Infections
advertisement

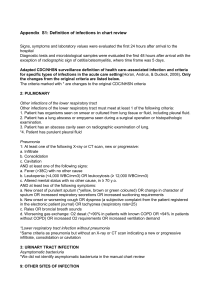
INFECTIONS This summary and its accompanying materials are provided primarily for the use of front-line caregivers in the longterm care facility, and for reference use by nursing home medical directors and the Quality Improvement Organizations (QIOs) that partner with them under the Nursing Home Quality Initiative (NHQI) by the Centers for Medicare and Medicaid Services (CMS). It is not intended to be complete, to represent a thorough, academic approach to the subject for general use by physician, or to imitate a peer-reviewed medical journal article. It is limited to those eight infection topics chosen by CMS for NHQI. Infections epidemics. The most common outbreaks are of respiratory, gastrointestinal tract, and skin infestations. The common endemic infections are in the urinary tract, and skin or soft tissue. The overall burden of infection in LTCFs ranges from an incidence of three to seven infections per 1000 resident-care-days. Residents of long-term care facilities (LTCFs) have a high prevalence of infections, which are a major cause of morbidity, mortality, hospital transfers, and a source of considerable expense. The literature indicates that there is concern about management of infections in LTCFs and whether it is optimal. The diagnosis, treatment, and surveillance of infection in the nursing home setting is made more difficult in this elderly population by a number of factors. Residents may have various degrees of immune compromise, from aging alone, due to difficulties with nutrition, or due to coexisting disease. This may result in atypical manifestations and presentations of infection. Limited staffing, lack of rapid access to physician attention, and lack of onsite availability of laboratory and imaging support may contribute to these difficulties. The variability among LTCFs in their patient populations may determine different service needs and solutions. One example is tuberculosis, which is a larger problem in areas having a high rate of tuberculosis in the general community, but may be only a potential problem in other areas, and thus The aging population of America represents an increasing public health priority. Citizens living to “old-old” age (i.e., greater than 85 years) comprise the most rapidly growing segment. The trends to smaller families and continuing geographical mobility with dispersal of family members point to increasing need for long-term care services in the future. Currently there are 1.7 million residents of LTCFs, and this number is expected to triple by 2030. Residents in LTCFs are at increased risk of infections, because they are undergoing physiologic aging, have a greater number of comorbidities, and they live in an institutional environment. Each factor makes them especially more susceptible during Infections 1 Prevention the frequency of surveillance screening would differ. Prevention of infections in long-term care facilities begins with thorough maintenance of an active lifestyle, proper nutrition, and appropriate management of underlying diseases, sanitation, hygiene, and compulsive attention to good hand washing by all staff, adherence to accepted food handling procedures, and maintenance of ventilation and plumbing systems. Education of staff, as well as residents and visitors, is helpful in avoiding transmission of known illnesses, especially those spread by airborne droplets (chicken pox, tuberculosis, measles, influenza) and by direct contact (staphylococcus and streptococcus diseases, especially multiantibiotic resistant organisms, and chronic hand carriage of gram-negative organisms). Employee health policies that provide paid leave during illness with a contagious disease, identification of employees with chronic conditions, such as dermatitis or infections, and recognition and immunization of those not immune to chicken pox help to prevent spread of illnesses between staff, residents, and visitors. In addition, special emphasis is warranted in encouraging all staff to obtain annual immunization against influenza. There is strong support in the literature showing that adequate influenza immunization of nursing home staff is effective in preventing influenza outbreaks. The increasing problem of the general use of empirical antibiotic treatment in the community and the resultant rise of antibiotic resistant organisms in the long term care setting (and elsewhere) further complicate the issue of infection in this setting. Frequently mentioned as contributing to antibiotic resistance is the empiric treatment for common infections such as indwelling catheter-associated UTIs, decubitus ulcers, and pneumonia. Current guidelines and literature on these conditions address the problem of resistance help to minimize it if followed. Infections represent up to 50% of the reasons for transfers to hospitals, comprising up to 300,000 admissions per year, and costs are estimated to approach $2 billion each year. Direct costs for antimicrobial therapies alone are estimated between $40 and $140 million per year. There is concern that the public health cost in terms of increased antibiotic resistance may be huge, and the decrease in quality of life, morbidity, and premature mortality for the residents of LTCFs is unmeasured. The Nursing Home Quality Initiative highlights increasing awareness and concern for this public health priority, and recognizes the need for increased prevention and control of infections in long-term care facilities. A renewed focus of attention toward improvement of the quality of care delivered in LTCFs, begun with the Omnibus Budget Reconciliation Act in 1987 and continued during the recent six years of work by the Quality Improvement Organizations under CMS, is evidenced in the choice of quality measures reported under this new initiative. Infections Primary prevention includes the proper treatment of underlying diseases (i.e., congestive heart failure, chronic obstructive pulmonary disease, stroke, diabetes, etc.) and avoidance of invasive devices such as urinary tract catheters when possible. In addition, oral and dental care may be an important strategy for prevention of infectious complications of aspiration pneumonia. 2 Bibliography Direct prevention of certain infections for residents is provided through immunization of both residents and staff, illustrated by use of pneumococcal and influenza vaccines, but also tetanus/diphtheria inoculation. Annual national targets for the 65 years and older population have been set for influenza and pneumococcal immunizations, leading to the 2010 goal of 90% coverage. Unfortunately, both influenza and pneumococcal vaccines remain underutilized, with the 2000 targets of 80% coverage for each not achieved. Nationally, only 38% coverage was achieved for pneumococcal immunization and 65% for influenza. Evidence of the efficacy of annual influenza immunizations in reduction of infection, morbidity, and mortality is compelling, and cannot be overstressed. A bibliography with complete citations and annotations on infections in the nursing home environment has been developed for this Quality Initiative. Guidelines and articles accompanying this text are mentioned under the categories presented below. In addition, review of materials presented at a conference by the Emory University Center for Health in Aging in March 2001 at Alpharetta, Georgia, contributed to this summary commentary. In the search for materials useful for LTCFs in addressing the subject of infections and infection control, the major criteria were usefulness and applicability in the nursing home environment by the nurses and nurses’ aides actually doing the work. While academic completeness and erudition are laudable, and ongoing investigation produces the evidence base supporting advances in care practices, those faced with the limits and demands of the LTCF environment require a focus on the actual "how to" instruction and basic understanding of the task and its elements. Another strategy for prevention is the early detection for intervention of outbreaks of infections, as well as identification of other infections in their asymptomatic stage in order to delay or prevent symptoms and morbidity. In this elderly population, declining physical responses such as ability to mount a fever or increase the white blood cell count in the face of infecting organisms makes recognition of the presence of infection difficult. Infection Control The importance of infection control is widely recognized in LTCFs, where the group living situation increases the exposure and risk of outbreaks. There is extensive regulation addressing this important aspect of long-term care delivery, and a cadre of professionals with its body of literature has emerged. However, it is well known that LTCFs are chronically understaffed, and the infection control professionals have many other duties and responsibilities. In addition, as many as half of those performing infection control duties have not had specific training, and most spend only about eight Because it is difficult to establish a clinical diagnosis of infection in residents of LTCFs, deciding when to initiate antibiotics is a challenge for practitioners. An article by Loeb et al. (2001), “Development of Minimum Criteria for the Initiation of Antibiotics in Residents of Long-Term Care Facilities: Results of a Consensus Conference,” provides useful guidance. Criteria for initiating antibiotics for skin and soft-tissue, respiratory and urinary infections, and fever where the focus of infection is unknown are included. Infections 3 Fever hours per week on those infection control issues. Furthermore, many of those efforts focus on data collection, without a direct link to intervention measures. Lastly, much of the work in infection control has been done in hospitals and is not directly applicable or appropriate to the nursing home environment. On the importance and role of fever as a marker of infection, a guideline is provided by Norman (1992) from the Clinics in Geriatric Medicine: “Infections in Elderly Persons: An Altered Presentation.” It addresses the special and unique characteristics of infections in the elderly as noted above and provides direct information useful in the LTCF. Lindsay highlights the diagnosis, treatment, and prevention of fever in nursing home patients, and discusses typical and atypical febrile responses and their infectious and noninfectious sources. Also included is the Practice Guideline for Evaluation of Fever and Infection in LTC Facilities, a recently published set of standards from the Infectious Diseases Society of America. They provide a practical approach to evaluation of potential infection and assistance in early recognition and treatment by nursing home personnel. In-depth information and an extensive bibliography for QIO reference are included. The updated guideline referenced by the Society of Hospital Epidemiologists of America (SHEA) Long-Term Care Committee and Association for Practitioners in Infection Control (APIC) Guidelines Committee, entitled “Infection Prevention and Control in the Long-Term Care Facility,” reviews the literature on infections and infection control programs in LTCFs. It covers such topics as tuberculosis, bloodborne pathogens, epidemics, isolation systems, immunization, and antibioticresistant bacteria, and is an excellent resource. Articles are included that review risk factors for infection in LTCFs and provide the components of an infection control program (Nicolle and Garibaldi, 1995), and summarize interventions that may prevent infections, identify outbreaks early, and minimize prevalence of resistant organisms (Nicolle, 2000). A source of information on the multiple antibiotic-resistant unusual organisms (Strasbaugh et al., 1996) and a nurses’ aide-centered prospective study on intensive surveillance (Jackson et al., 1993) should assist in management of these difficult problems. The latter is especially useful in that it provides insights on how the frontline certified nurse-assistant (CNA) staff view symptoms of infection and their dependence on simple signs such as fever. Infections Infections in LTCFs Specific types of infections in LTCFs are highlighted. Pulmonary infections (pneumonia, recurrent lung-aspirations, other respiratory infections), urinary tract infections, wound infections and septicemia, are included: Pulmonary Infections Pneumonia A LTCF-oriented guideline from the Institute for Clinical Systems Improvement provides an analytic framework to assist practitioners in LTCFs in evaluating and treating residents with community-acquired pneumonia and understanding the rationale for treatment choices. Two articles by Mulder (1998, 2000) are included. A review 4 of the literature on pneumonia in LTCFs thoroughly covers risk factors, etiology, clinical presentation, treatment, and prevention. The second is included for its completeness and bibliography as a reference source for QIO use in this project. chronic aspiration in the etiology of nocosomial pneumonia. Two-thirds of the patients in their study were found to have a history of recurrent aspiration and were more likely to require tube or assisted oral feedings. Pick et al. (1996), identified tube feeding, presence of a hyperextended neck contraction, malnutrition, and the use of benzodiazepines and anticholinergics as risk factors for aspiration in their study published in the Journal of the American Geriatric Society. An overview of the disorders that place the LTCF resident at risk for aspiration, as well as a discussion of evaluation, treatment, and prevention is provided by Teofilo and Lee-Chiong (1998) in the Annals of Long-Term Care. Lastly, the American Speech-Language-Hearing Association (2000) provides as a desk reference, guidelines for the use of instrumentation in the assessment, diagnosis, management, and treatment of patients with dysphasia. The article by Fried et al. (1995) covers the factors associated with the decision to treat or transfer the patient to the hospital. It shows that the time of day the attending physician is contacted by LTCF staff is a major determinant of the decision to transfer, and that no difference in survival was demonstrated between treatment in the LTCF or hospital location for cases with mild to moderate pneumonia. Additional publications on this subject indicate that those with severe pneumonia do better on intravenous antibiotics, which have usually mandated hospital transfer, but some LTCFs do now have the capability of offering such therapy, along with good nursing monitoring of the patient. Lastly, an editorial from the Journal of the American Geriatrics Society (Zimmer, 1997) emphasizes an individualized approach to the LTCF resident with pneumonia and provides the opposing view by favoring hospitalization for treatment. Other Respiratory Infections Tuberculosis Screening for tuberculosis at admission has long been practiced, even mandated, in LTCFs; but there is increasing concern that annual screening is not being performed, or is inadequate to identify residents with reactivated TB who might pose a risk to other residents and staff. Two references for the prevention and control of tuberculosis are included. Bentley (1990) summarized recommendations for prevention and control of TB from the DHHS Advisory Committee for the Elimination of Tuberculosis, and reviews an outbreak in a large, wellrespected LTCF, thus underscoring the importance of careful TB surveillance for this serious and extremely contagious disease. He points out that the current estimated incidence of TB in LTCF residents was 39.2 per 100,000 person years, “Prevention and Control of VaccinePreventable Diseases in Long-Term Care Facilities” is a comprehensive supplement from the American Medical Directors Association Journal (2000), which provides a "plug-in" process and complete instructions for LTCFs to implement an immunization program and surveillance for influenza and pneumococcal disease. It is an excellent reference for use by both the LTCF and its supporting QIO. Recurrent Lung Aspiration McDonald et al. (1992), highlight in the Journal of Infection Control the role of Infections 5 compared to the incidence of 21.5 per 100,000 person years among elderly persons living in the community. The observed rate of tuberculosis for employees of LTCFs was 3.0 times the rate expected in employed adults of similar age, race, and sex. Rajagopalan and Yoshikawa outline the epidemiology and clinical features of TB in the elderly and point out that the often subtle clinical manifestations present diagnostic challenges. The use of the familiar two-step testing in older persons is emphasized. discussed in Falsey (1991). These types of infections often occur as "outbreaks" or case-clusters in nursing homes. In addition, Heath et al. (1997) present two fatal LTCF cases of Haemophilus Influenzae Type B infection transmitted within the facility. This vaccine-preventable disease, usually seen in young children, may be under-recognized in the elderly. Urinary Tract Infection The position paper developed by the SHEA Long-Term Care Committee (Nicolle, 2001) is included to assist LTCFs, as well as physicians and QIOs, in dealing with this common and difficult problem. It is a "must" for understanding and managing UTI in this setting. In addition, the current CDC guideline covering epidemiology, control, and prevention of catheter-associated UTI, with an extensive bibliography, provides an authoritative reference. The University of Michigan Health System guideline on UTI diagnosis, management, treatment, and follow-up provides a helpful clinical algorithm. An excellent "in-service" TB training is provided in the nurse-conducted review of tuberculosis by Schultz et al. (2001), concerning new converters in LTCF settings. A classic paper on significance of the PPD in the elderly by Stead and To (1987) is based on a study of almost 50,000 residents. They specify that conversion with an increase of at least 12mm or more from those with previously documented negative PPDs indicated occurrence of infection. If not treated at that time, 7.6% of women and 12.7% of men developed active disease. They point out that as many as 25% of those clinically ill with TB may show no reaction to 5 units of tuberculin. In their experience, 61% of cases of (active) tuberculosis in nursing homes developed among previous reactors to tuberculin, assumed to be the result of old infection. Viral Hepatitis A study by Marcus and Tur-Kaspa (1997) offers a review of the epidemiology, manifestations, and prevention of hepatitis in elders and deals with all known types, including A, B, C, D, and G. It points out that age is not necessarily an exclusion criterion for anti-viral treatment. Chien et al. (1999) found anti-HCV was surprisingly high in a study of three LTCFs and recommends that all new patients admitted be screened for anti-HCV. The comprehensive CDC guideline on Hepatitis C virus is also included for QIO and clinician reference for its extensive bibliography. Influenza The Centers for Disease Control and Prevention guideline, “Prevention and Control of Influenza 2002,” is presented as the current and definitive treatise on prevention and treatment of influenza and control or outbreaks in LTCFs. Other Unusual Respiratory Infections Viral infections including respiratory syncytial, parainfluenza, rhinovirus, coronavirus, and adenovirus in LTCFs are Infections 6 LTCF setting. Muder et al. (1992) provide an excellent reference, showing that the urinary tract source accounted for 55% of bacteremia, while respiratory tract (11%) and soft tissue (9%) infections were the other major sources. In this study, mortality was significantly associated with the respiratory tract infection bacteremia. Wound Infections Two cases of peri-stomal wound infection associated with bacteremia in the same LTCF caused by the nocosomial pathogen, Group A streptococcus, presumably spread by a nurse with Group A streptococcal pharyngitis, are presented by Tsai and Bradley (1992). This highlights the fact that wound infections with common pathogens can result in serious consequences, including spread within the nursing home. Prompt identification and treatment of both carriers, and residents with infected wounds, is important to prevent spread of disease. References Bentley DW. Tuberculosis in long-term care facilities. Infection Control and Hospital Epidemiology. 1990; 11: 42-46. Chien NT, Dundoo G, Horani MH, et al. Seroprevalence of viral hepatitis in an older nursing home population. Journal of the American Geriatric Society 1999; 47: 11101113. The common problem of infections in pressure ulcers is dealt with under that separate topic. A guideline, “Treatment of Pressure Ulcers,” from the U.S. Department of Health and Human Services, Public Health Service, AHCPR, is included to cover the management of bacterial colonization and infection, as well as education and quality improvement concerning pressure ulcers in the LTCF environment. Falsey AR. Noninfluenza respiratory virus infection in long-term care facilities. Infection Control and Hospital Epidemiology 1991; 12: 602-608. Fried TR, Gillick MR, and Lipsitz LA. Factors associated with hospitalization and outcome of elderly long-term care patients with pneumonia. Journal of General Internal Medicine 1995; 10: 246-250. Septicemia Llewelyn and Cohen's (2001) reference covering general considerations in the diagnosis of septicemia and the importance of appropriate microbiological diagnosis, markers of infection, and literature-based recommendations is provided for LTCF Medical Directors use. A review of clusters of Group A Streptococcal infection in LTCFs is presented to underscore the importance of this contagious and dramatic illness presenting with a toxic-shock-like syndrome. Studies by Leibovici et al. (1993) and Richardson et al. (1995) deal with this problem of septicemia and highlight the status of the urinary tract infection, especially those associated with urinary incontinence or indwelling catheter use, as the most frequent source of septicemia in the Infections Health TC, Hewitt MC, Jalaludin B, et al. Invasive Haemophilus influenzae type b disease in elderly nursing home residents: Two related cases. Emerging Infectious Diseases 1997; 3(2): 179-182. Jackson MM, Schafer K. Identifying clues to infections in nursing home residents: The role of the nurses’ aide. Journal of Gerontological Nursing 1993; Jul: 33-42. Leibovici L, Pitlik SD, Konisberger H, and Drucker M. Bloodstream infections in 7 patients older than eighty years. Age and Ageing 1993; 22: 431-442. Nicolle LE. Infection control in long-term care facilities. Clinical Infectious Diseases 2000; 31: 752-756. Llewelyn M and Cohen J. Diagnosis of infection in sepsis. Intensive Care Medicine 2001; 27: S10-S32. Nicolle LE and Garibaldi RA. Infection control in long-term-care facilities. Infection Control and Hospital Epidemiology 1995; 16: 348-353. Lindsay JM, Greenough WB, Zelesnick LB, and Kuhn KE. Fever in the nursing home resident. Maryland Medical Journal 1994: 159-164. Nicolle LE and the SHEA Long-Term Care Committee. Urinary tract infections in longterm care facilities. Infection Control and Hospital Epidemiology 2001; 22: 167-175. Loeb M, Bently DW, Bradley S, et al. Development of minimum criteria for the initiation of antibiotics in residents of longterm-care facilities: Results of a consensus conference. Infection Control and Hospital Epidemiology Feb 2001; 120 (2): 210-124. Norman DC and Toledo SD. Infections in elderly persons: an altered clinical presentation. Clinics in Geriatric Medicine 1992; 8(4): 713-719. Marcus EL, Tur-Kaspa R. Viral hepatitis in older adults. Journal of the American Geriatric Society 1997; 45: 755-763. Pick N, McDonald A, Bennett N, et al. Pulmonary aspiration in a long-term care setting: Clinical and laboratory observations and an analysis of risk factors. Journal of the American Geriatric Society 1996; 44: 763-768. McDonald AM, Dietsche L, Litsche M, et al. A retrospective study of nosocomial pneumonia at a long-term care facility. American Journal of Infection Control 1992; 20: 234-238. Prevention and Control of VaccinePreventable Diseases in Long-Term Care Facilities. Journal of the American Medical Directors Association Sep/Oct 2000; 1(5): S1-S37. Muder RR. Approach to the problem of pneumonia in long-term care facilities. Comprehensive Therapies 2000; 26(4): 255262. Rajagopalan S and Yoshikawa TT. Tuberculosis in long-term-care facilities. Infection Control and Hospital Epidemiology 2000; 21: 611-615. Muder RR. Pneumonia in residents of longterm care facilities: Epidemiology, etiology, management, and prevention. The American Journal of Medicine. 1998; 105: 319-330. Richardson JP and Hricz L. Risk factors for the development of bacteremia in nursing home patients. Archives of Family Medicine 1995; 4: 785-789. Muder RR, Brennen C, Wagener MM, et al. Bacteremia in a long-term-care facility: A five-year prospective study of 163 consecutive cases. Clinical Infectious Diseases 1992; 14: 647-654. Infections Schultz M, Hernández JM, Hernández NE, and Sanchez RO. Onset of tuberculosis disease: New converters in long-term care settings. American Journal of Alzheimer’s 8 Disease and Other Dementias. 2001; 16(5): 313-318. Schwartz B, Elliott JA, Butler JC, et al. Clusters of invasive group A streptococcal infections in family, hospital, and nursing home settings. Clinical Infectious Diseases 1992; 15: 277-284. Shugarman LR, Rhew DC, Badamgarav E, et al. Interventions to improve the quality of care in nursing homes: A systematic review update 1. Zynx Health Incorporated: 19 Nov 2001. Strausbaugh LJ, Crossley KB, Nurse BA, Thrupp LD, and the SHEA Long-Term-Care Committee. Antimicrobial resistance in long-term-care facilities. Infection Control and Hospital Epidemiology 1996; 17: 129140. Stead WW and To T. The significance of the tuberculin skin test in elderly persons. Annals of Internal Medicine 1987; 107: 837842. Treatment of Pressure Ulcers. U.S. Department of Health and Human Services, Public Health Service, AHCPR. 1994. Available online: http://www.guidelines.gov Tsai CC and Bradley SF. Group A streptococcal bacteremia associated with gastrostomy feeding tube infections in a long-term care facility. Journal of the American Geriatrics Society 1992; 40: 821823. Zimmer JG and Hall WJ. Nursing homeacquired pneumonia: Avoiding the hospital. Journal of the American Geriatrics Society 1997; 45: 380-381. Infections MO-02-01-NHI December 2002 This material was prepared by Primaris under contract with the Centers for Medicare & Medicaid Services (CMS). The contents presented do not necessarily reflect CMS policy. Version 12/20/2002 9