Welcome
advertisement
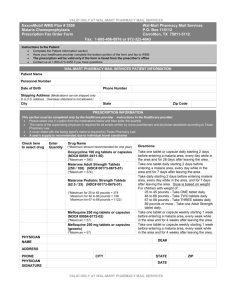
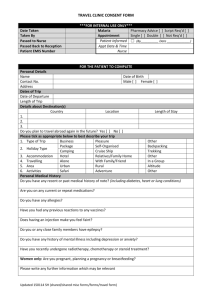
Malaria Malaria is one of the more common and serious of the tropical diseases causing 7-10 deaths from imported malaria in travellers every year. Infection is usually acquired by the bite of an infected mosquito, normally between dusk and dawn. It is important to remember that malarial illness may be delayed until up to a year after exposure. The shortest incubation period is 12 days; so short-term travellers are most likely to develop the disease after their return. The doctor should be made aware that you have been to a malarial area if you develop a flulike illness, so that malaria can be excluded. Symptoms Malaise, headache, fever, sweats, diarrhoea, vomiting, abdominal pain, joint pain, followed by anaemia and jaundice. Advice 1. Avoid contact with mosquitoes and bites. 2. Wear long sleeves and trousers in the evenings. 3. Wear insect repellents on the skin on top of sunscreen. 4. Avoid perfume, hairsprays and aftershave. Avoid dark clothing. 5. Sleep in a screened room or under impregnated nets. 6. Use knockdown sprays to kill mosquitoes in unscreened rooms. 7. Burn antimalarial coils at night. 8. Avoid mosquito breeding areas, e.g. stagnant water or rivers. 9. Consider using wrist or ankle bands impregnated with DEET. They usually last 100-120 hrs. Non-DEET repellents include Autan. Chemoprophylaxis No drug regime is 100% effective, and malaria may still develop when taking tablets. Approximately 25% of people taking antimalarial drugs experience side effects so it is important before taking any tablets to read the enclosed leaflet. All are on private prescription except Chloroquine and Proguanil, which may be bought directly from the chemist. Z Drive, Leaflets 2009, Travel 06/01/09 Mefloquine – 250mgs (one tablet) weekly. Start 2-3 weeks before entering malarial zone, continue during stay and for four weeks after. Although it is the preferred antimalarial for many parts of the world and is well tolerated by the majority of people, some do find it produces side effects such as sleep disturbance and nightmares, headaches, dizziness, and vomiting. It is not recommended for people with a history of psychiatric problems, depression, or epilepsy. Up to 25% of users develop some side effects, but severe reactions occur in 0.01% of users. If you experience any adverse side effects, seek medical help. If it is necessary to stop taking the drug, another will be prescribed. Doxycycline – 100mgs daily after food. Start 1-2 days before entering malarial zone, continue during stay and for four weeks after. This can cause skin photosensitivity in 3-10% of users. Diarrhoea and vomiting can also occur, so it is recommended to take the tablet with lots of water. Do not lie down immediately after taking. Proguanil - 200mgs daily and Chloroquine 300mgs two tablets. Start one week before entering malarial zone, continue during stay and for four weeks after. Can cause itchiness in dark skinned people. Other possible side effects are blurred vision, headaches, convulsions and gastrointestinal disturbances. Severe reactions occur in 0.01%. Malarone – 1 tablet daily (adults). Start 1-2 days before entering malarial zone, continue during stay and for one week after leaving. The tablet should be taken with food or a milky drink at the same time each day. It is usually well tolerated. Adverse reactions are similar in number to Mefloquine but more related to gastrointestinal disturbances. It may also cause rash, fever, headache, cough, insomnia, anaemia, stomach pain and upsets.