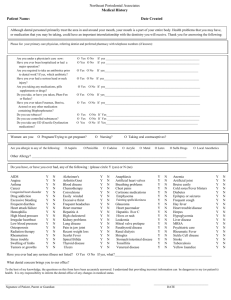
Infectious Disease Improvement Checklist
advertisement

Infectious Disease Improvement Checklist Goals 1. 95% of pregnant women will be offered testing for Gonorrhea and Chlamydia. 2. 95% of pregnant women who are at-risk (either through social factors or positive test) will be offered rescreening/ re-testing for Gonorrhea and Chlamydia by 34 weeks. 3. 75% of pregnant women will be offered a flu vaccination while pregnant. 4. 90% of pregnant women will be examined for Periodontal Disease. 5. 90% of pregnant women identified as possibly having Periodontal Disease will be referred for dental care, if available in community. The dental piece was newer for us…Though we always did our exam for dentition, now we’re more interested in following up on that and saying, “Okay, what can we do about this?” (midwife, rural OB practice) We’ve always screened for STDs in the first trimester. The difference now is that we re-screen in second trimester. (midwife, rural OB practice) Sexually Transmitted Infections (Chlamydia, Gonorrhea, Syphilis) The Preventive Screening Task Force and ACOG guidelines recommend screening all pregnant women for common, generally asymptomatic, sexually transmitted infections, such as Gonorrhea and Chlamydia (GC). Other guidelines suggest risk-based screening focusing on age (< 25 years old), behavior (multiple sexual partners or history of STIs) and prevalence of gonorrhea and syphilis in the population. Additionally, women who are found to be at risk and are being screened for sexually transmitted infections during early pregnancy are often not rescreened later in pregnancy, and women at high risk for STIs are generally not counseled about the well recognized, STI-preventive benefits of condom use even during pregnancy.1,2 Assess Offer STI testing to all patients at the 1st prenatal visit. Assess for lifestyle factors and the need for re-screening. Document if patient declines test. Intervene Hand out educational materials at the 1st prenatal visit Follow up Repeat GC screening by 34 wks for women at high risk and those previously treated. Repeat screening raises the predictive value and is necessary to know that treatment was successful. Important to re-screen patients who have a prior positive test during pregnancy and re-screen those with lifestyles that put them at-risk. HIV Assess Offer to all patients. Document if patient declines test. Hepatitis B The ACOG and AAP recommend universal screening for Hepatitis B with the use of Hepatitis B Surface Antigen (HBSAg) and early treatment (within 12 hours of birth) of neonates with HBSAg positive mothers. It is estimated that at least half neonatal Hepatitis B infections may be preventable by use of the maternal test (HBSAg), maternal 1 United States Preventive Services Task Force (USPSTF). Department of Health and Human Service. Guide to Clinical Preventive Services. Washington, DC. 2001. 2 Primary and Preventive Care: Periodic Assessments. American College of Obstetricians and Gynecologists Committee on Gynecologic Practice. Committee Opinion No. 293. November 2003. re-screening when appropriate, and notifying pediatric providers of positive maternal screening in a timely manner.3 Document Hepatitis (HBSAg) status on all prenatal patients. If maternal status is unknown at the time of delivery, hospital standing orders are such that neonate will receive immunoglobulin within 12 hours. Maternal Hepatitis status must be documented and accessible in prenatal record to avoid unnecessary treatment. Document if patient declines newborn treatment. Influenza Current guidelines place pregnant women in a high risk category concerning influenza and recommend vaccination during flu season, regardless of gestational age. Additionally, women with significant chronic diseases should get vaccinated at any point in their pregnancy. Assess Offer every pregnant woman an influenza vaccination during flu season (October through March or April for the Northern Hemisphere) regardless of gestational age. Intervene Vaccinate pregnant women October through April as this is the optimal time. Reassure patient that vaccination is not harmful, even in the first trimester Follow-up If patient referred out of office, ensure vaccination was received. Document vaccination even if done out of office Periodontal Disease There is strong emerging evidence of a significant association between Periodontal Disease and preterm delivery. Dental health should be a routine part of the prenatal evaluation.4 Practices participating in IPCV experienced considerable problems with referring pregnant women for dental care within Vermont. Documentation regarding assessment and the lack of access to dental resources may help provide evidence to assist in the development of effective and available dental care during pregnancy. Access to care is especially challenging for the Medicaid population. This is an important topic for statewide policy development. Assess Screen all patients for Periodontal Disease by examining the oral cavity at the 1st prenatal visit. Intervene Refer for dental care when evidence of Periodontal Disease is present or suspected or the patient has not had dental care in the last year Refer patients with suspicion of Periodontal Disease for dental care. Though prenatal care providers may not feel qualified to absolutely determine the presence of Periodontal Disease in every patient, it is important to refer those who appear to have decay and irritated gums. Follow-up Ensure dental care was received. Document lack of available resources, if applicable. Suggestions for Monitoring Your QI Efforts To assess whether your intended change in practice is occurring and is being documented, regularly (i.e., quarterly) review patient charts within the first and third trimesters for the following indicators: Was patient screened for GC and Chlamydia? Was patient re-tested if positive and/or re-screened if at risk due to social factors by 34 weeks? 3 Antepartum Care. In: Guidelines for Perinatal Care. Fifth Ed. American Academy of Pediatrics and American College of Obstetricians and Gynecologists. October 2002. 4Jeffcoat M, Geurs N, Reddy M, Cliver S, Goldenberg R, Hauth J. Periodontal infection and preterm birth: Results of a prospective study. J Amer Dent Assoc 2001;132:875-80. Is the date of influenza vaccination recorded? Did the patient receive an evaluation for Periodontal Disease? Was evidence of Periodontal Disease found? If yes, was referral made for dental care? If resources unavailable was there documentation of this? Is there documentation of HIV screening offered and results noted, if applicable? If patient declined testing for GC and Chlamydia or influenza vaccination, was it documented? Was Hepatitis B Surface Antigen screening performed? Is Hepatitis B Surface Antigen result easily accessible within the prenatal chart? Resources — Center for Disease Control (http://www.cdc.gov) — Vermont Department of Health for current statistics – state or county specific rates of testing and infection — March of Dimes Web site: http://www.marchofdimes.com (English) or http://www.nacersano.org (Spanish). To order a catalog or multiple copies of materials, call 1-800-367-6630. - Prenatal Care (booklet) (also available in Spanish) - Preconception Health Promotion: A Focus for Women's Wellness (nursing education) - High-Risk Antepartal Home Care (nursing education) Other References - Periodontal Disease — Emmons-Wener M, Lavigne SE. (2004). Can periodontal disease lead to premature delivery?: How the mouth affects the body. AWHONN Lifelines, 8(5), 422-31. — Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldenerg RL, Hauth JC. (2001). Periodontal infection and pre-term birth: results of a prospective study. J Am Dent Assoc, 132 (7), 875-80 — Lopez NJ, Smith PC, Gutierrez J. (2002). Periodontal therapy may reduce the risk of pre-term low birth weight in women with periodontal disease: a randomized controlled trial. J Periodontol, 73(8), 911-24.