975
advertisement

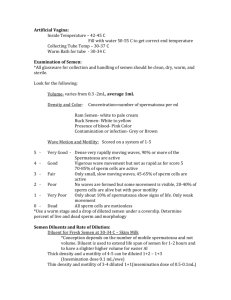
EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 Hussein et al THE EFFECT OF BENZENE ON SEMINAL PARAMETERS AND TESTICULAR FUNCTION By Alayman F. Hussein, Mamdouh Abol-Nasr, and *Manal Abd El-Aziz Departments of Urology and *Forensic Medicine El-Minia Faculty of Medicine ABSTRACT: Objective: To investigate the effect of prolonged exposure to benzene on the semen parameters and hence male reproductive function among men working at gas stations and occupationally exposed to these chemical substances. Participants: Eighty-eight workers at gasoline service stations with a mean age of 33.51±5.72 (Range: 24-52) were included in this study. Participants were exposed to benzene and related products with a duration of exposure varied from one upto 28 years (mean: 8.57±5.39). Methods: All participants are subjected to clinical history taking and physical examination including measuring the size of both testes. Semen analyses were performed to all participants. In addition, we measured a morning blood sample for serum testosterone and follicular stimulating hormones. The data were then studied and analyzed for the correlation between the seminal parameters and hormonal profile, and the duration of exposure to benzene Results: The most evident abnormal semen characteristics include reduction in sperm concentration, motility, normal morphological forms, and the semen volume. The duration of exposure correlates with the declined quality of seminal variables. We found that sperm motility and concentration are affected first (after 5 years), then sperm morphology, and seminal volume are affected later (after 7 years). Conclusion: Occupational exposure to benzene could adversely interfere with the human reproduction and fertility. The mechanism of these effects is not known. Further molecular biological studies on the male reproductive organs are required. KEY WORDS: Benzene Male infertility Semen Aromatic hydrocarbons INTRODUCTION: Benzene is a liquid inflamemable, and volatile organic compound that is obtained on refinement of the crude petroleum. This organic substance is one of the aromatic hydrocarbons. It is made up primarily from many carbon and hydrogen atoms. Benzene is added to prevent engine knocking with a subsequent exposure through the cars' exhaust fumes and evaporation from gasoline service stations. Absorption of benzene is either by inhalation of contaminated air or by dermal exposure.1 Polychlorinated aromatic hydrocarbons (PCAHS) have been described as endocrine disruptors in animals and in accidentally or occupationally exposed humans. Environmental exposure to the PCAHS may interfere with sexual maturation and in the longterm, they have an adverse effect on the human reproduction.2 320 EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 Since forty years, the public in the western world has become increasingly concerned and worry about the toxicity of environmental pollutants in relation to the fetal development and human reproduction. The more recent epidemiologic evidence of the decreased quality of human sperm has drawn attention to effects on the male reproductive system.3 Hussein et al sperm concentration, sperm motility and percentage of abnormal sperm forms. A morning blood sample was withdrawn for the measurement of the follicular stimu-lating hormone (FSH) level, total serum testosterone level, and Leutininzing hormone (LH) level with the immunometeric assay using commercially available kits and the automated analyzer. Continuous variables were expressed as mean ± standard deviation. Parameters of semen analysis were compared to the normal values established by the WHO*. All examined variables were correlated to the duration of exposure to benzene and to the age of the participants. Pearson Correlation Coefficient test, independent sample t test, Fisher’s exact and Mann–Whitney U tests were used for comparison of continuous variables when appropriate, while the chi-square test was used to compare categorical variables, with a p value less than 0.05 considered significant. A statistics software (SPSS) was used for statistical analysis. Participants and Methods This study was conducted in one year duration at El-Minia University in the period from April 2004 to April 2005. A total of 88 men working at gasoline service stations at the governorate and occupationally exposed to benzene are included in this study. The mean age of the patients was 33.51±5.72 years (range: 24-54 years) and the mean duration of exposure to benzene was 8.57±5.39 years (range: 1-28 years). Participants involved in this study had normal testes without any varicocele. Any participant under radiotherapy or chemotherapy, and those who were receiving treatment to improve spermatogenesis were excluded. RESULTS: Out of the included 88 workers, 72 patients were married with 24 of them suffered primary infertility on their marriage (33.3%). According to standardization of WHO, abnormal seminal parameters were detected in 28 out of 88 workers (31.8%). The mean semen volume in all workers was 2.9 ml, the mean sperm concentration was 40.8±41.8 million/ml, the mean sperm motility was 33.3±21% and the mean normal sperm morphology was 41.4±19.8%. After clinical history taking, physical examination was done including the external genitalia where the size of both testes was measured by means of the Prader's orchidometer. The longitudinal accesses of both testes were measured separately, and mean volume of both testes was calculated. Semen analysis, according to standards of The World Health Organization (WHO), was done with a report including the semen volume, 321 EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 Hussein et al Table (1): Semen parameters, testicular longitudinal axis, testosterone and FSH serum levels in Gas Station workers participants Semen volume Sperm conc. (million/ml) Sperm Motility Normal sperm forms Right testis longitudinal Axis Left testis longitudinal Axis Total testosterone (ng/dl) FSH (ng/dl) Minimum 2 ml 0.00 0% 5% 2 cm 2 cm 99 1.0 The mean right and left testicular longitudinal axis was 4.13 cm and 3.96 cm respectively. The mean serum levels of testosterone and FSH was 384.81 ng/dl and 7.73 ng/dl respectively. All these data are shown in table (1). Maximum 4 ml 205.00 75 % 85 % 5.5 cm 5.0 cm 890 11.0 Mean ± Sd 2.8955 ± 0.5856 40.8710 ± 41.8926 33.2791 ± 20.9659 41.4302 ± 19.7987 4.1314 ± 1.0365 3.9667 ± 1.0321 384.81 ± 238.03 7.7333 ± 2.6853 exposure, there is a significant reduction of sperm concentration, sperm motility and percentage of normal sperm forms (p<0.001, p<0.001 and p=0.013 respectively) and insignificant reduction of semen volume (p=0.081). There were insignificant changes in the testicular longitudinal axis, serum level of total testosterone and FSH in correlation to the duration of exposure to benzene. All these data are shown in table (2). The criteria of abnormal semen parameters are significantly correlated to the duration of benzene exposure. With the increase in the duration of Table (2): Changes in semen parameters in correlation to duration of exposure and age of Gas Station workers participants Duration of benzene exposure Sperm concentration Sperm motility Normal sperm forms Semen volume Right testis longitudinal axis Pearson correlation - 0.446 - 0.412 - 0.267 - 0.187 0.148 P value 0.001** 0.001** 0.013* 0.081 0.337 0.171 0.188 -0.210 Total testosterone 0.199 Folicular Stimulating Hormone Significant at the 0. 05 level (2- tailed) – ** highly significant at the 0. 01 (2- tailed) 0.374 0.293 Left testis size longitudinal axis 322 EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 Using a cut-point of five years exposure, we found significant difference in sperm concentration (t=4.845, p<0.001) and sperm motility (t=-3.371, p=0.001) between workers with duration of exposure more than 5 years and those with duration of exposure less than 5 years (Figure 1&2) and insignificant difference in the percentage of normal sperm forms (t=-0.85, p=0.398) (Figure 2). With Hussein et al more duration of benzene exposure, (7 years), we found significant difference in sperm concentration (t=4.864, p<0.001), sperm motility (t=4.619, p<0.001) and percentage of normal sperm forms (t=-2.419, p=0.018) between workers with duration of exposure more than 7 years and those with duration of exposure less than 7 years (Figure 3&4). Figure 2: Relation between sperm motility and normal forms and duration of exposure 50 80 60 40 20 40 Percentage Sperm concetration Figure 1: Relation between sperm concentration and duration of exposure 30.75 30 20 10 77.63 29.45 0 46.79 Motility > 5 years exposure 40.46 44.84 0 < 5 years exposure > 5 years exposure Normal forms < 5 years exposure Figure 4: Re lation be twe e n spe rn motility and normal forms and duration of e xposure Percentage Sperm concetration Figure 3: Re lation be twe e n spe rn conce ntration and duration of e xposure 24.11 Motility > 7 ye ars e xposure < 7 ye ars e xposure > 7 ye ars e xposure 323 36.52 Normal forms < 7 ye ars e xposure EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 Hussein et al sperm vitality and motility in the exposed workers. The mean acrosin activity, gamma–glutamine transferase activity and lactate dehydrogenase-C4 relative activity in the exposed workers were lower, and the fructose concentration was higher than those in the control group. There were negative correlations between sperm vitality, sperm activity, acrosin activity or LDH-C4 relative activity and the working history.8 DISCUSSION: The role of specific environmental and occupational factors in health problems is incompletely elucidated. Various physical and chemical occupational agents have been shown to affect male reproductive function. Chemicals are proved to cause genital tract malformations, such as hypospadias, cryptorchidism, feminization, and altered sexual behavior and reduced fertility in both men and women. Occupational exposure to traffic pollution has been reported to reduce the semen quality.4 Previous studies have shown that on exposure to hydrcarbons, the sperm motion parameters (in the exposure group) such as linearity (LIN), straightness (STR), and the sperm count were decreased significantly, and the abnormality rate of viscidity, coagulation and sperm count were increased significantly as compared with the control group.9 (Tan et al., 2002). The reduced semen quality are coinciding with Xiao et al.(1999) and Kawaguchi et al.,(2004), who concluded that occupational exposure to hydrocarbons can affect the worker’s semen quality especially the sperm count and movement ability.10,11 Benzene has toxic effects on sperms either directly or by inducing hormonal changes. Testicular failure secondary to benzene exposure leads to increased serum level of FSH and may be associated with reduction of testicular volume. Indeed, benzene behaves as an endocrine disruptors.5 Benzene could reduce the sperm count, motility, and vitality, together with a reduced forward velocity and increased the percentage of the abnormal spermatic forms.6 It is suggested that all such effects are caused by androgen deprivation and all such changes were reversible within two weeks of withdrawal from further benzene exposure.6 Results of our study are consistent with these results. Animals exposed to benzene showed azoospermia which is maintained for 150 days of observation period. The libido and fertility of the treated animals were zero. The effects appear to be mediated through the testes.12 (Lohiya et al., 1999). In animal studies with Pathak et al. (2000), it has been demonstrated that administration of benzene chromatographic fraction of chloroform extract of the seeds of Carica papaya have been done on a dose regimen of 5 and 10 mg/animal/day, orally to male albino rats, resulted into a total suppression of cauda epididymal sperm motility coinciding with a decrease in sperm count, viability, and an increase The reduced semen quality as a result of benzene exposure observed in this study are in agreement with Wang et al., 2000, who found that exposure to low concentration of benzene could be correlated with the declined quality of semen in occupational workers.7 The same results also are in concordance with Xiao et al., 2001, who suggested that hydrocarbons could affect the sperm and the function of accessory gonads leading to decreased 324 EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 in percent of abnormal spermatozoa during 60-150 days observation period.13 Hussein et al In relation to the duration of exposure to benzene, the current results are in the same line with Xiao et al. (2001), who suggesting that prolonged exposure to benzene had resulted into a reduced sperm activity and motility.8 The reduced testicular size, which could be correlated to the changes in the serum FSH level, is consistent with the study of Watanabe and Qanuki (1999), which demonstrated that diesel engine exhaust depressed gonadotrophic hormones and inhibited spermatogenesis in rats. The same authors reported that the smaller testes will reduce the sperm output in adults, and could subsequently affect the fertility.14 Conclusion: This study provides good epidemiological evidence that occupational exposure to benzene could influence the male reproductive function, and it is inversely correlated to the semen quality with a substantial role in reducing the human fertility. Furthermore, the study demonstrates that the duration of exposure to benzene plays an important role in detrimental male reproductive toxicological effects. The recent results supporting the hypothesis found by Elly Den et al. (2002), that there is a negative correlation between the biomarkers related to exposure to (PCAHS) and the sexual maturation. This may be explained as (PCAHS) behave as an endocrine disruptors, but their precise mechanism of action remains under investigation.2 Polychlorinated biphenyls interact with the receptors of sex steroid hormones, by which they may exert estrogenic, androgenic, or antiestrogenic effects.15 (Brouwer et al., 1995). Epidemiological studies produced evidences suggesting that environmental and occupational exposure to endocrine disruptors may explain the decreasing quality and quantity of human sperm (Swan et al., 1997),16 the increasing incidence of testicular cancer (Felming et al., 1999),17 and cryptorchidism (Weinder et al., 1998).18 REFERENCES: 1. Ahmad M.; Ahamed R.N.; Aladakatti R. H., and Ghosesawar M. G. (2002): Reversible anti-fertility effect of benzene extract of Ocimum sanctum leaves on sperm parameters and fructose content in rats. J. Basic Clin. Physiol. Pharmacol., 13(1):51-59. 2. benzene and lower quality of semen and very early fetal loss. Zhonghua Ya Fang Yi Xue Za Zhi., 34 (5): 271- 273 (English abstract). 3. Brouwer A.; Ahlborg U. G.; Vandenberg M., and Birbaum L. S. (1995): Functional aspects of development toxicity of polyhalo-genated aromatic- hydrocarbons in experimental animals and human infants. Eur. J. Pharmacol. Environ. Toxicol. Pharmacol., 293: 140. 4. Carlsen E.; Giwercmam A.; Keiding N.; and Shakkebaek N. E. (1992): Evidence of decreasing quality of semen during past 50 years. Br. Med. J., 305: 609613. 5. Elly Den H.; Harry A.; Karel H.; Tim N., and Lutgorade T. (2002): Sexual maturation in relation to Polychlorinated Aromatic Hydro- There is a body of evidences linking the duration of exposure to benzene and the reduced serum testosterone level. Epidemiological studies produced evidences suggesting that endocrine disruptors may explain the decreasing quality and quantity of the human sperm (Carlsen et al., 1992).19 325 EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 carbons: Sharpe and Shakkebaek,s Hypothesis Revisted. Environmental Health Perspectives, 110 (8):1-15. 6. Felming L.E.; Bean J. A.; Ruddolph M., and Hamilton K. (1999): Cancer inscidence in a cohort of licensed pesticide applicators in Florida. J. Occup. Environ. Med., 41: 279288. 7. Kawaguchi T.; Kawachi M.; Morikawa M.; Kazuta H., and Shibata K. (2004): Key parameters of sperm motion in relation to male fertility in rats given alpha- chlorohydrin or nitrobenzene. J. Toxicol. Sci., 29 (3): 217-231. 8. Lohiya N.K.; Mishra P. K.; Pathak N.; Manivannan B., and Jain S. C. (1999): Reversible azoospermia by oral administration of the benzene chromatographic fraction of the chloroform extract of Carica papaya in rabbits. Adv. Contracept., 15 (2):141161. 9. Michele D.R.; Stefano Z.; Luigi P.; Umberto C.; Bartolomeo B.(2003): Traffic pollutants affect fertility in men. European Society Of Human Reproduction and Embryology, 18 (5):1055-1061. 10. Pathak N.; Mishra P. K.; Manivannan B., and Lohiya N. K. (2000): Sterility due to inhibition of sperm motility by oral administration of benzene chromatographic fraction of the chloroform extract of the seeds of Carica papaya in rats. Phytomedicine, 7 (4): 325-333. 11. Safe S. (2000): Endocrine disruptors and human health is there a problem? An update. Environ. Health Perspect., 108: 487493. 12. Staessen J. A.; Nawrot T.; Den Hond E., and Thijs L. (2001): Renal function, cytogenetic measurements and sexual development in adolescents in relation to common environmental pollutants. Lancet, 357: 16601669. Hussein et al 13. Swan S. H.; Elkin E. P., and Fenster L. (1997): Have sperm densities declined? A reanalysis of global trend data. Envir. Health Perspect., 105 : 12281232. 14. Tan L. F.; Wang S. L.; Sun X. Z.; Li Y. N.; Wang Q. L., and Ji J. M. (2002): Effects of fenvalerate exposure on the semen quality of occupational workers. Zhonghua Nan Ke Xue., 8 (4):273-276 ( English abstract). 15. Tas S.; Lauwerys R., and Lison D. (1996): Ocuupational hazards for the male reproductive system. Crit. Rev. Toxicol.,26 (3): 261-307. 16. Wang S.; Chen H., and Wang X. (2000): Studies on relationship between exposure to low concentration of mixed 17. Watanabe N., and Qonuki Y. (1999): Inhalation of diesel engine exhaust effects on spermatogenesis in growing male rats. Environ. Health Perspect., 107: 539-544. 18. Weinder T. K.; Moller H.; Jensen T. K., and Shakkebaek N. E. (1998): Cryptorchidism and hypospadias in sons of gardeners and farmers. Environ. Health Perspect., 106: 793796. 19. World Health Organization (1999): Laboratory Manual for the Examination of Human Semen and Sperm Cervical Mucous Interaction.4th. edition, Cambridge University Press, Cambridge. 20. Xaio G.; Pan C.; Cai Y.; Lin H., and Fu Z. (2001): Effect of benzene, toluene, xylene on the semen quality and the function of accessory gonad of exposed workers. Ind. Health, 39 (2): 206-210. 21. Xiao G.; Pan C.; Cai Y.; Lin H., and Fu Z. (1999): Effect of benzene, toluene, xylene on the semen quality of exposed workers. Chin. Med. J. (Engl.), 112 (8): 709-712. 326 Hussein et al EL-MINIA MED., BULL., VOL. 19, NO. 2, JUNE, 2008 األيمن فتحي حسين -ممدوح محمد أبو النصر -منال عبد العزيز* قسم المسالك البولية -قسم الطب الشرعي* كلية طب المنيا أجريتتتذ تتترا ة لرةيتتتا اريتتتيب ة اتتتتر ة يتتتلقيا ة إلتاجتتتا للتتت ة رتتتلر ة إلجتقيتتتا لرجتتتت ة معرضتتيم ميإليتتت لقإلت يم هتتد لمليتتب لةلت م .تتتذ ة قإلت يم قتتل ةمتتاملذ ة لرةيتتا للت 88 ر ك قعل ةياقعتل ج ل أيا أمرةض لض يا أ اإلتيتليا ذتر ك اتب ةيتاقعتل لتمال مم ة رجت ة متتللإليم أ ة تتريم ياإلتتت م أع لرتتترةذ قيتتا متتم ةجتت اإلمتتي ة رتتلر ة اإلتيتتليا أ ا.يتتيم ة ظتتت ا ة إلجتقيتتا قتتل اتتب اجميتتت ليإلتتتذ ة يتتت ة مإل ت ع لرةيتتا لتتلل .رذيتتا ة .ي ةإلتتتذ ة مإل يا ذميا ة يتت ة مإلت ع – ذتر ك إليتقا ة .ي ةإلتتذ ة مإل يتا ة ممت ا – ذمتت اتب اجميتت ليإلتذ ة لب ر ك ريتس ميا ى رم م ة اييا ياير م ذر ك ة يرمت م ة مإلمت للصتيايم ة رع ياب ةهرة ق ةي ا ة غل ة إللتميا ذمت ةمتاملذ ة لرةيتا للت قيتيتتذ .جتب ة لصتيايم ةيتامرذ ة لرةيتا متل ق ةي ا جيت ةال رذيل ميار ق.يث اب قيتس ذت لصتيا للت .تل يإلا ذتملا قل أيفرذ إلات ج رة ة ق.ث لم أم إلتك ال رة مل .ظت هد ة رلر لل ة لصتت لإلتتل تتاالر ة رجتتت ةعذاتتر اعرضتتت لقإلت يم هتتد ظيفتتايب لةلت م .تتتذ ة قإلت يم -ذتتتم تترة ة اتتل ر مل .ظتتت هتتد إلرتتح لتتلل .رذيتتا ة .ي ةإلتتتذ ة مإل يتتا ذتتر ك يتتتل لتتلل ة .ي ةإلتتتذ ة مإل يا ة مم ا -ذمت أاقاذ ترا ة لرةيتا أم إلتتك إلرتح هتد ميتا ى رمت م ة اييا يتاير م قت لب ذرة صغر هد .جب ة لصيايم ذتإلذ را ة اغييرةذ ا لةل ق يتل مل ة اعرض لقإل يم متتت يتتتل هاتتر ة اعتترض لقإل ت يم و ت لمتتس يتتإل ةذ ياتتةار هر ت لتتلل .رذيتتا ة .ي ةإلتتتذ ة مإل يا -ذم لإلل ة ليتل هار ة اعرض و يقت يإل ةذ هتإله قت ضتها و مت يقق هتإلته إلتتك إلرح هد ذميا ة يت ة مإل ع للل ة .ي ةإلتذ ة مإل يا ة قيعيا مم رة ة ق.ث إلياللح أم ة عمت هد م .تذ ة قإل يم ةذار اعرضتت تإلرح ة رتلر ة إلجتقيتا ةعمر ة رع ييا ج .متيايب قما ة رق 327