Airway Management - University of Manitoba
advertisement

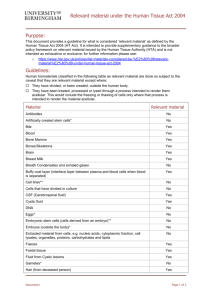
DEPARTMENT OF ANESTHESIA UNIVERSITY OF MANITOBA Fluid Therapy Training Module for Para Professional Personnel Preamble The Department of Anesthesia at the University of Manitoba is committed to the promotion of patient safety and quality of care. Education of providers of primary and resuscitation support from all disciplines is a fundamental part of that mission. For this educational effort to be effective, it is important to consider and incorporate the particular needs of each group for whom skills development is contemplated. This document outlines the structure, and goals and objectives of a program designed to meet the developmental needs of paramedical personnel providing care for patients with respect to fluid management in resuscitation. Program Outline Each trainee will be provided with a program outline, including a reference manual, orientation and contact information, and evaluation logs. At the end of the rotation, the trainee will be expected to keep evaluation logs and provide them to the Coordinator of the sponsoring program as proof of completion of the educational program. The trainee will present to the assigned hospital OR suite on the first day of the rotation, at the time and place indicated in the orientation manual. The senior resident or site coordinator will direct the trainee to a primary staff person. This primary staffperson shall Review the educational material with the trainee Provide resource discussion Evaluate the degree to which the trainee has met the knowledge objectives Record the results of that evaluation on the evaluation log Coordinate access to vascular access techniques with him/herself, and other staff as available Each individual staff physician or resident who supervises vascular access techniques will Observe the trainee and provide formative feedback Evaluate the trainee’s competence with the technique Record the evaluation on the provided log As applicable review and evaluate elements of the curriculum as discussed with the primary mentor Goals and Objectives By the end of this rotation, the trainee will be able to: Describe the indications for, contraindications to and complications of o Blood product therapy o Colloid therapy o Crystalloid therapy Describe the differences between colloid, crystalloid and blood component therapy Select and perform appropriate vascular access for patients requiring stabilization Recognize complications of vascular access techniques Assess fluid status and quantify need for fluid administration Evaluation Log for Paramedical Fluid Therapy Training Module Major Omissions Minor Omissions No Omissions Complete Discussion Outstanding o Normal saline o Non-blood colloid o Matched Red Cells o Emergency red cells o Central venous access Correctly assesses fluid status Correctly quantifies need for fluid therapy Describes the appropriate technique for central venous access Performs peripheral venous access Identifies complications of central or peripheral venous access Describe the correct interpretation of information from a pulse oximeter, including sources of error Major Errors Minor Errors Competent technique Efficient technique Outstanding Cognitive Objectives Describes the indications for, contraindications to and complications of o Technical Skills Objectives IV #1 IV #2 IV #3 IV #4 IV #5 IV #6 IV #7 IV #8 IV #9 IV #10 BLOOD AND FLUID COMPONENT THERAPY Stephen Kowalski, MD, FRCPC Rob Brown, MD, FRCPC Rational fluid therapy is dependent upon an appropriate understanding of the normal physiology of body fluids. Essentially, the body is divided into two major fluid components: 1) Intracellular fluid, and 2) Extracellular fluid. Although these compartments are separated by membranes of varying types, water, oxygen, electrolytes and nutrients cross these membrane barriers according to electrical, osmotic or chemical gradients. In order to preserve cell viability, each compartment maintains a fluid environment that allows cellular function to occur efficiently. Water accounts for 45 to 50 percent of the body weight of adult females and 55 to 60 percent of the body weight in adult males. The lower water content in females is due to their increased percentage of adipose tissue, which contains less water than muscle. Water content decreases with age. Newborn infants have 75 to 85% of their body weight as water. This decreases to 65% by age 1 and continues to decrease gradually after adolescence. Total body water is distributed between two major fluid compartments: 1) The extracellular fluid includes both the interstitial and the circulating blood volume, which accounts for 20% of body weight while, 2) The intracellular fluid accounts for 40% of the body weight. (Table 1) TABLE 1 WATER DISTRIBUTION (70 KG MALE) WATER COMPARTMENT %BODY WEIGHT Extracellular: 20% - Blood Volume 6% - Interstitial Fluid 14% Intracellular: h TOTAL VOLUME 14.0 L 4.2 L 9.8 L 40% 28.0 L 60% 42.0 L The movement of water between different fluid compartments is determined by two forces: 1) hydrostatic pressure, and 2) osmotic pressure. Water moves from a compartment with a high hydrostatic pressure to a compartment with a low hydrostatic pressure. However, osmotic forces are the prime determinant of water distribution in the body. The osmotic pressure of a solution or compartment is proportional to the "number of molecules" in a solution. Since water can freely cross all cell membranes, the body fluids are in osmotic equilibrium as the osmolalities of the intracellular and extracellular fluids are the same. Consequently, both the actual volume and the distribution of the body water between the cells and the extracellular fluid is determined by the number of osmotically active particles in each compartment. Sodium (Na+) is the principle electrolyte that acts to hold water in the extracellular space. Potassium (K+) performs a similar function in the intracellular compartment. Although the cell membrane is permeable to both Na+ and K+ these ions are able to be effective because they are restricted to their respective fluid compartments by the Na+/K+ pump in the cell membrane. In contrast, larger molecules such as plasma proteins do not cross cell membranes easily and are "confined" to the circulating blood volume. Therefore plasma proteins although they constitute only a small fraction of the total number of dissolved particles in the plasma, represent a major osmotic force preventing excessive fluid loss from capillaries. This effect of the plasma proteins (particularly albumin) is called the oncotic pressure. During a normal day, water intake equals water output. Most of water output involves "obligatory" losses from three sources (Table 2): 1) the skin and respiratory tract, 2) urine, and 3) stool. "Insensible" water loss by vaporization from the skin and lungs is approximately 12-15 ml/kg or about 900 ml per day in a 70 kg man. Insensible losses can be increased 10% per degree C rise in body temperature, by ventilation with dry anesthetic gases and active sweating. Urinary losses average 1 ml/kg/hr or 1600 ml in a 70 kg male while fecal loss is less than 100 ml/24 hour period (Table 2). The replacement of these water losses can be termed "maintenance" fluids. TABLE 2 1) WATER LOSS PER DAY (70 KG MALE) INSENSIBLE a) Perspiration 600 ml b) Lungs 400 ml 2. URINE 1,500 ml 3. FECES 100 ml TOTAL 2,600 ml Under normal circumstances, daily water losses are not associated with loss of electrolytes. However, gastric suction, vomiting, bowel obstruction, and diarrhea may be associated with significant electrolyte losses, which must be replaced in addition to water replacement. Typical electrolyte contents of various body fluids are included in Table 3. Therefore, replacement fluids should be selected on the basis of quantitative water loss and qualitative electrolyte loss. TABLE 3 FLUID Gastric Juice Bile Pancreatic Juice Ileal Fluid Cecal Fluid Na+(mEq/L) 60 149 141 129 80 K+(mEg/L) 9 5 5 11 21 Cl-(mEq/L) 84 101 77 116 48 HCO3-(mEq/L) 0 45 92 29 22 Several prepared solutions are outlined in Table 4. In the operating room, fluid replacement is directed at replacing: 1) maintenance fluid requirements, 2) third space losses (edema, exudates, transudates, ascites), and 3) blood. After replacing the pure water loss that has occurred when the patient is fasting before surgery, a balanced electrolyte solution (5% D N/S; Ringer's Lactate; 5% D, 1/2 N/S) should be used to replace both maintenance fluid requirements and third space losses. Approximate fluid volume can be administered according to the following guidelines: 4 ml/kg/hr Baseline Maintenance Requirements. 6 ml/kg/hr Minimal Surgery (ex. squint repair). 8 ml/kg/hr Moderate Surgery (ex. hernias). 10-12 ml/kg/hr Extensive Surgery (ex. thoracotomy, bowel obstruction). The final category of fluid management during surgery is the replacement of blood and blood products. Blood has several important components: 1. Volume is necessary to maintain blood pressure and to provide adequate tissue perfusion to all organs. Approximations of circulating blood volumes are: Newborn 85 ml/kg; Adult Male 65 ml/kg; and Adult Female 60 ml/kg. 2. Hemoglobin which is vital for the transport of oxygen. 3. Platelets and coagulation proteins which are necessary for hemostatis. 4. Plasma proteins which supply the oncotic pressure for proper water balance between the extracellular and intracellular fluid compartment. The following is a summary of some of the blood products that are currently available. It should be remembered that almost all blood products are stored at 4oC and should be warmed and filtered before administration to patients. Na+ K+ ClCa++ Lactate PH Dextrose Calories/L Osmol RINGER’S LACTATE 130 4 109 3 28 6.5 272 TABLE 4 NORMAL SALINE 154 154 5.5 308 5% D1/2 N/S 77 77 4.0 5.0 g/100 ml 200/L 406 1/3D, 2/3, N/S 3.3 g/100 ml 132/L 269 Packed Red Blood Cells The volume of packed red blood cells is approximately 250-300 ml/unit. Since the hematocrit is 55%, packed cells are very viscous which makes them difficult to transfuse rapidly. This property makes packed cells more effective in treating chronic anemias than rapid blood loss. In emergencies, the viscosity may be reduced which will allow for more rapid administration by adding either 200 ml of normal saline or one unit of fresh frozen plasma. In order to raise the hemoglobin 1 gram (or 10 gm/dl), 3 ml/kg of packed cells or 6 ml/kg of "reconstituted" packed cells may be transfused. Packed cells may transmit hepatitis but do not contain platelets, coagulation proteins or albumin. Fresh frozen plasma/stored plasma. The volume of frozen plasma is approximately 200 ml/unit. Plasma contains both coagulation factors and plasma proteins. Fresh frozen plasma contains the labile clotting factors (Factors V and VIII) while stored plasma contains reduced amounts of these clotting factors. Most plasma used in operating rooms is stored plasma. Plasma is labelled for ABO but not usually for RH group. Plasma must be compatible with the recipient's blood but it is not necessarily group specific. (see Table 5) TABLE 5 BLOOD GROUPS OF PLASMA THAT MAY BE INFUSED INTO RECIPIENTS RECIPIENTS BLOOD GROUP DONOR BLOOD GROUP 0 0, A, B, AB A A, AB B B, AB AB AB Stored plasma is effective in treating patients requiring volume expansion and protein replacement while fresh frozen plasma should be administered to patients with coagulation abnormalities. Plasma does not contain platelets and may transmit hepatitis and other viruses (HIV). Platelets The volume of platelet concentrates is approximately 50 ml/unit. Unlike plasma and packed red blood cells, platelets cannot be stored for long periods of time and must be administered within 72 hours of collection. They are stored at 22oC with continuous gentle agitation. Each unit contains 60% of the functional platelets found in a unit of fresh whole blood. Platelet concentrates are reserved for the treatment of thrombocytopenia and serum levels of 50,000 mm3 should be present to prevent bleeding during major surgery. Six units of platelets will raise the platelet count by 30,000 in a 70 kg male. Platelet concentrates may transmit hepatitis and other viruses. Cryoprecipitate The volume in cryoprecipitate is 5-15 ml/unit. Cryoprecipitate is essentially a concentrate of factor VIII and is effective in treating hemophilia. The administration of 1 unit/6 kg body weight will raise the factor VIII level 15-20%. It is usually administered every 8 hours due to the 1/2 life of factor VIII. Cryoprecipitate can transmit hepatitis and other viruses. Albumin Albumin is available in concentrations of 5% and 25%. The 5% solution is supplied in 50 ml, 250 ml, and 500 ml volumes and is osmotically equivalent to an equal volume of normal plasma. The 25% solution is available in volumes of 20 ml, 50 ml, and 100 ml and is osmotically equivalent to five times its volume of plasma. Albumin is used as a volume expander or to replace protein loss as occurs with an extensive burn or ascites. Albumin is pasteurized and does not transmit hepatitis or HIV. Pentastarch Pentastarch is a synthetic solution. It is a hydroxyethyl starch derived from cornstarch which is prepared commercially as a 10% solution dissolved in normal saline. Pentastarch is a large molecule (average molecular weight 200,000 to 300,000) and was developed as a substitute for albumin. It is supplied as a 250 ml and 500 ml bags for intravenous infusion. It is slightly more osmotically active than an equivalent volume of 5% albumin. Pentastarch does not cause coagulation abnormalities that are seen with other synthetic plasma volume expanders such as hetastarch and dextran. In summary, the goal of fluid therapy during surgery is to maintain homeostasis. Since the patients are unconscious, the Anesthesiologist must replace both maintenance water and electrolyte losses. Third space and blood losses represent additional fluid replacement that must be individualized. This chapter has suggested "guidelines" for optimal fluid replacement during surgery. However, the absolute amount and type of solution used during surgery must be modified by clinical examination of the patient. Therefore the ultimate goal of fluid therapy is not to comply with the guidelines of fluid administration, but to preserve cardiovascular stability, adequate perfusion and urine output. Fluid therapy must be individualized for each patient, with consideration of the functional status of most organ systems and based on accepted principles of basic science and physiology.