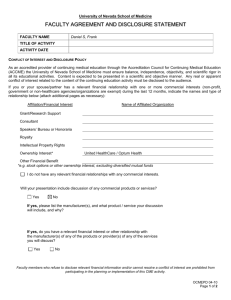
CME Faculty Financial Disclosure
advertisement

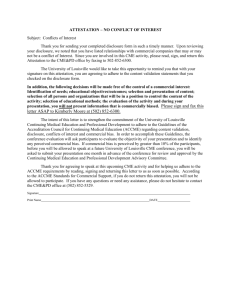
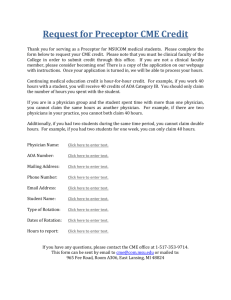
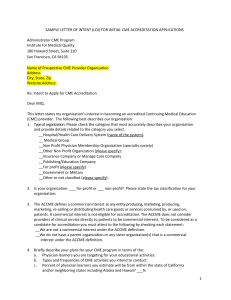
Office of Continuing Medical Education Form Due: FACULTY FINANCIAL DISCLOSURE FORM ACTIVITY INFORMATION: Speaker: Activity: Date: Role(s) in Activity: __ Activity Director __ Planning Committee __ Author (enduring material/poster/abstract) __ Speaker __Moderator As a CME provider accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Keck School of Medicine of USC, Office of Continuing Medical Education (OCME) upholds the Standards for Commercial Support of the ACCME and strives to assure balance, independence and scientific rigor in all sponsored educational activities and to eliminate commercial bias. Everyone in a position to control the content of a CME activity must disclose to the OCME and to the learners, all his/her relevant financial relationships with commercial interests and all potential conflicts must be resolved PRIOR to the activity. Disclosure: Conflict exists when you have a financial interest in a company and the opportunity to affect the CME content about that company’s product or service as related to your participation in this activity. Have you (or your spouse/partner) had a personal financial relationship in the last 12 months with the manufacturer of the products or services that will be discussed in this CME activity? ___ NO (skip to Balance in Content section) ___ YES (please list your disclosures below) Indicate categories of relevant financial relationships Name of Commercial Interest Consultant Paid Speaker Shareholder Grant/Research Other If you reported relevant financial relationships in the chart above, will any of these relationships impact your ability to present an unbiased presentation? ___ YES ____ NO Balance in Content Section: As a CME faculty, I am aware that: Presentations, individually or in combination during the activity, must give a balanced view of the therapeutic options. Generic names of products contribute to impartiality. If trade names are used, those of several companies should be used. For FDA regulated products, unapproved uses (i.e., “off-label” uses) must be identified as such. If information is to be presented that is not established medical practice, the information must be identified as such. I represent that the foregoing information is complete and truthful. ____________________________________________________ Signature of Reporting Individual ___________________ Date RESOLUTION OF CONFLICT OF INTEREST IS REQUIRED WHEN A FINANCIAL RELATIONSHIP IS DISCLOSED. Resolution of real or apparent conflict of interest will be accomplished by: (check one or more) ___ Signed Attestation Form ___ Peer review of content ___ Alter control over content ___ Exclude planner, presenter or author from participation ___ Other alteration, restriction or data ___________________________________________________________________________________ Reviewed and resolved by: Rev 8/13/13 __________________________________________________________________________________ Activity Director and/or OCME Date Page 1 Office of Continuing Medical Education Form Due: CONFLICT OF INTEREST RESOLUTION POLICY The Accreditation Council for Continuing Medical Education (ACCME) requires all accredited CME providers of CME have a mechanism in place for identifying and resolving potential conflicts of interest prior to an educational activity. The Keck School of Medicine of USC uses the Faculty Financial Disclosure and CME Disclosure Attestation Forms to accomplish this. Goal: The Keck School of Medicine Office of Continuing Medical Education’s (KSOM OCME) goal is to ensure that conflicts of interest are resolved in a manner consistent with the public good. In the context of continuing medical education, the solution could be achieved by eliminating, avoiding, or managing conflicts of interest in such a way that the educational program is designed to be free of commercial bias and is aligned with the public interest. Policy: 1. Activity directors, planning committee members, teachers/authors, and any others planning or participating in CME activities (contributors) shall disclose to the KSOM OCME any relevant financial relationships between themselves and commercial organizations. This disclosure will be accomplished by the completion of a Faculty Financial Disclosure Form, the contents of which will be shared with the audience, prior to the educational activity. 2. Faculty Financial Disclosure Forms will be reviewed prior to the CME activity by the KSOM OCME or its designee, in cases of joint sponsorship, and if a conflict exists, an appropriate course of action will be determined and taken. 3. An individual who refuses to disclose relevant financial relationships will be disqualified from being an activity director, planning committee member, or teacher/author of a CME activity and cannot have control of, or responsibility for, the development, management, presentation, or evaluation of the CME activity. 4. The KSOM OCME will document in writing how the identified, perceived conflicts of interest were resolved. 5. The following mechanisms for resolving conflicts of interest may be used to bring a successful conclusion: A. Signed Attestation: By completing and signing the CME Disclosure Attestation Form, the contributor agrees that said conflicts or relationships will not bias or otherwise influence their involvement in the CME activity, practice recommendations will be limited to those based on the best available evidence (or absence of evidence), and recommendations will be consistent with generally accepted medical practice. They also agree to all other mandatory ACCME disclosure guidelines. B. Audience Evaluation: Attendees will be advised of their right to expect non-biased presentations and queried regarding their impressions concerning bias (or the absence of bias) within the activity. Activity Directors and teachers/authors will receive copies of the evaluation summaries and comments. C. Prior Speaker Evaluations: Historical data, relating to the particular faculty from previous evaluations, can be used to document status of commercial bias. D. Altering Control Over Content: An individual’s control of CME content may be altered to remove the opportunity to affect content related to the products/services of a commercial interest. For example: Select someone else to control that part of the content: If a proposed presenter/author has a conflict of interest related to the content, choose someone else who does not have a relationship to the commercial interests related to the content. Change the content of the person’s assignment: The role of a person with a conflict of interest can be changed within the CME activity so that he/she is no longer teaching about issues relevant to the products/services of the commercial interest. For example, an individual with a conflict of interest regarding products for treatment of a disease state could address the pathophysiology or diagnosis of the disease rather than the therapeutics. Limit the content to a report without recommendation: If an individual has been funded by a commercial company to perform research, the individual’s presentation may be limited to the data and results of the research. Someone else can be assigned to address broader implications and recommendations. Limit the sources for recommendations to those based on best available evidence: Rather than having a person with conflict of interest present personal recommendations or personally select the evidence to be presented, limit the role of the person to reporting recommendations based on formal structured review of the literature with the inclusion and exclusion criteria stated (evidence-based). For example, the individual could present summaries from systematic reviews of a peer reviewed source, e.g., the Cochrane Collaboration (www.cochrane.org) E. Peer Review/Independent Content Validation: An informed learner or peer will review content. The extent of review depends on the circumstance. If the person performing the review knows the individual and the individual’s past views and presentations, a brief conversation may be adequate for the person performing the review to be confident that the presentation will be independent and balanced. If the person performing the reviews is not familiar with an individual’s views, a more extensive review (e.g., longer discussion, review of slides or handouts) may be necessary for the person performing the review to be confident of the presentation’s independence and balance. F. Altering Financial Relationships: Contributor’s relationship with commercial interest has changed or discontinued, and in doing so, no duty remains to introduce bias into the content. Although not relevant to conflict of interest, relationship must be disclosed to learners for 12 months. G. Elimination: Contributors who are perceived as either manifesting conflicts of interest or being biased may be eliminated from consideration as resources (committee members, teachers, authors, etc.) in subsequent certified CME activities. This policy will be reviewed annually by the OCME Committee. Rev 8/13/13 Page 2 Office of Continuing Medical Education Form Due: FACULTY ATTESTATION FORM Please indicate your understanding of and willingness to comply with each statement below. If you have any questions regarding your ability to comply, please contact the activity coordinator as soon as possible. Agree ____ Disagree ____ Disclosure: I have disclosed to the Keck School of Medicine of USC all relevant financial relationships, and am aware that this information will be disclosed to the learner in writing. ____ ____ Best Available Evidence: The content and/or presentation of the information which I am involved will promote quality or improvements in healthcare and will not promote a specific proprietary business interest of a commercial interest. Content for this activity, including any presentation of therapeutic options, will be wellbalanced, evidence-based, and unbiased. ____ ____ Free of Commercial Bias: CME content presented to learners will be free of commercial bias. No product, service or therapeutic option will be over-represented when comparing competing products, services and therapeutic options. ____ ____ Scientific Integrity: If I am providing recommendations involving clinical medicine, they will be based on evidence that is accepted within the profession of medicine as adequate justification for their indications and contraindications in the care of patients. All scientific research referred to, reported or used in CME in support of justification of a patient care recommendation will conform to the generally accepted standards of experimental design, data collection and analysis. ____ ____ Generic Names: If I am discussing specific healthcare products or services, I will use generic names to the extent possible. If I need to use trade names, I will use trade names from several companies when available and not just trade names from any single company. ____ ____ Off Label Use: Discussions during this activity may include off label use. According to the ACCME, all the recommendations involving clinical medicine in a CME activity are based on evidence that is accepted within the profession of medicine as adequate justification for their indications and contraindications in the care of patients. All scientific research referred to, reported or used in CME in support or justification of a patient care recommendation conforms to the generally accepted standards of experimental design, data collection and analysis. ____ ____ Content Review: I understand that the Keck School of Medicine of USC may need to review my presentation and/or content prior to the activity, and I will provide educational content and resources in advance as requested. ____ ____ HIPAA: I will comply with patient confidentially requirements as outlined in the Health Insurance Portability and Accountability Act (HIPAA). ____ ____ Copyright: I will obtain the necessary copyright permission(s) if any portion of my CME activity materials prepared is not my original work and if I do not hold the copyright. ____ ____ Payments: I have not and will not accept any honoraria, additional payments or reimbursements beyond the agreed upon honoraria, payments or reimbursements from the Keck School of Medicine of USC. I understand all payments made in compliance with the Keck School of Medicine of USC Office of Continuing Medical Education Honorarium and Expense Reimbursement Policy. If you disagree with any of the above statements, please state why: __________________________________________________ ____________________________________________________________________________________________________ I have carefully read and considered each item in this form, and have completed it to the best of my ability __________________________________ Please Print Last Name Rev 8/13/13 __________________________________ Signature Page 3 ____________ Date Office of Continuing Medical Education Form Due: October 3, 2012 CORE COMPETENCIES DESIGNATION FORM Speaker: The American Board of Medical Specialties (ABMS) and the Accreditation Council of Graduate Medical Education (ACGME) have embarked on a joint initiative to quantify and evaluate a set of 6 physician core competencies by which the individual physician will be measured for Residency Certification, Board Certification and more recently, Maintenance of Certification (MOC). To assist our conferees in demonstrating their completion of continuing medical education in the 6 core competencies we ask that each speaker indicate which of the core competencies (presentation may address more than 1 core competency) the educational content of their presentation will provide information or insight. PLEASE CHECK ALL THAT APPLY: 1. Patient Care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. 2. Medical Knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. 3. Practice-Based Learning and Improvement that involves investigation and evaluation of their own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care. 4. Interpersonal and Communication Skills that result in effective information exchange and teaming with patients, their families, and other health professionals. 5. Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. 6. Systems-Based Practice, as manifested by actions that demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. Core Competencies addressed will be indicated by numbers 1-6 adjacent to the title of your presentation in the conference syllabus. See attached sheet for a detailed summary of the Core Competencies. Signature: Date: Please complete this form and submit it to the Office of CME by fax (888)-665-8650, email (usccme@usc.edu), or mail Keck School of Medicine of USC Office of CME|1540 Alcazar Street CHP 208|Los Angeles, CA 90033 Rev 8/13/13 Page 4 CORE COMPETENCIES INFORMATION SHEET PATIENT CARE Physicians must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. CME programs address these issues if the topics relate to: The ability to communicate effectively and demonstrate caring and respectful behaviors when interacting with patients and their families. Gathering essential and accurate information about their patients. Making informed decisions about diagnostic and therapeutic interventions based on patient information and preferences, up-to-date scientific evidence, and clinical judgment. Developing and carrying out patient management plans. Counseling and educating patients and their families. Using information technology to support patient care decisions and patient education. Performing competently all medical and invasive procedures considered essential for the area of practice Providing health care services aimed at preventing health problems or maintaining health. Working with health care professionals, including those from other disciplines, to provide patient-focused care. MEDICAL KNOWLEDGE Physicians must demonstrate knowledge about established and evolving biomedical, clinical, and cognate (e.g. epidemiological and social-behavioral) sciences and the application of this knowledge to patient care. CME programs address these issues if the topics relate to: Demonstration of an investigatory and analytic thinking approach to clinical situations. Knowledge and application of the basic and clinically supportive sciences which are appropriate to their discipline. PRACTICE-BASED LEARNING AND IMPROVEMENT Physicians must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices. CME programs address these issues if the topics relate to: Analyzing practice experience and performing practice-based improvement activities using a systematic methodology. Locating, appraising, and assimilating evidence from scientific studies related to their patients’ health problems Obtaining and using information about their own population of patients and the larger population from which their patients are drawn. Applying knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness. Using information technology to manage information, access on-line medical information; and support their own education. Facilitating the learning of students and other health care professionals. Rev 8/13/13 Page 5 INTERPERSONAL AND COMMUNICATION SKILLS Physicians must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients families, and professional associates. CME programs address these issues if the topics relate to: Creating and sustaining a therapeutic and ethically sound relationship with patients. Using effective listening skills and eliciting and providing information using effective nonverbal, explanatory, questioning, and writing skills. Working effectively with others as a member or leader of a health care team or other professional group. PROFESSIONALISM Physicians must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. CME programs address these issues if the topics relate to: Demonstrating respect, compassion, and integrity; responsiveness to the needs of patients and society that supersedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development. Demonstrating a commitment to ethical principles pertaining to provision or withholding of clinical care, confidentiality of patient information, informed consent, and business practices. Demonstrating sensitivity and responsiveness to patients’ culture, age, gender, and disabilities. SYSTEMS-BASED PRACTICE Physicians must demonstrate an awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value. CME programs address these issues if the topics relate to: Understanding how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society and how these elements of the system affect their own practice. Knowing how types of medical practice and delivery systems differ from one another, including methods of controlling health care costs and allocating resources. Practicing cost-effective health care and resource allocation that does not compromise quality of care. Advocating for quality patient care and assisting patients in dealing with system complexities. Knowing how to partner with health care managers and health care providers to assess, coordinate, and improve health care and knowing how these activities can affect system performance. Rev 8/13/13 Page 6