Depth of - 高雄榮民總醫院
advertisement

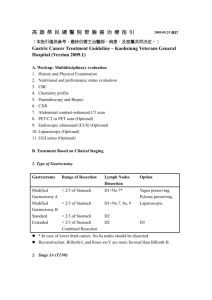
高 雄 榮 民 總 醫 院 胃 腺 癌 治 療 指 引 ﹝本指引僅供參考,最終仍需主治醫師、病患、及家屬共同決定。﹞ Gastric Cancer Treatment Guideline – Kaohsiung Veterans General Hospital (Version 2008.1) A. Workup: Multidisciplinary evaluation 1. History and Physical Examination 2. Nutritional and performance status evaluation 3. CBC 4. Chemistry profile 5. Panendoscopy and Biopsy 6. CXR 7. Abdominal contrast-enhanced CT scan 8. PET/CT or PET scan (Optional) 9. Endoscopic ultrasound (EUS) (Optional) 10. Laparoscopy (Optional) 11. UGI series (Optional) B. Treatment Based on Clinical Staging 1. Type of Gastrectomy Gastrectomy Range of Resection Lymph Nodes Dissection Option Modified < 2/3 of Stomach Gastrectomy A Modified < 2/3 of Stomach Gastrectomy B Standard > 2/3 of Stomach D1+No.7* Vagus preserving, Pylorus preserving, Laparoscopic Extended D2 > 2/3 of Stomach Combined Resection D1+No.7, 8a, 9 D2 D3 *:In case of lower third cancer, No.8a nodes should be dissected Reconstruction: Billroth-I, and Roux-en-Y are more favored than Billroth-II. 2. Stage IA (T1N0) Depth of invasion# Histology Size Treatment Mucosa(M) Differentiated (well <2 cm EMR*, ESDΦ, or MGΨA ≧2cm ESD, or MGA Any <1.5 cm ≧1.5cm MG A MG A MG B MG B & moderately) Mucosa(M) Differentiated (well & moderately) Mucosa(M) Submucosa (SM) Submucosa (SM) Submucosa (SM) Others Differentiated Differentiated Others Any * Endoscopic Mucosal Resection; Φ Endoscopic Submucosal Dissection Ψ Modified Gastrectomy # Depth of invasion determined by either endoscopic ultrasonography (EUS) or endoscopic findings (1. mucosal cancer: (i) small protruded cancer [type 0-I cancer], (ii) superficial elevated cancer [type 0-IIa cancer] or (iii) superficial depressed cancer with smooth surface [type 0-IIc cancer]; 2. cancer with submucosal invasion: (i) cancer with a rigid base, (ii) cancer with a nodular margin, (iii) cancer with interrupted or fused folds or (iv) excavated cancer [type 0-III early cancer]) 3. Stage IB (T1N1, T2N0) Depth of invasion Size Lymph Node Surgery T1 T1 T2 < 2cm > 2cm N1 N1 N0 MG B Standard Standard 4. Stage II (T1N2, T2N1, T3N0) Depth of invasion Lymph Node Surgery T1 T2 T3 N2 N1 N0 Standard Standard Standard 5. Stage IIIA (T2N2,T3N1,T4N0) Depth of invasion Lymph Node Surgery T2 N2 Standard T3 T4 N1 N0 Standard Extended 6. Stage IIIB (T3N2, T4N1) Depth of invasion Lymph Node Surgery T3 T4 N2 N1 Standard Extended 7. Stage IV (N3, M1) a. In patients with M1 lesion(s),but with good performance status (0-2): Chemotherapy, Radiotherapy, or Best supportive care b. In patients with urgent symptoms: bleeding, stenosis, malnutrition etc Palliative surgery (resection, by-pass, gastrostomy, or enterostomy) c. In patients with T1-3N3 or T4N2-3 lesions without M1: Extended radical gastrectomy C. Adjuvant or Neo-adjuvant Chemotherapy: 1. Indicated in Stage II (optional), IIIA, IIIB & IV 2. Regimen (admission usage) A. patient with performance status (ECOG) 0&1 and age ≦70 modified ECF regimen: 5FU 600mg/m2 Epirubicin 50mg/m2 Cisplatin 60mg/m2 Total 6 cycles IV D1 every 4 weeks IV D1 every 4 weeks IV D1 every 4 weeks B. patient with performance status (ECOG) 2 or age >70 . 5-FU 450mg/m2 Leucovorin 25mg/m2 Total 6 cycles IV Day 1-5 every 4 weeks IV Day 1-5 every 4 weeks 3. OPD usage Regimen C. patient with performance status (ECOG) 0&1 and age ≦70 5-FU 600mg/m2 weekly Leucovorin 25mg/m2 weekly For 6 months D. patient with performance status (ECOG) 2 or age >70 UFUR 第二線用藥 2# bid for 6 months (建議) 1. DCF (Docetaxel, cisplatin and 5-FU) Docetaxel 75mg/m2 iv D1 2 Cisplatin 75mg/m iv D1 5 FU 750mg/m2 iv D1-5 2. every 3 weeks every 3 weeks every 3 weeks Oxaliplatin + fluoropyrimidine (5-FU or capecitabine) D. Chemotherapy for Unresectable and Metastatic Cancer 如上 E. Intraperitoneal Hyperthermic Chemotherapy (continuous hyperthermic peritoneal perfusion: CHPP) 1. Indication: > T3 2. Regimen: Cisplatin 90 mg/3-4 liter(L) Lactated Ringer solution Etoposide 90 mg/3-4 L Lactated Ringer solution Mitomycin C 30 mg/3-4 L Lactated Ringer solution 41-42℃ for 20-60 minutes F. Radiation Adjuvant Chemoradiotherapy following Complete Surgical Resection 1. For R0 resection T4 2. For R1 resection and R2 resection (R0 = no cancer at resection margin, R1 = microscopic residual cancer, R2 = macroscopic residual cancer or M1B) Source: NCCN Practice Guideline in Oncology – Gastric Cancer v.2.2009 Chemoradiation Therapy as the Primary Treatment 1. Medically fit patients but unresectable cancer and no distant metastasis 2. Medically unfit patients, no distant metastasis Source: NCCN Practice Guideline in Oncology – Gastric Cancer v.2.2009 Protocol of adjuvant chemoradiotherapy 45 Gy (1.8 Gy/day) of RT given with 5-FU (400 mg/m2 per day) and leucovorin calcium (20 mg/m2 per day) on days 1 through 4 and the last three days of RT. Protocol of Chemoradiation therapy as the primary treatment 45 Gy (1.8 Gy/day) of RT given with 5-FU (400 mg/m2 per day) and leucovorin calcium (20 mg/m2 per day) on days 1 through 4 and the last three days of RT. 5.4 Gy (1.8 Gy/day) of reduced boost field to small areas of residual disease. Reference: 1. NCCN Practice Guideline in Oncology – Gastric Cancer v.2.2009 2. Macdonald JS; Smalley SR; Benedetti J; Hundahl SA; Estes NC; Stemmermann GN; Haller DG; Ajani JA; Gunderson LL; Jessup JM; Martenson JA: Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction [Intergroup trial 0016]. N Engl J Med 2001 Sep 6;345(10):725-30. G. Summary of Treatment Indication According to Clinical Staging N0 N1 N2 N3 T1 (M) IA EMR, ESD MG A IB MG B Standard II Standard T1 (SM) IA MG A IV Extended gastrectomy or Palliative gastrectomy MGB T2 IB Standard II Standard Adj. Chem IIIA Standard Adj. Chem or Chemotherapy or Radiation or Palliative II IIIA IIIB Standard CHPP (opt) Adj. Chem (opt) Standard CHPP (opt) Adj. Chem Standard CHPP (opt) Adj. Chem T4 IIIA Extended CHPP (opt) Adj. Chem Radiation(opt) IIIB Extended CHPP (opt) Adj. Chem Radiation(opt) M1 IV T3 care G. Follow-up 1. 0- 3 years after operation every 3 months: liver function test, CEA, & CA19.9 every 6 months: CXR, panendoscopy, CBC & abdominal sono/CT 2. 4,5 years after operation every 3 months: liver function test, CEA, & CA19.9 every 6 months: CXR, CBC & abdominal sono every year: panendoscopy, & abdominal CT 3. 5 years later every 6 months: liver function test, CEA, & CA19.9 every year: CXR, panendoscopy, CBC and abdominal sono/CT