Rheumatoid Arthritis
advertisement
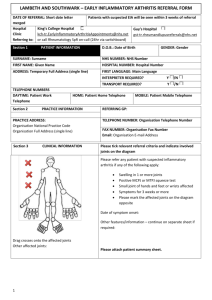
RHEUMATOID ARTHRITIS Dr. Vivek Rajagopal MD, MRCP Consultant Rheumatologist West Suffolk Hospital, Bury St Edmunds, UK Introduction: Rheumatoid Arthritis (RA) is a chronic inflammatory disease that manifests with persistent arthritis affecting the small joints of the hands and feet. As RA progresses, any system of the body may be affected, and can lead to premature death. Incidence/ Prevalence RA is a common condition with a prevalence of 1%. This can vary between 0.5% to 1.2% in various parts of the world. The incidence increases with age with a peak onset in the 4 th and 5th decades. RA is 2 to 4 times more common in women. Approximately 1/3 of people stop work within 2 years of onset of RA. RA is associated with an increased risk of cardiovascular disease similar to that of diabetes. This is thought to be multifactorial and is not fully explained by traditional cardiovascular risk factors. Clinical Features Synovitis – is the main clinical feature of RA. Synovitis is identified by the presence of pain, soft or boggy joint swelling and limitation of movement of the involved joint. In RA, Synovitis is persistent and tends to affect the small joints of the hands and feet. It is symmetrical (i.e. affects the same joints on both sides of the body, the degree of swelling may differ). Any synovial joint can be affected in RA – the exception is the distal interphalangeal joints. The spine is usually spared. The important exception is atlanto- axial joint involvement – this can be affected in up to 50% in patients with RA at some point and can cause subluxation and myelopathy. Onset – is usually gradual and additive i.e. a few joints- usually the hands or feet are initially involved with further joints being affected over the next few months. Sometimes the onset can be (i) Acute with multiple, severe crippling joint involvement over a few days. This is a marker of severity. (II) Palindromic- intermittent involvement of one or two joints that resolve within 24 to 48 hours and then returns in another joint area. (iii) Polymyalgic – can mimic polymyalgia rheumatica with predominant shoulder involvement. Other joints get affected over time. This pattern is seen mainly in patients over 60 years. Other Clinical Features Patients often suffer from fatigue or depression. A small proportion can have systemic features such as low grade fever, anorexia and weight loss. Sometimes extra articular features such as vasculitis, generalised lymphadenopathy or serositis may be the presenting feature. Carpal Tunnel Syndrome – is an early sign of wrist involvement. Differential diagnosis Any other condition causing synovitis needs to be considered before making a diagnosis of RA. (i) Viral Arthritis – present as a symmetrical polyarthritis, preceded by fever. Usually resolves within 6 weeks. (ii) Septic Arthritis – presents as a red, swollen monoarthritis, usually accompanied by constitutional symptoms. This is an important differential diagnosis in patients with established RA who present with a monoarticular flare. (iii) Polyarticular Gout – can mimic RA. Differentiating features are either long history of episodic monoarthritis, family history of gout or presence of tophi. (iv) Seronegative spondyloarthritis – These are asymmetric oligoarthritis with spinal involvement. Some patients may have peripheral arthritis alone, but may have a history of IBD or Psoriasis. Differentiation can be difficult at times. (v) Paraneoplastic arthritis – suspect if arthritis has not responded to first line medication or if patients have other localising symptoms such as chronic cough or altered bowel habit. Investigations If RA is suspected clinically, no investigations are necessary in primary care and patients should be referred for specialist assessment to avoid delay. The following tests are done by Rheumatologists to aid diagnosis and for baseline measure prior to starting treatment. Full blood count, CRP, ESR Urea and electrolytes, bone profile and liver function tests Rheumatoid factor and Anti CCP antibodies Radiography of hands and feet, chest( to exclude lung involvement) Ultrasound or MRI of hands and feet – if there is diagnostic uncertainty. When to refer Refer people with persistent synovitis without a known cause to a rheumatologist. Urgent referral is indicated if there are any of the following a. A delay of 3 months or longer between onset of symptoms and seeking medical advice. b. Small joints of hands and feet are affected ( Best screening test is metatarsal or metacarpal squeeze) c. More than one joint is affected Manage symptoms with Paracetamol, Codeine or NSAIDS till the patient is seen. Do not prescribe corticosteroids before specialist review as this can alter the clinical picture and delay diagnosis. Treatment RA needs to be managed in partnership with a specialised unit. Early referral makes a big difference in outcome as early use of disease modifying therapy has been shown to limit disabilities and deformities. Generally, patients are treated with Methotrexate, Hydroxychloroquine or Sulphasalazine either in combination or as monotherapy. Leflunomide is used in patients intolerant of Methotrexate. Anti TNF agents are used in patients who are either unresponsive or intolerant to first line disease modifying agents. However, DMARD treatment is constantly evolving and anti TNF medications are starting to be used at diagnosis in selected patients. Newer biologic agents are being trialled with a significant number likely to come into clinical use. Primary care physicians have an essential role in the following areas (i) Identifying and managing flares – the best way to manage a generalised flare is to treat with either intramuscular steroids (Triamcinolone 80mg or Methyl prednisolone 120mg) and arrange a specialist review. If one or two joints are affected, intra articular steroid if expertise is available. Short reducing courses of oral steroids can be used if injectable steroids are ineffective or not preferred by patients. (ii) Identify and manage any co morbidities related to RA or drug treatment. (iii) Cardiovascular risk assessment and treatment – RA is associated with excess cardiovascular risk similar to patients with diabetes. (iv) Offer pneumococcal and yearly influenza vaccine in patients on disease modifying agents. (v) Smoking cessation advice and treatment. Prognosis Advances in treatment have dramatically altered the long-term outlook for patients with RA. Drug induced remission has become a feasible goal of treatment. Early diagnosis and treatment with disease modifying therapies have reduced the need for orthopaedic interventions, maintained functional ability and kept more people in employment thus reducing the burden of disease in the community. Rheumatoid arthritis is associated with a 5 to 10 year reduction in lifespan mainly due to premature cardiovascular disease and GI bleeding due to peptic ulcer disease. NSAIDS are used less frequently and in short courses currently and this has reduced the incidence of GI bleeds in patients with RA. Changing paradigms of treatment with earlier use of biologics are likely to improve the prognosis further. However, a significant number of patients have disease which is refractory to current therapies and continue to experience significant disability.