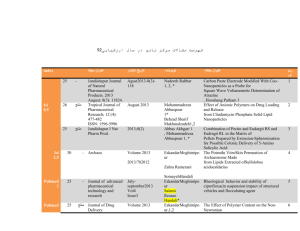
Reviews, Chapters, and Editorials
advertisement

Emad Eskandar, MD 1 Harvard CV PART 1: General Information Date Prepared: August 1, 2002 Name: Emad N. Eskandar, MD Office Address: Massachusetts General Hospital 15 Parkman St. ACC-021 Boston, MA 02114 617-724-6590 Home Address: Email: eeskandar@partners.org Fax: 617-724-0339 Education 1987 1993 B.A. M.D. University of Nebraska Lincoln University of Southern California Postdoctoral Training 1991 1994 1998 1999 Predoctoral Fellow Internship Postdoctoral Fellow Resident & Chief Resident Neuroscience Surgery Neuroscience Neurosurgery HHMI - National Institute of Mental Health Massachusetts General Hospital Harvard Medical School Massachusetts General Hospital Licensure and Certification 1999 Massachusetts Board of Medicine Academic Appointments 1999 1999 Instructor in Surgery Instructor in Neurobiology Harvard Medical School Harvard Medical School Hospital Appointments 1999 Assistant in Neurosurgery Massachusetts General Hospital Emad Eskandar, MD 2 Harvard CV Other Professional Positions and Major Visiting Appointments NA Hospital and Health Care Organization Service Responsibilities 1999 Attending Neurosurgeon Massachusetts General Hospital Major Administrative Responsibilities N/A Major Committee Assignments N/A Professional Societies American Association for Stereotactic and Functional Neurosurgery Congress of Neurologic Surgeons Community Service Related to Professional Work N/A Editorial Boards Ad Hoc Reviewer Journal of Neuroscience Awards and Honors 1987 1988 1989 1990 1992 1993 1996 1997 1998 2000 Phi Beta Kappa - University of Nebraska at Lincoln Medical Student Research Fellowship, University Southern California Research Scholar, Howard Hughes Medical Institute, N.I.H. Medical Student Fellowship, Howard Hughes Medical Institute Alpha Omega Alpha – University of Southern California Lange Medical Award – Top Student University of Southern California National Research Service Award, National Eye Institute R. S. Morrison Fellowship, Grass Foundation Resident Research Award - American Association Neurologic Surgeons Rappaport Fellowship - Massachusetts General Hospital PART II: Research, Teaching, and Clinical Contributions A. Narrative Report The goal of my work is to understand the functional circuitry involved in motor control in order to provide better treatments for movement disorders such as Parkinson’s Disease (PD). My research involves single and multi-neuron recordings in awake behaving primates and in humans undergoing surgery. The focus of my clinical work is functional neurosurgery which involves placing deep brain Emad Eskandar, MD 3 Harvard CV stimulating (DBS) electrodes to treat PD, tremor, and other disorders. In addition to research and clinical work, I teach students at Harvard Medical School and residents at the Massachusetts General Hospital. Over the previous 5 years, I have focused on the role of the posterior parietal cortex (PPC) in visually guided movements. We discovered that different areas within PPC are functionally segregated and that one area of PPC appears to convey unique, predictive information. Area MST conveys primarily visual information, area MIP conveys sensorimotor information, and area LIP appears to convey a predictive signal about moving or ambiguous stimuli. This work has been published in Nature neuroscience and Journal of Neurophysiology. My current research is aimed at understanding the interaction of two important pathways in the basal ganglia (direct and indirect) which are important in motor control. This work has been funded by a K08 (Mentored Clinical Scientist Development Award) and more recently a grant from the Harvard Center for Neurodegeneration and Repair. Preliminary data suggests that the two pathways function in a center-surround organization similar to that seen in the visual system. A better understanding of the interaction between the pathways will hopefully lead to better treatments for PD. I am currently in the process of setting up my own laboratory at MGH. The lab will include two rigs for awake monkey recordings and one rig for anesthetized preparations. The lab will be part of a larger group , including Jeff Mackliss and Dick Masland. One of the goals of this group will be to explore restorative therapies such as the use of deep brain stimulation and transplantation to treat neurologic disorders due to trauma, stroke, and degenerative disease. Clinically, I have been involved in creating an active program in deep brain stimulation at MGH. In addition, I have an approved protocol to study the physiologic properties of basal ganglia neurons in patients undergoing surgery and have built an intra-operative rig which allows for neuronal recordings while patients are performing reproducible visually guided movements. High quality data of this sort has never been obtained in humans and preliminary data already suggest several novel observations regarding the function of the basal ganglia in patients with PD. Some of this work has been published in JAMA and the Journal of Neurosurgery. I have been teaching the basal ganglia and spinal cord lectures in the HST neurobiology course since 1997. More recently, I have initiated a multi-media lecture that utilizes videotape of patients with movement disorders, surgical therapies of PD, and a computerized demonstration of intraoperative recordings to consolidate the basal ganglia information. In addition I have an active role in teaching neurosurgical residents during cases and in 2-4 formal lectures per year. Emad Eskandar, MD 4 Harvard CV B. Funding Information Years Covered Funding 1996-1998 2000-2003 2002-2004 PI/Co-PI NRSA - NEI Eskandar K08- NINDS Eskandar HCNR – HMS Eskandar Grant Title Extraretinal Signal in Parietal Cortex Neostriatal Visual Processing in Movement Initiation Basal Ganglia in Movement Control C. Report of Current Research Activities Project Role Neostriatal visual processing in movement initiation Basal ganglia in movement control Basal ganglia function in human PD patients Transplantation of embryonic cells in MPTP treated monkeys Clinical outcome of DBS in patients with PD Principal Investigator Principal Investigator Principal Investigator Collaborator with Ole Isacson Collaborator with Neurology Group D. Report of Teaching 1. Local Contributions a. Medical School Courses Taught Section Class Role 1996-1998 HST II Neurobiology Neuroanatomy Teaching Asst. 8 HST Students 30 hours/Year 1997-2001 HST II Neurobiology Basal Ganglia Lecturer 60 HST Students 10 hours /Year 1999-2001 HST II Neurobiology Movement Disorders Lecturer 60 HST Students 10 hours /Year 1997-2001 HST II Neurobiology Spinal Cord Lecturer 60 HST Students 10 hours /Year Lecturer 120 HMS Students 20 hours/Year 2000 - 2002 HMS II Neurobiology Basal Ganglia b. Graduate Medical Courses # Students Contact Hours 1999-2002 Attending Neurosurgeon Neurosurgery 1999-2002 Lecturer Basal Ganglia Residents and 4th year students 20 hrs / year Residents and 4th year students 8 hrs / week c. Local Invited Presentations for CME Credit 2000 Neurology Grand Rounds, MGH Management of Closed Head Injury Staff and Residents Emad Eskandar, MD 5 2000 2000 2001 2001 2002 Surgical Treatment of PD Parietal Cortex in Guidance The STN in the treatment of PD Surgical Treatment of PD Surgical Treatment of PD Neurology Grand Rounds, MGH Neurosurgery Grand Rounds, BWH Neurosurgery Grand Rounds, MGH Neurology Grand Rounds, Beverly Medicine Grand Rounds, South Shore Harvard CV Staff and Residents Staff and Residents Staff and Residents Staff Staff d. CME Courses 2001 Neuromodulation Symposium Cleveland Clinic Surgery for Psychiatric Disorders e. Advisory and Supervisory Positions 1999-2002 Attending Neurosurgeon Supervision of Neurosurgical Residents 2001-2002 Lab Preceptor 2 Residents on Research Rotations 6 Weeks / year 6 months / year f. Teaching leadership role N/A g. Names of Advisees or trainees Duration Name 6 months Ziv Williams, MD 6 months Ekkehardt, Kaspar, MD Position Neurosurgical Resident Neurosurgical Resident 2. Regional, National, or International Contributions 1999 Neurosurgery Grand Rounds 2000 Neurobiology Seminar 2000 Neurology Grand Rounds 2000 CVS Symposium 3. Description of teaching awards UCSF U. Chicago Cleveland Clin U. Rochester Role of Parietal Cortex in Visual Guidance Role of Parietal Cortex in Visual Guidance Surgical Treatment of Parkinson’s Disease Role of Parietal Cortex in Visual Guidance N/A 4. Description of major curriculum offerings I have been involved, in conjunction with John Assad, with developing the motor systems portion of the HST II neurobiology course. We have been jointly giving this course since 1997. In addition to giving the spinal cord and basal ganglia lectures, I have developed a lecture about movement disorders and their surgical therapy. This lecture involves videotape presentations of different types of movement disorders, operative procedures, and more recently demonstrations of intra-operative physiology, all of which help bring the material to life and are generally quite well received by the students. E. Report of Clinical Activities 1. My clinical practice is in functional neurosurgery and is aimed at treating patients with Parkinson’s disease, tremor, intractable pain, and epilepsy among others. I also have interest in the treatment of brain tumors, trigeminal neuralgia, and some spinal disorders. My sole practice is in the Department of Neurosurgery at the Massachusetts General Hospital. 2. I see about 20 patients per week on my office day and I operate one day per week. The complexity of the cases varies but includes highly complex deep brain stimulation cases and complex spine cases with multi-level instrumentation. The remainder of my time is generally spent in the laboratory. Emad Eskandar, MD 6 Harvard CV 3. My major contribution has been to bring the promising new technology of deep brain stimulation and high quality intra-operative microelectrode recordings to MGH. We have now performed about 30 operations with excellent results and the practice is growing. These operations involve stereotactic localization of the target area, intra-operative multi-electrode recordings, and implantation of the electrodes. An important aspect of these cases is that they provide the unique opportunity to record neuronal activity in the context of a controlled experimental paradigm. These data will yield important insights into the underlying pathophysiology. More recently, I have begun collaborations with the MGH psychiatry service to place DBS electrodes in the cingulate gyrus for the treatment of intractable obsessive compulsive disorder and with the MGH Anesthesia service to place thalamic stimulators for the treatment of intractable pain. In both cases we will have protocols to explore the underlying physiology. Emad Eskandar, MD 7 Harvard CV PART III. Bibliography Original Articles 1. Eskandar, EN, Richmond, BJ, Optican, LM. Role of Inferior Temporal Neurons in Visual Memory: I. Temporal Encoding of Information about Visual Images, Recalled Images, and Behavioral Context. J. Neurophysiol 1992; 68(4):1277-95. 2. Eskandar EN, Optican, LM, Richmond, BJ. Role of Inferior Temporal Neurons in Visual Memory: II. Multiplying Temporal Waveforms Related to Vision and Memory. J. Neurophysiol., 1992; 68(4):1296-1306. 3. Hertz, JA, Kjaer, TW, Eskandar, EN, Richmond, BJ. Measuring Natural Neural Processing with Artificial Neural Networks. International Journal of Neural Systems. 3. Suppl. 1992: 91-103. 4. Eskandar, EN, Weller, SA, Frim, DA. Hydrocephalus Requiring Urgent External Ventricular Drainage in a Patient with Diabetic Ketoacidosis and Cerebral Edema. Neurosurgery 1997;40(4):836-8. 5. Eskandar, EN, Cosgrove GR, Shinobu, LA, Penney JB. The Importance of Accurate Lesion placement in Pallidotomy. J. Neurosurgery 1998;89(4):630-4,. 6. Eskandar, EN Assad, JA. Dissociation of Visual, Motor, and Predictive Signals in Parietal Cortex During Visual Guidance. Nature neuroscience 1999;2(1):88 – 93. 7. Eskandar EN, Shinobu, LA, Penney JB, Cosgrove GR. Nonmicroelectrode-guided pallidotomy: Surgical Technique and 2 year results. J. Neurosurgery 2000;92:375-383. 8. Counihan TJ, Shinobu LA, Eskandar EN, Cosgrove GR, Penney Jr JB Jr. Outcomes following staged bilateral pallidotomy in advanced Parkinson's disease. Neurology 2001;56(6):799-802. 9. Eskandar, EN, Borges, LF, Putman, C, Budzik C, Ogilvy, CS. Spinal Dural Arteriovenous Fistulae: Experience with Endovascular and Microsurgical Therapy. J Neurosurg 2002;96(2):1204-10. 10. Eskandar, EN, Assad. JA. Representations of direction during visual guidance in the primate parietal cortex. J Neurophysiology 88: 2002. Emad Eskandar, MD 8 Harvard CV Proceedings of Meetings Eskandar EN, Richmond BJ, Hertz, JA, Optican LM, and Kjaer T. Decoding of Neuronal Signals in Visual Pattern Recognition. Advances in Neural Information Processing Systems IV. San Mateo, CA, Morgan and Kaufman; 1992. P. 356-363. Eskandar E, Shinobu LA, Penney JB Jr, Cosgrove GR. Non-microelectrode guided stereotactic pallidotomy for Parkinson's disease: surgical technique and results. Stereotact Funct Neurosurg. 1999;72(2-4):245. Reviews, Chapters, and Editorials Reviews Eskandar EN, Cosgrove RC, Shinobu, LA. Surgical treatment of Parkinson Disease. JAMA 2001, 286(24):3056-9. Book Chapters Cosgrove GR, Eskandar EN. Thalamotomy and Pallidotomy. In: Kaye AH, Black PM, editors. Operative Neurosurgery; 2000. London: Harcourt Publishers; P. 1431-1445 Eskandar EN, Cosgrove GR. Neurosurgical Treatment of Pain.. In: Ballantyne, J Fishman A, and Abdi S, editors. The Massachusetts General Hospital Handbook of Pain Management. Philadelphi: Lippincot Williams and Wilkins; 2002. P. 215-223 Eskandar EN, Cosgrove GR. Intractable Tremor: Thalamotomy or Thalamic Stimulation. In: Eric Schulder E, editor. Handbook of Functional Neurosurgery; In Press - 2002. Abstracts of Unpublished Work Eskandar EN, Shinobu LA, Penney JB, Cosgrove GR. Stereotactic Pallidotomy for Parkinson’s Disease: Long-term results. Congress of Neurologic Surgeons. 1999. Williams, Z, Eskandar, E, Elfar J, Assad, J. Neuronal Correlates of Subjective Visual Perception. Congress of Neurologic Surgeons, 2001. Eskandar, E, Williams, Z, Shinobu L, Cosgorve, G. Simultaenous mutli-electrode recordings in the subthalamic nucleus. American Association of Neurologic Surgeons, 2002. Curry, WT, Hoh, BL, Amin-Hanjani, S, Eskandar EN. Spinal Epidural Abscess: Clinical presentation, management, and outcome. American Association of Neurologic Surgeons, 2002.