Abouthialine_Final
advertisement

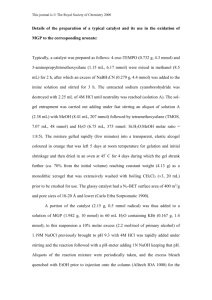
Preclinical Toxicology Studies with a Novel Antithyroid Medication Rafiq R. A. Abou-Shaaban1,* Malaz AbuTarif2, David R. Taft2 and Anthony P. Simonelli2 1 Faculty of Pharmacy and Health Sciences, Ajman University of Science and Technology, Abu Dhabi, United Arab Emirates 2 Division of Pharmaceutics, Long Island University, Brooklyn NY 11201 USA * Corresponding Author: Dr. Rafiq R. A. Abou-Shaaban Faculty of Pharmacy and Health Sciences Ajman University of Science and Technology Abu Dhabi Campus PO Box 5102 Abu Dhabi, United Arab Emirates Fax: +971-2-676-1828 Tel: +971-50-445-8952 Email: rafiq_a@hotmail.com Running Title: Preclinical Toxicology of Abouthioline Key Words: Abouthioline; Toxicology; Propylthiouracil; Methimazole; Preclinical -1- Abstract Abouthioline (1-Cyclohexyl-3(3-quinolyl)-2-thiourea) is a novel compound with antithyroid activity. Abouthioline was designed based on structure-activity relationships (E-state indexes) aimed at reducing the antioxidant properties of the compound by modification of acyclic thiourylene moiety. Antioxidant effects of currently available treatments (e.g., propylthiouracil, methimazole) are associated with an incidence of agranulocytosis and aplastic anemia. In the present study, the preclinical toxicology of abouthioline was determined in mice and rats and compared to several reference compounds (e.g., propylthiouracil, methimazole). Following short-term administration (7 days) to mice, ABL had minimal effects of on biochemical parameters, although significant reductions in both total protein and albumin were noted. Chronic toxicity studies (30 days) in rats revealed significant effects of abouthioline, propylthiouracil and methimazole on serum electrolyte and glucose levels. Abouthioline had no detrimental effects on hematologic parameters. However, total WBC count (propylthiouracil) and neutrophil levels (propylthiouracil and methimazole) were significantly decreased among other treatment groups. The results of this investigation suggest that abouthioline is a promising new antithyroid therapy with a reduced risk of hematologic toxicity that is associated with current pharmacological treatments. Further studies are warranted to assess the safety and efficacy of abouthioline. -2- Introduction Antithyroid medications are used throughout the world in the treatment of hyperthyroidism resulting from Graves’ disease (1,2). Antithyroid therapy is also indicated in patients with toxic adenoma or toxic multinodular goiter prior to chemical or surgical thyroidectomy (3). The most commonly prescribed antithyroid medications are the thionamides. Agents in this class include methimazole (MTH) and propylthiouracil (PTU). Thionamide medications are generally administered for long periods of time. While the incidence of adverse effects with antithyroid therapy is low, these medications are associated with severe hematologic toxicity including agranulocytosis and aplastic anemia (4-8). Agranulocytosis is a severe and life-threatening complication of thionamide therapy. Agranulocytosis is presumably an autoimmune reaction to circulating anti-neutrophil antibodies and lymphocyte sensitization to antithyroid medications. The presence of a cyclic thioamide group in the structure of medications such as MTM and PTU may be responsible for the stimulation of anti-neutrophil antibodies that mediate agranulocytosis. Antibody production is thought to result from the antioxidant effects of these compounds (9,10). Recent efforts have been directed towards the development of new antithyroid agents with a more favorable toxicity profile. A series of compounds have been synthesized using structure-activity relationships. The design of these compounds was based on atom level electrotopological state (E-state) indexes, a measure of atom electronic accessibility that is a useful tool in drug design of compounds with desired pharmacologic activity (11-13). E-state indexes of the thiourylene moiety have successfully been utilized to design antithyroid compounds with reduced antioxidant properties (14). One of these compounds is Abouthioline (1-Cyclohexyl-3(3-quinolyl)-2-thiourea, ABL, Figure 1). A series of investigations have been -3- published evaluating the antithyroid and antioxidant activities of ABL. Using the 125 I- thiocyanate discharge technique in rats, ABL demonstrated significantly greater antithyroid efficacy compared to PTU (15). Additional studies of the chemiluminescence response and phagocytic activity of polymorphonuclear lymphocytes demonstrated that ABL had reduced antioxidant and phagocytic activity compared to PTU and MTM (16). Thus, it appears that ABL may represent a useful antithyroid medication with a reduced risk of toxicity. In the present investigation, the preclinical toxicology of ABL was studied in mice and rats. The objective of these experiments was to compare the effects of ABL, PTU, MTM and thyroxine on biochemical and hematological parameters in these species. Methodology All animal experiments were conducted in accordance with the Institute for Laboratory Animal Research (ILAR) “Guide for Care and Use of Laboratory Animals” (17) Acute toxicity assessment in mice Equimolar doses of test and reference compounds were utilized: ABL (17mg/kg /day), PTU (10mg/kg/day), MTM (6.7 mg/kg/day) and thyroxine (77g/kg/day). The compounds were freshly dispersed in 1% tween-80 aqueous solution prior to oral dosing. Thirty male mice were divided into on of five study groups: control (n=10), ABL (n=5), PTU (n=5), MTM (n=5) and thyroxine (n=5). The control group received 0.1ml/10g/day of 0.1% Tween-80 aqueous vehicle. Each of the treatment groups were administered 0.1ml/10g/day of drug dispersion. Drug dosing (including control) was performed daily for seven days. At the end of the seventh day, blood samples were collected via the tail vein. Blood biochemical -4- parameters were measured using an AxSym Analyzer (Abbott Laboratories, North Chicago, IL). Parameters included the following: glucose, urea, creatinine, sodium, potassium, chloride, uric acid, calcium, inorganic phosphorous, magnesium, iron, total bilirubin, total protein, albumin, cholesterol, triglycerides, alkaline phosphatase, lactate dehydrogenase (LDH), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and creatine kinase. Long term toxicity in rats The dose of test (ABL) and reference compounds (PTU, MTM) was 20 mg/Kg/day. The compounds were freshly dispersed in 2% Cremophor EL/Saline solution prior to oral dosing. Twenty-five male Sprague-Dawley rats were divided into one of four study groups: control (n=10), ABL (n=5), PTU (n=5) and MTM (n=5). The control group received 0.1ml/10g/day of 0.1% Cremophor EL/Saline aqueous vehicle. Each of the treatment groups were administered 0.1ml/10g/day of drug dispersion. Drug dosing (including control) was performed daily for 30 days days. At the end of 30 days, blood samples were collected via the tail vein. Blood biochemical parameters were measured using an AxSym Analyzer (Abbot Laboratories, North Chicago, IL) as described previously. Hematological parameters were determined using a Cell-Dyne 1700 Analyzer (Abbott Laboratories). The hematologic profile consisted of a CBC (WBC, RBC, HgB, HCT, MCV, MCH, MCHC, RDW and PLT), a three-part WBC differential (lymphocyte, monocyte, granulocyte) and histograms of RBC, WBC and platelets. -5- Statistical Analysis The effects of ABL and reference compounds on biochemical and hematological parameters were analyzed by one-way analysis of variance. Dunnett’s test was utilized to identify significant differences between individual treatment groups and controls (p < 0.05). Results Acute Toxicity in Mice The results of acute toxicity studies in mice are presented in Table 1. Reported in the table are the biochemical parameters for control studies together with the compounds tested. Overall, there were few treatment effects on serum chemistry. Mice treated with thyroxine and ABL had a slightly higher sodium level, although this finding appears to be clinically insignificant. Additionally, both compounds significantly reduced uric acid. ABL administration was associated with significant reductions in total protein and albumin concentrations. Chronic Toxicity in Rats The effects of long term exposure (30 days) of ABL, PTU and MTM on serum biochemistry in rats are presented in Table 2. In contrast to the acute toxicity studies (Table 1), a number of effects were noted. Both PTU and ABL were associated with significant reductions in serum glucose. Each compound studied produced varying degrees of electrolyte imbalance (K, Cl, Mg). Total protein levels were significantly increased. PTU administration significantly increased creatinine, bilirubin, ALT and AST levels. -6- Table 3 provides contains a summary of hematologic findings. ABL administration was associate with changes in Hct, mean cell volume and mean cell width. No other changes in hematology were noted with ABL. PTU caused a significant reduction in total WBC count. Neutrophil concentrations were significantly reduced by both PTU (absolute value) and MTM (both absolute value and %total). Discussion ABL is a novel antithyroid compound specifically designed to reduce the incidence of severe hematologic toxicity that is associated with medications that are presently used in the treatment of Graves’ disease (PTU and MTM). pharmacologic activity of ABL (14,15). Previous studies have demonstrated the The goal of this investigation was to assess the tolerability of ABL as compared to PTU and MTM. Acute toxicity studies in mice established that ABL compared favorably with the reference compounds. Although serum protein and albumin levels were decreased by ABL, the reason for this effect is unclear. Reduced protein concentrations can sometimes be a manifestation of liver toxicity, although this seems unlikely given the short duration of the study and the fact that other indices of hepatobiliary function (e.g., ALT, AST, bilirubin, LDH) were unchanged. Furthermore, these changes did not occur following long-term administration to rats. ABL also appeared to perform well following chronic administration. Although the compound appeared to cause electrolye imbalance and hypoglycemia, similar observations were observed with PTU and MTM. The clinical significance of this observation is yet to be evaluated, although the magnitude of this imbalance is unlikely to be dose limiting. There was -7- evidence of drug-induced kidney and liver damage in rats treated with PTU. These findings were not observed with ABL and MTM. ABL did not appear to cause any disturbances in hematological values. There was no evidence associating ABL with the most severe side effect of present antithyroid therapy, agranulocytosis (characterized by neutropenia). Conversely, both MTM and PTU were associated with changes in WBC (PTU) and neutrophil concentrations (PTU and MTM). In summary, the results of this preclinical toxicity study indicated that ABL compared favorably with existing antithyroid medications. Serum chemistry data from mice and rats indicated similar effects of ABL, PTU and MTM on electrolyte and glucose levels. In contrast to the reference compounds, there were no detrimental effects of ABL on hematologic parameters (i.e., WBC and neutrophils). These results suggest that ABL is a promising new antithyroid therapy with a reduced risk of the blood dyscrasias (agranulocytosis and aplastic anemia) that have been reported with commonly prescribed medications. Additional studies are warranted to further investigate the safety and efficacy of this compound. -8- References 1. Chiovato L, Santini F, Pinchera A 1995 Treatment of hyperthyroidism. Thyroid Int. 2:1-22. 2. Roti E, Minelli R, Gardini E 1994 Controversies in the treatment of thyrotoxicosis. Adv. Endocrinol. Metab. 5:429-460. 3. Klein I, Becker DV, Levey GS 1994 Treatment of hyperthyroid disease. Ann Intern Med 121:281-288. 4. Bartalena L, Bogazzi F, Martino E 1996 Adverse effects of thyroid hormone preparations and antithyroid drugs. Drug Safety 15:53-63. 5. Tajiri J, Noguchi S, Murakami T, Murakam T 1990 Antithyroid drug–induced agranulocytosis: the usefulness of routine white blood cell count monitoring. Arch. Intern. Med. 150:621-624. 6. Tajiri J, Noguchi S, Okamura S, Morita M, Tamaru M, Murakami N, Niho Y 1993 Granulocyte colony-stimulating factor treatment of antithyroid drug-induced granulocytopenia. Arch. Intern. Med. 153:509-514. 7. Retsagi G, Kelly JP, Kaufman DW. 1988 Risk of agranulocytosis and aplastic anemia in relation to use of antithyroid drugs: international agranulocytosis and aplastic anemia study. BMJ 297:262-265. 8. Biswas N, Ahn Y, Goldman JM, Schwartz JM 1991 Case report: aplastic anemia associated with antithyroid drugs. Am. J. Med. Sci. 301:1353-1362. 9. Wall JR, Fang SL, Kurocki T, Lagbar SH , Braverman LE 1984 In vitro immunoactivity of propylthiouracil, methimazole and carbizole in patients with Graves’ disease: a possible cause of antithyroid drug-induced agranulocytosis. J. Clin. Endocrinol. Metab. 58:868-872. -9- 10. Wilson R, McKillop JH, Travers M, Smith J, Smith E, Thomson JA 1990 The effect of antithyroid drugs on intracellular mediators. Acta Endocrinol. Copenh. 122:605-609. 11. Hall LH, Mohney B, Kier LB 1991 The electrotopological state: an atom index for QSAR. Quant. Struct. Act. Relat. 10:43-52. 12. Kier LB, Hall LH 1992 An atom description in QSAR models: development and use of an atom level index. In: Testa B (ed) Advances in Drug Design, Academic Press Ltd, New York, pp. 1-38. 13. Hall LH, Kier LB 1992 Binding of salicylamides: QSAR analysis with electrotopological state indexes. Med. Chem. Res. 2:497-502. 14. Abou-Shaaban RRA, Al-Kahmees HA, Abou-Auda HS, Simonelli AP 1996 Atom level electrotopological-state indexes in QSAR: designing and testing antithyroid agents. Pharm. Res. 13:129-136. 15. Abou-Shaaban RRA, Al-Kahmees HA, Abou-Auda HS, Simonelli AP 1995 Development of new antithyroid compounds with reduced antioxidant property. Saudi Pharmaceutical Journal 3:180-195. 16. Abou-Shaaban RRA, Simonelli AP Antioxidative and proliferative activity of two newly synthesized antithyroid drugs, abouthiazine and abouthioline, as compared to propylthiouracil and methimazole. (submitted for publication?) 17. Institute for Laboratory Animal Research. National Research Council. Guide for the Care and Use of Laboratory Animals. Washington DC, National Academy Press, 1996. - 10 - Table 1. Serum Biochemistry Data Following Acute Exposure (7 days) in Micea Serum Parameters (SI units) Concentration of Parameters (Mean ± SD) Control PTU MTM Thyroxine ABL Glucose 8.84 7.4 9.28 7.54 8.96 (mmol/l) (± 2.10) (± 1.17) (± 0.89) (± (0.79) (± 0.94) Urea 10.1 10.52 8.90 9.56 9.60 (mmol/l) (± 1.47) (±1.61) (± 0.47) (± 0.58) (± 0.93) Creatinine 33.3 32.2 30.50 30.00 28.80 (micmol/l) (± 3.72) (± 3.31) (± 1.80) (± 3.41) (± 3.31) Sodium 151.8 153.6 153.00 154.60 154.40 (mmol/l) (± 2.36) (± 1.4) (± 0.71) (± 1.36)* (± 0.49)* Potassium 6.49 6.9 6.88 6.78 5.62 (mmol/l) (± 0.87) (± 0.43) (± 0.37) (± 0.26) (± 0.31) Chloride 88.0 74.0 82.00 83.20 96.00 (mmol/l) (± 18.7) (± 3.29) (± 2.24) (± 6.94) (± 4.05) Uric Acid 180.3 218.2 229.00 93.40 89.40 (micmol/l) (± 97) (± 73.9) (± 44.43) (± 6.62) (± 19.32) Calcium 2.58 2.52 2.48 2.56 2.48 (mmol/l) (± 0.10) (± 0.1) (± 0.04) (± 0.05) (± 0.04) Inorg. 3.35 3.44 3.33 3.72 3.28 Phosphorous (± 0.25) (± 0.54) (± 0.23) (±0.44) (± 0.28) (mmol/l) Mg 0.99 1.14 0.99 1.04 0.86 (mmol/l) (± 0.13) (± 0.22) (± 0.12) (± 0.20) (± 0.08) Fe 46.1 49.8 61.75 32.60 42.80 (mmol/l) (± 12.57) (± 8.61) (± 12.17) (± 7.47) (± 6.62) Total bilirubin 2.76 2.96 3.00 2.98 2.22 (micmol/l) (± 0.55) (± 0.3) (± 0.42) (± 0.31) (± 0.37) Total protein 51.7 52.0 52.75 50.80 44.80 (g/l) (± 1.9) (± 1.4) (± 1.48) (± 1.60) (± 1.72)* Albumin 28.1 26.6 29.00 26.40 25.20 (g/l) (± 1.45) (± 1.02) (± 0.00) (± 1.50) (± 0.98)* Cholesterol 2.99 2.96 2.83 2.28 2.52 (mmol/l) (± 0.37) (± 0.34) (± 0.18) (± 0.32)* (± 0.32) Triglycerides 1.60 1.60 1.48 1.30 1.52 (mmol/l) (± 0.28) (± 0.27) (± 0.11) (± 0.22) (± 0.27) Alk. Phosphatase 127.6 104.2 142.25 164.40 101.20 (U/l) (± 32.99) (± 21.7) (± 26.93) (± 38.24) (± 16.19) LDH 963 917 813.50 995.40 728.40 (U/l) (± 381) (± 141.2) (± 100.64) (± 76.75) (±75.76) ALT 41.9 51.8 48.00 99.00 51.00 (U/l) (± 7.2) (± 9.74) (± 9.03) (± 45.45)* (± 18.06) AST 199.4 278 192.50 284.20 181.80 (U/l) (± 68.7) (± 49.8) (± 29.92) (±68.76) (± 20.89) Creatine Kinase 253 244.4 248.75 329.40 179.40 (U/l) (± 127.4) (± 140) (± 42.16) (±71.06) (± 45.40) a data reported as Mean ( SD) for control (n = 10) and treatment groups (n = 5). The following daily doses were studied: PTU (10mg/kg/day) , MTM (6.7 mg/kg/day), thyroxine (77g/kg/day), ABL (17mg/kg /day). * denotes significant difference compared to control (p < 0.05) - 11 - Table 2. Serum Biochemistry Data Following Chronic Exposure (30 days) in Ratsa Serum Parameters (SI units) Glucose (mmol/l) Urea (mmol/l) Creatinine (micmol/l) Sodium (mmol/l) Potassium (mmol/l) Chloride (mmol/l) Uric Acid (micmol/l) Calcium (mmol/l) Phosphorous (mmol/l) Mg (mmol/l) Fe (mmol/l) Total bilirubin (micmol/l) Total protein (g/l) Albumin (g/l) Cholesterol (mmol/l) Triglycerides (mmol/l) Alk. Phosphatase (U/l) LDH (U/l) ALT (U/l) AST (U/l) Creatine Kinase (U/l) Concentration of Parameters (Mean ± SD) Control 5.44 (± 0.75) 5.90 (± 0.53) 55.20 (± 3.66) 144.60 (± 0.80) 5.16 (± 0.25) 98.00 (± 1.41) 56.60 (± 5.85) 2.55 (± 0.09) 2.50 (± 0.11) 1.09 (± 0.15) 37 (± 8.22) 2.16 (± 0.81) 68.4 (± 1.96) 31.2 (± 0.98) 1.36 (± 0.16) 0.64 (± 0.17) 150.2 (± 35.7) 636 (± 307) 45.6 (± 8) 126.2 (± 22.9) 516 (± 231.7) PTU 1.60 * (± 0.5) 11.2 * (± 1.2) 75.6 * (± 3) 143.2 (± 2.1) 3* (± 0.5) 103 * (± 1.9) 67.8 (± 30) 2.7 (± 0.11) 2.1 (± 0.34) 1.6 * (± 0.1) 27.6 (± 8.2) 4.1 * (± 0.4) 83.2 * (± 2.2) 31 (± 1.3) 2.2 * (± 0.38) 0.78 (± 0.1) 178.6 (± 30) 725 (± 559.8) 64 * (± 8.5) 171 * (± 31.7) 518.6 (± 249) - 12 - MTM 3.44 (±0.71) 5.56 * (± 1.50) 55.6 (± 1.74) 143.6 (± 0.49) 3.3 * (± 0.30) 98.2 (± 0.40) 53.2 (± 16.19) 2.72 (± 0.07) 2.36 (± 0.14) 1.6 * (± 0.06) 25 (± 5.76) 2.42 (± 0.53) 75.4 * (± 2.73) 32.2 (± 0.98) 2.44 * (± 0.54) 0.92 * (± 0.19) 158.6 (± 11.41) 353 (± 119) 38.20 (± 6.27) 96.6 (± 4.63) 648.2 (± 477) ABL 2.32 * (± 0.61) 7.14 (± 0.70) 54.80 (± 3.66) 144.20 (± 1.33) 2.54 * (± 0.53) 91.0 * (± 2.97) 78.40 (± 21.30) 2.90 * (± 0.06) 2.60 (± 0.18) 1.66 * (± 0.14) 24.60 (± 5.85) 2.38 (± 0.61) 76.20 * (± 1.72) 32.40 (± 0.80) 1.90 (± 0.17) 0.82 (± 0.17) 172.20 (± 23.40) 530.60 (± 143.23) 57.20 (± 8.75) 147.40 (± 9.16) 439.80 (± 57.31) a data reported as Mean ( SD) for control (n = 10) and treatment groups (n = 5). The dose of each test compound was 20 mg/Kg/day. * denotes significant difference compared to control (p < 0.05) - 13 - Table 3. Hematology Data Following Chronic Exposure (30 days) in Ratsa Blood Parameters (S.I. Units) Control Mean Parameter Values ( SD) PTU MTM ABL White blood counts 14.06 8.62 13.34 13.22 (x103 /l) ( 1.61) ( 1.70) ( 2.42) ( 2.50) Red blood counts 7.81 6.82* 7.22 7.36 (x 106 /l) ( 0.15) ( 0.52) ( 0.67) ( 0.54) Hemoglobin (Hg) 14.58 13.44 13.72 14.20 (g/dl) ( 0.32) ( 0.53) ( 0.92) ( 0.70) Hematocrite 45.78 43.68 44.22 53.12* (%) ( 1.09) ( 2.64) ( 3.08) ( 2.77) Mean cell volume 58.64 64.22 61.40 72.54* (fl.) ( 2.27) ( 3.98) (2.08) ( 6.46) Mean cell Hg 18.64 20.25 19.02 19.34 (pg.) ( 0.67) ( 0.30) ( 0.76) ( 0.66) Mean cell Hg conc. 31.80 30.80 30.98 26.84* (g/dl) ( 0.75) ( 1.04) ( 0.21) ( 2.01) Red cell distribution width 15.24 16.36 15.30 22.56* (%) ( 0.91) ( 1.26) ( 0.72) ( 2.14) Platelets 951.40 714.20* 669.20* 953.40 (x 103/l) ( 30.05) ( 121.9) ( 88.08) ( 261.29) Mean platelet volume 6.10 7.50* 7.12* 6.72 (fl) ( 0.26) (0.58) ( 0.47) ( 0.42) Neutrophils 28.20 21.00 5.60* 39.00 (%) ( 7.60) ( 12.99) ( 1.85) ( 15.13) Lymphocytes 67.40 77.40 92.40* 59.00 (%) ( 7.68) ( 12.29) ( 2.06) ( 15.17) Monocytes 1.80 1.00* 1.00* 0.60 (%) ( 1.17) ( 0.63) ( 0.63) ( 0.49) Eosinophils 2.60 0.60 1.00 1.40 (%) ( 1.02) ( 0.49) ( 0.89) ( 1.85) Basophils 0.00 0.00 0.00 0.00 (%) ( 0.00) ( 0.00) ( 0.00) ( 0.00) Neutrophils Absolute value 4.07 1.92 0.78* 5.01 3 (x10 / l) ( 1.41) ( 1.46) ( 0.34) ( 1.96) Lymphocyte Absolute value 9.36 6.57 12.30 7.98 (x103/ l) ( 0.54) ( 1.25) ( 2.13) ( 2.88) Monocytes Absolute value 0.27 0.08 0.13 0.09 3 (x10 / l) ( 0.18) ( 0.06) ( 0.10) ( 0.07) Eosinophils Absolute value 0.35 0.05* 0.13* 0.14 (x103/ l) ( 0.11) ( 0.04) ( 0.11) ( 0.16) Basophils Absolute value 0.00 0.00 0.00 0.00 (x103/ l) ( 0.00) ( 0.00) ( 0.00) ( 0.00) a data reported as Mean ( SD) for control (n = 10) and treatment groups (n = 5). The dose of each test compound was 20 mg/Kg/day. * denotes significant difference compared to control (p < 0.05) - 14 - Figure Legend Figure 1. Chemical structures of propylthiouracil, methimazole and abouthialine - 15 - H N S CH3 HN O Propylthiouracil (PTU) H3C N SH N Methimazole NH S HN N Abouthialine (1-Cyclohexyl-3(3-quinolyl)-2-thiourea) - 16 -