstances 4.1 In the event of an emergency or when no advance notice is given, staff should contact the following numbers to arrange interpretation or supported communication services: ORGANISATION SERVICE CONTACT NHS Lanarkshire Linkline Monday – Friday 9am – 5pm 01698 855588 Out of hours answer machine available outside business hours for non-urgent requests. Strathclyde Hospital Switchboard (Out of hours emergencies) 01698 245000 North Lanarkshire Council South Lanarkshire Council Strathclyde Police Scottish Ambulance Service 33 5 Using Interpretation Service 5.1 The interpretation services are designed to be straightforward and easy to use however the following guidelines are provided by Language Line to facilitate the interpretation process. Interpretation can be provided both face to face and via telephone interpreting. It is likely that telephone interpretation will be used in most emergency circumstances. Here are the step-by-step guides for using both: 5.2 Telephone interpreting - a simple 4 step process: Step 1: Identify the language required (a language card may help) Step 2: Call the appropriate number for the service Step 3: Brief the interpreter Step 4: Speak directly to your client 5.3 Face to Face interpreting - a simple 6 step process: Step 1. Identify the language required Step 2. Call the appropriate number to book the interpreter Step 3. Brief the interpreter before they attend the interview Step 3. Arrange the meeting room for maximum clarity and comfort Step 4. Introduce the interpreter and set the scene Step 5. Speak directly to your client Step 6. Debrief the interpreter once the conversation is finished 34