Evaluation of a Physiological Strain Index for use During Intermittent
advertisement

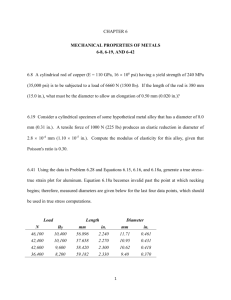
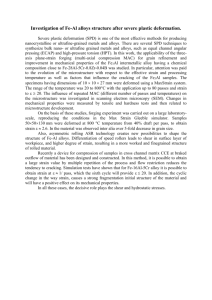
Intermittent exercise in the heat 22 JEPonline Journal of Exercise Physiologyonline Official Journal of The American Society of Exercise Physiologists (ASEP) ISSN 1097-9751 An International Electronic Journal Volume 4 Number 3 August 2001 Environmental Exercise Physiology EVALUATION OF A PHYSIOLOGICAL STRAIN INDEX FOR USE DURING INTERMITTENT EXERCISE IN THE HEAT R.W. GOTSHALL, D.J. DAHL AND N.J. MARCUS. Health and Exercise Science, Colorado State University, Fort Collins CO 80523. ABSTRACT R.W. GOTSHALL, D.J. DAHL AND N.J. MARCUS. Evaluation Of A Physiological Strain Index For Use During Intermittent Exercise In The Heat. JEPonline. 2001;4(3):22-29. A physiological heat strain index that includes a combination of heart rate and core temperature has been proposed as an index of heat strain for use to monitor heat strain during continuous, steady-state exercise. The current study evaluates this physiological heat strain index during work-rest, intermittent, exercise in the heat. Ten subjects each participated in either a 60-minute steady-state or 60-minute intermittent (15 min exercise, 5 min rest; repeated 3 times) exercise protocol in normal (20oC, 50% RH), hot-dry (40oC, 35% RH), and hot-humid (35oC, 70% RH) conditions. Exercise was walking on the treadmill at 1.34 m/sec (3 mph), 5% grade. Heart rate was determined with a heart rate monitor and core temperature was determined by rectal temperature probe. The physiological heat strain index was calculated from heart rate and core temperature. The physiological heat strain index distinguished between normal and heat conditions for both protocols. However, only the steadstate exercise protocol resulted in physiological heat strain differences between hot-dry and hot-humid conditions. Heat strain was less for the intermittent protocol. The results confirm previous investigations using the physiological heat strain index during steady-state exercise in the heat, and extend the usefulness of this index to intermittent, work-rest, exercise in the heat. Keywords: Stress, Work, Environment, Humidity, Thermoregulation, Core Temperature, Heart Rate INTRODUCTION While indices of heat stress have become widely used in occupational settings (1), attempts at developing adequate indices of heat strain have been less successful (5-7). The onset of heat-related injury is insidious. Athletes, military personnel, firefighters, and other industrial workers often continue to perform unaware that they are, or are rapidly becoming, victims of hyperthermia (3). From 1979 through 1996, the Centers for Disease Control reported 6864 deaths attributed to excessive heat exposure, though not all of these occurred in those at work or exercising (3). The increased need for workers to wear heavy, impermeable clothing while Intermittent exercise in the heat 23 working in hot environments has the potential to increase heat-related injuries. In 1994, the US Air Force reported 19 individuals hospitalized due to excessive heat exposure (4). That same year, the US Army reported 196 individuals hospitalized for heat illness (4). To ameliorate risk for workers and athletes who perform in the heat, both environmental heat stress and physiological heat strain are important to consider. In order to effectively monitor the physiological heat strain, physiological variables must be included. However, these variables should be combined to produce an effective heat strain index for use across environments. Therefore, a simple, easily calculated physiological strain index for use in hot environments that would provide rapid and accurate assessment of heat strain potentially could reduce the risk of heat exposure. Moran et al. (11) have developed a physiological heat strain index (PSI) that places the heat strain on a scale of 0 through 10. This potentially standardizes the interpretation of the heat strain across individuals and environments. Moran and colleagues (8-11) have evaluated the PSI under a variety of hot environmental conditions, primarily using database information on subjects who had exercised continuously in the heat. Their data are convincing in that the PSI discriminated among the various hot, hot-humid, and normal conditions. In one prospective study whose primary purpose was to investigate the potential influence of gender on the PSI, the PSI again was able to discriminate among the environmental conditions (10). Most work environments and protocols do not involve continuous, steady-state exercise, but rather, work-rest cycles. Monitoring of heat strain during intermittent exercise is especially important for those individuals wearing protective clothing while working in the heat, in which rest cycles are mandatory. The PSI is an index of the physiological strain and should track the changes in heat strain occurring as rest cycles are employed. The concern lies in the use of Tr in the setting of work-rest cycling. Tr is usually greater and responds more slowly than the Tesophogeal (12-14) to changes in work intensity. Tr responds to changes in blood temperature with a time constant of ~12 min, while Tesophogeal, for comparison, responds with a time constant of about ~1 min (14). Thus, there is the concern that the PSI might not reflect the heat strain associated with work-rest cycles during an intermittent exercise protocol due to a failure of Tr to change. However, because the PSI includes HR as well as Tr, it was hypothesized in this study that the changes in HR associated with work-rest cycles might obviate this concern. It was reasoned that HR would respond to work-rest cycles reflecting the changes in metabolic heat production, and more appropriately correspond to heat strain. Therefore, the purpose of this study was to evaluate the PSI under varying hot-humid conditions in subjects performing continuous, steadystate exercise or performing work-rest cycles. We hypothesized that the PSI would effectively discriminate among the environmental conditions during both continuous and intermittent exercise. METHODS Prior to the onset of this study, approval was obtained from the Colorado State University Human Research Committee and all procedures were in accordance with the ethical standards of the Helsinki Declaration of 1975. Twelve men and eight women volunteered for this study. All subjects were apparently healthy as ascertained by health questionnaire. Subjects were regularly exercising a minimum of 3 days per week, 1 hour per day, for at least the last 6 months. Subjects with a history of heat-related illness were not eligible for the study. Subjects refrained from exercise, alcohol, and over-the-counter medication for 24 hours and from caffeine for 12 hours prior to each test period. Prior to the environmental exposures, each subject performed a maximal exercise stress test using a modified Balke protocol on a Quinton Q65 treadmill (Quinton, Seattle, WA). Exercise ECG was recorded for heart rate and rhythm determination. Expired gases were collected and analyzed using a TrueMax 2400 metabolic cart (ParvoMedics, Sandy, UT). Intermittent exercise in the heat 24 Subjects were divided into two groups of 6 men and 4 women for the two different exercise protocols, continuous, steady-state exercise (SS) and intermittent exercise (INT). Each subject was exposed in an environmental chamber to each of three environmental conditions in random order, normal (N: 20oC, 50% RH), hot-dry (HD: 40oC, 35% RH), and hot-humid (HH: 35oC, 70% RH). Following 10 min of seated rest data collection, the SS subjects walked on the treadmill at 1.34 m/s (3 mph), 5% grade for 60 min. The INT group walked on the treadmill under the same conditions, but walked for a 15-min interval followed by 5-min interval of seated rest repeated up to the 60 min of total time. Prior to entering the environmental chamber, each subject was weighed in the nude; dressed in t-shirt, shorts, running shoes and socks; and instrumented for physiological measurements. A rectal temperature probe (YSI, Yellow Springs, OH) was self-inserted 10 cm passed the anal sphincter. A Polar heart rate monitor (Polar, USA) was placed around the chest. Core (rectal) temperature (Tr) and heart rate (HR) were recorded continuously via AcqKnowledge v3.5.3 acquisition software (Biopac, Santa Barbara, CA) and stored on computer. Core temperature of 39oC or HR in excess of 180 b/min would have terminated the heat exposure trial. No trial had to be terminated. Tr and HR were averaged for the last 90 sec of rest, and for 60 sec at 5, 30 and 60 min of exercise for the SS protocol. Tr and HR were averaged for the last 90 sec of rest, and for the last 60 sec of each of the exercise and subsequent rest periods for the INT protocol. Each subject was permitted water ad libitum. A weighed filled water bottle was provided that was again weighed after the exposure to determine amount consumed. Subjects immediately exited the chamber upon completion of the protocol, stripped, towel-dried, and obtained a nude body weight. Sweat loss and rate were calculated by subtraction of the post-bodyweight from the pre-body weight corrected for water consumption. The physiological strain index (PSI) was calculated according to Moran et al. (11). The equation used was: PSI = (5 * (Tri - Tr0)/ ((39.5 - Tr0)) + (5 * (HRi - HRo) * (180-HR0)) Where Tri and HRi are simultaneous measurements taken at any time during the heat exposure; and Tr0 and HR0 are the seated resting values in the chamber prior to beginning the exercise protocol. The PSI yields values between 1 and 10 when values for HR and Tr fall between 60-180 bpm and 36.5o-39.5oC, respectively. A two-way (time, climate), repeated measures ANOVA was used for each of the two groups to analyze variables for the three climatic exposures. Where differences were found, post hoc analysis was performed with Fisher's LSD Multiple Comparison Test. For comparisons between the two groups, a two-way (time, group) ANOVA was used for each climatic exposure, with the Fisher's LSD Multiple Comparison Test used for post hoc analysis. All statistics were accomplished with NCSS2000 software (NCSS Kaysville, UT). Significance was set at p<0.05. RESULTS Table 1 presents the subject's characteristics. There were no significant differences between the two groups. Table 2 shows the volume of sweat lost for each climatic condition for each group. While there were significant increases in sweat loss for both HD and HH compared to N for both groups, there were no differences between HD and HH for either group. Sweat loss was the same for both SS and INT groups for each climatic condition. Intermittent exercise in the heat 25 Table 1. Subject Characteristics. SS, n=10 INT, n=10 Age (years) 251.0 241.0 Height (cm) 1773.2 17.6 Weight (kg) 69.34.4 74.55.4 VO2MAX (mL/kg/min) 50.72.2 49.22.4 Values are mean SEM. SS, continuous, steady-state exercise protocol; INT, intermittent exercise protocol. Table 2. Sweat loss in each of the climatic conditions (mL). SS INT N 19463 312114 HD 86953* 1125330* HH 871112* 1075340* Values are mean SEM. SS, continuous, steady-state exercise protocol; INT, intermittent exercise protocol; N, normal climate; HD, hot-dry climate; HH, hot-humid climate. *p<0.05, compared to N. Figure 1 presents the HR, Tr, and PSI data for SS exercise. HR was higher while resting in HD and HH conditions. HR was elevated with the SS exercise, being more elevated during HD and HH, and becoming highest in HH by 60 min. Core temperature, Tr, was the same at rest for N and HD, but slightly lower for HH. All Tr values increased with exercise, reaching higher levels with HD and HH than for N. No differences in exercise Tr values were detected between HD and HH. The PSI rose with exercise, but increased more with HD and HH. PSI for HH was greater than HD by 60 min of SS exercise. For intermittent exercise (Figure 2), HR was again slightly higher than N at rest in HD and HH. With exercisesit cycles, HR increased and declined with exercise and sit, respectively, for all conditions. During the exercisesit cycles, HR was highest for HD and HH, but not different between them. Tr was the same for all conditions and did not change significantly over the 60 min for any condition. PSI increased with exercise and declined with sitting rest throughout the 60 min. PSI remained higher during HD and HH, but not different between these two conditions. Table 3. Comparison of continuous (SS) and intermittent (INT) protocols for heart rate, core temperature and physiological strain index. Condition SS INT N HD HH N HD HH Heart Rate (b/min): Rest 663 795 755 685 755 756 Peak 984 1197 1238 968 1149 12010 Core Temperature (C): Rest 37.10.1 37.20.1 36.90.1 37.10.1 37.30.1 37.00.2 Peak 37.40.1 37.80.1 37.70.1 37.40.1 37.70.1 37.40.3 Physiological Strain Index: 0 0 0 0 0 0 Rest Peak 2.00.2 3.40.3 3.80.4 1.90.2 2.80.2* 2.90.4* Values are mean SEM. *p<0.05, compared to corresponding SS climatic condition. Intermittent exercise in the heat 26 Figure 1. Responses of heart rate, rectal temperature and physiological strain index to continuous, steady-state exercise in three climatic conditions. Values are means SEM. Significance among climatic conditions is indicated for each time period by letter, dissimilar letters are significantly different at p<0.05. Same letters are not different from one another. Table 3 shows the comparison of resting and peak values for HR, Tr, and PSI between the two exercise protocols, SS and INT. Resting and peak HR were similar between the two protocols, as were Tr values. PSI was less for INT during HD and HH than for SS under the same conditions. DISCUSSION Heat stress is the combination of environmental and physical work factors that constitute the heat load on an individual while working. Heat strain is the physiological response to the heat stress that includes the direct effect of the heat load on the body, as well as the compensatory thermoregulatory responses to the heat stress. Heat stress increases the risk of increased frequency of accidents and therefore the safety of workers. Additionally, the risk of heat-induced disorders such as heat cramps, heat exhaustion, and heat stroke increases with additional heat stress. Finally, worker productivity is lowered by heat stress and the work-rest cycles employed to reduce heat strain (1,2). The goal of any program developed for working in the heat, especially for Intermittent exercise in the heat 27 those requiring protective clothing, is to optimize productivity while maximizing safety and minimizing health risks of individuals. Thus, effective monitoring of physiological heat strain would permit the determination of the level of heat strain relative to threshold limit values (TLV) (1), thereby optimizing the worker's work/rest cycles and minimizing risk. Figure 2. Responses of heart rate, rectal temperature and physiological strain index to intermittent exercise in three climatic conditions. Values are means SEM. Significance among climatic conditions is indicated for each time period by letter, dissimilar letters are significantly different at p<o.05. Same letters are not different from one another. It was hypothesized that the combining of HR and Tr within the PSI would make the PSI applicable to the setting of work-rest cycles in the heat. The results of this study indicate that the PSI was effective in distinguishing between the normal condition and both conditions in the heat. Furthermore, the PSI increased and decreased accordingly with work and rest, respectively. Tr did not reflect these cycles, but HR did. Therefore, the PSI appropriately indicated heat strain during both SS and INT protocols. In the present study, the PSI discriminated between HD and HH conditions by 60 minutes of SS exercise, confirming previous studies (9). In contrast, the PSI did not discriminate between these two conditions during Intermittent exercise in the heat 28 the intermittent exercise protocol. The question is whether this an accurate depiction of the differences in heat strain between the two protocols involving these environmental conditions, or whether the INT protocol reduced the ability of the PSI to distinguish between these two heat conditions. In evaluating the individual indicators of heat strain, HR and Tr, there were no differences indicated between INT and SS protocols with regard to peak values obtained (Table 3). While, HR was different for these two climatic conditions during SS, and not during INT. As seen in table 2, the overall heat strain was greater for the steady-state exercise than for the intermittent protocol. Therefore, it is likely that the PSI is appropriately documenting the lesser heat strain of the INT protocol. Additionally, the difference in heat strain between HD and HH during INT exercise is small and likely not detected by any of the measures of heat strain. It is not surprising that INT exercise generates less heat strain than SS exercise, as heat is permitted to dissipate from the individual during the rest cycle and there is less heat produced metabolically. In conclusion, this study has confirmed the use of the PSI in representing heat strain during continuous exercise in the heat. The results also indicate that the PSI appropriately documents heat strain during intermittent exercise. The ease of calculation and scaling of the PSI make it attractive as a monitor of heat strain under a variety of exercise and work conditions. Address for Correspondence: Robert Gotshall, Ph.D., Professor, Health and Exercise Science, Colorado State University, Fort Collins, CO 80523-1582; Phone: (970) 491-6374 ; FAX: (970) 491-0445 ; email: gotshall@cahs.colostate.edu REFERENCES 1. American Conference of Governmental Industrial Hygienists. TLVs threshold limit values and biological exposure indices for 1985-86. 91-98. 1991. Cincinnati OH, ACGIH. 2. Belard JL, Stanevich RL. Overview of heat stress among waste abatement workers. Applied Occup Environ Hygiene 1995;10(11):903-907. 3. Centers for Disease Control and Prevention. Heat related illness and deaths- Missouri, 1998 and United States, 1979-1986. Morbid Mortal Weekly Rep 1999;48:469-473. 4. Gardner JW, Amoroso PJ, Grayson JK, Helmkamp J, Jones BH. Hopitalizations due to injury: Inpatient medical records data. Milit Med 164,5-6-5-143. 1999. 5. Gonzalez RR, McLellan TM, Withey WR, Chang SK, Pandolf KB. Heat strain models applicable for protective clothing systems: comparison of core temperature response. J Appl Physiol 1997;83(3):1017-1032. 6. Hubac M, Strelka F, Borsky I, Hubacova L. Application of the relative summary climatic indices during work in heat for ergonomic purposes. Ergonomics 1989;32(7):733-750. 7. McArdle B, Dunham W, Holling HE, Ladell WSS, Scott JW, Thompson ML et al. The Prediction of the Physiological Effects of Warm and Hot Environments: The P4SR Index. R.N.P. 47/391. 1947. London, Medical Research Council. 8. Moran DS, Horowitz M, Meiri U, Laor A, Pandolf KB. The physiological strain index applied to heatstressed rats. J Appl Physiol 1999;86(3):895-901. Intermittent exercise in the heat 29 9. Moran DS, Montain SJ, Pandolf KB. Evaluation of different levels of hydration using a new physiological strain index. Am J Physiol 1998;275:R854-R860. 10. Moran DS, Shapiro Y, Laor A, Izraeli S, Pandolf KB. Can gender differences during exercise-heat stress be assessed by the physiological strain index? Am J Physiol 1999;276:R1798-R1804. 11. Moran DS, Shitzer A, Pandolf KB. A physiological strain index to evaluate heat stress. Am J Physiol 1998;44:R129-R134. 12. Nielsen B, Nielsen M. Body temperature during work. Acta Physiol Scand 1962;56:120-129. 13. Saltin B, Hermansen L. Esophageal, rectal, and muscle temperature during exercise. J Appl Physiol 1966;21:1757-1762. 14. Sawka MN, Wenger BC, Pandolf KB. Thermoregulatory responses to acute exercise, heat stress and heat acclimation. In: Handbook of Physiology, Environmental Physiology. Bethesda MD: Am Physiol Soc, 1995:157-185.