Role of the cell growth suppressor p27 during vascular remodelling
advertisement

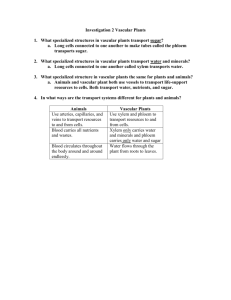
Role of the growth suppressor p27Kip1 during vascular remodeling Antonio Díez-Juan, Claudia Castro, M. D. Edo and Vicente Andrés* Laboratory of Vascular Biology, Department of Molecular and Cellular Pathology and Therapy, Instituto de Biomedicina de Valencia (IBV-CSIC), Spanish Council for Scientific Research, Valencia, Spain. * Corresponding author: Tel: 96-3391752 FAX: 96-3690800 E-mail: vandres@ibv.csic.es KEY WORDS: atherosclerosis, restenosis, neovascularization, proliferation, migration, p27Kip1 List of abbreviations: AngII, angiotensin II; apoE, apolipoprotein E; ASMC, aortic smooth muscle cell; bFGF, basic fibroblast growth factor; CDK, cyclin-dependent kinase; CKI, cyclin-dependent kinase inhibitor; EC, endothelial cell; ECM, extracellular matrix; ERK, extracellular signal-regulated kinase; FSMC, femoral artery smooth muscle cell; HUVEC, human vein endothelial cell; IMA, internal mammary artery; MAPK, mitogen-activated protein kinase; PDGF-BB, plateled-derived growth factor-BB; SV, saphenous vein; VSMC, vascular smooth muscle cell. 1 Abstract At homeostasis, vascular cells display a very low proliferative rate and scant migratory activity. However, hyperplastic growth and locomotion of vascular cells are a hallmark of vascular remodeling during several pathophysiological conditions (e. g., neovascularization, arteriosclerosis and restenosis post-angioplasty). Thus, a better understanding of the molecular mechanisms that control vascular cell proliferation and migration should facilitate the development of novel therapies to treat cardiovascular disease. In this review, we will discuss recent studies implicating the cell cycle regulatory protein p27Kip1 as a key modulator of vascular cell growth and locomotion in vitro and during vascular remodeling in vivo. 2 Introduction According to the response-to-injury hypothesis, atherosclerosis is triggered by different risk factors (i. e., hypercholesterolemia, aging, hypertension, smoking and diabetes) that cause endothelial dysfunction [1]. Studies in hypercholesterolemic animals and in human atherosclerotic specimens have identified three processes involved in the formation of the atherosclerotic plaque once the normal properties of the endothelium have been altered by the action of cardiovascular risk factors: 1) accumulation of lipid and mostly free and esterified cholesterol in the surrounding extracellular matrix (ECM) and the associated cells; 2) proliferation and migration of vascular cells within the injured arterial wall (Fig. (1)); and 3) formation of a connective tissue matrix comprising elastic fiber proteins, collagen and proteoglycans. Numerous observations suggest that vascular smooth muscle cells (VSMCs) in atherosclerotic lesions have changed from a contractile to a synthetic phenotype, in which they can respond to different growth factors and synthetize ECM components [2,3]. “Activated” VSMCs migrate toward the arterial lumen and express abundant levels of novel matrix components and proteases that modify the surrounding ECM. It is accepted that this “growth and synthetic” response of VSMCs contributes to neointimal lesion development during atherogenesis. Excessive VSMC proliferation and migration also contribute to restenosis postangioplasty (Fig. (2)), the recurrence of arterial narrowing at the site of revascularization that occurs in 20-40% of coronary artery disease patients after successful angioplasty [4-6]. Acute mechanical disruption of the protective endothelial lining at the site of angioplasty appears to trigger this aggressive form of vascular obstructive disease. Although arterial cell proliferation occurs in animal models during all phases of atherogenesis [1,7-9], studies with hyperlipidemic rabbits have shown an inverse correlation between atheroma size and cellular proliferation within the atheromatous 3 plaque [10-12]. Consistent with the response-to-injury hypothesis [1], medial cell proliferation at early stages of atherogenesis in fat-fed rabbits increased as a function of intimal lesion size [1,7-9]. Experimental angioplasty is also characterized by abundant proliferation of VSMCs (Fig. (2)), followed by the reestablishment of the quiescent phenotype typically within 2-4 weeks [4-6]. These animal studies suggest that vascular cell proliferation prevails at the onset of atherogenesis and restenosis. Expression of a variety of proliferation markers in human primary atheroma and restenotic lesions has been well documented [13-22]. However, controversy exists regarding the magnitude of the proliferative response during human atherosclerosis and restenosis, ranging from a very low index of cell proliferation [14,15,17,19,21] to abundance of dividing cells [16,23]. Aside from methodological issues (e. g., differences in the fixatives used for tissue preservation, antigen accessibility, analysis of different proliferation markers), some of the reported variance with regard to the issue of cell proliferation might relate to differences in the arteries being analyzed (e. g., peripheral, coronary and carotid arteries) and variance in the stage of atherogenesis at the time of tissue harvesting [24]. Proliferating cells within human atherosclerotic tissue include VSMCs, leukocytes and endothelial cells (ECs) [13-15,17-19,21]. Histological examination in 20 patients undergoing antemorten coronary angioplasty revealed that the extent of intimal proliferation was significantly greater in lesions with evidence of medial or adventitial tears than in lesions with no or only intimal tears [25]. Regarding the relative magnitude of intimal and medial cell proliferation, analysis of human carotid plaques revealed more proliferative activity in the intimal lesion versus the underlying media [19]. This study also disclosed differential distribution of proliferating cells in the intima versus the media; while the prevailing proliferative cell type in the intima was the monocyte/macrophage 4 (46% versus 9.7% -actin immunoreactive VSMCs, 14.3% ECs, 13.1% T lymphocytes), VSMCs were the preponderant proliferating cell type in the media (44.4% versus 20% ECs, 13.0% monocyte/macrophages, and 14.3% T lymphocytes). It is noteworthy that studies in human peripheral and coronary lesions have suggested more prominent proliferation in restenotic compared to primary lesions [17,23]. Moreover, cultured VSMCs from human advanced primary stenosing disclosed lower proliferative capacity than cells from fresh restenosing lesions [26]. Thus, similar to the situation in animal models, proliferation during human atherosclerosis and restenosis might peak at the onset of these pathologies and then progressively decline. Molecular control of cell proliferation in mammalian cells Mammalian cell cycle progression requires the activation of cyclin-dependent kinases (CDKs) through their association with regulatory subunits called cyclins [27]. Different CDK/cyclin holoenzymes are orderly activated at specific phases of the cell cycle. Active CDK/cyclin complexes are presumed to hyperphosphorylate the retinoblastoma gene product and the related pocket proteins p107 and p130 from mid G1 to mitosis. VSMC proliferation in the balloon-injured rat carotid artery is associated with a temporally and spatially coordinated expression of CDK2 and its regulatory subunits, cyclin E and cyclin A [22]. Induction of these factors correlated with increased CDK2-, cyclin E- and cyclin A-dependent kinase activity, indicating that functional CDK2/cyclin E and CDK2/cyclin A holoenzymes are assembled in the injured arterial wall. Expression of CDK2 and cyclin E was also detected in VSMCs within human atherosclerotic and restenotic tissue [16,22,28]. CDK activity is negatively regulated by the interaction with specific CDK inhibitory proteins (CKIs) [29]. CKIs of the Cip/Kip family (for CDK interacting protein/Kinase 5 inhibitory protein) (p21Cip1, p27Kip1 and p57Kip2) bind to an inhibit a wide spectrum of CDK/cyclin holoenzymes, while members of the Ink4 family (for inhibitor of CDK4) (p16Ink4a, p15Ink4b, p18Ink4c, p19Ink4d) are specific for cyclin D-associated kinase activity (CDK4 and CDK6). In the next sections, we will discuss in vitro and in vivo studies that implicate p27Kip1 as an important regulator of restenosis and atherosclerosis. Coordinate control of cell proliferation and migration by p27Kip1. Aside from its well established growth suppressive function, recent studies suggest a role for p27Kip1 as a negative regulator of cell migration. First, we have shown that overexpression of p27Kip1 can reduce human vein endothelial cell (HUVEC) and rabbit aorta VSMC migration in culture, and impair angiogenesis in vivo [30,31]. Second, p27Kip1-null VSMCs were more resistant than wild-type cells to the antimigratory properties of rapamycin [32], a bacterial macrolide that attenuates experimental restenosis [33] and has shown promising results in preventing human in-stent restenosis [34]. In view of these results, we investigated whether the dual function of p27Kip1 as a cell-cycle and migration inhibitor is achieved via common or independent molecular pathways (DíezJuan and Andrés, unpublished work - submitted for publication). Using retroviral vectors, we found that physiologically high level of p27Kip1 expression inhibits CDK activity and attenuates both proliferation and migration of VSMCs and fibroblasts. Mutations that rendered p27Kip1 unable to abrogate CDK activity also prevented p27Kip1-induced growth arrest and migration blockade. Collectively, these findings suggest that p27Kip1 coordinately modulates cell proliferation and locomotion via regulation of CDK activity (Fig. (3)). It is noteworthy that the related Cip/Kip protein p21Cip1, which reduced neointimal thickening in normocholesterolemic [35,36] and hypercholesterolemic animals [37], also inhibited VSMC migration in vitro [38]. Thus, p21Cip1 and p27Kip1 might attenuate neointimal growth by blocking both cell proliferation and chemotaxis. 6 Role of p27Kip1 in establishing regional phenotypic variance in VSMCs from different vascular beds Internal mammary artery (IMA) bypass grafts have a higher patency than saphenous vein (SV) grafts. Yang et al. investigated the growth properties of human VSMCs isolated from IMA and SV [39]. Cell outgrowth from explants over a 20-day period and seruminduced increase in cell number over an 8-day period were more pronounced in SV than in IMA of the same patient. Both types of VSMCs displayed functional growth factor receptor expression and activation of the mitogen-activated protein kinase (MAPK) pathway. Interestingly, platelet-derived growth factor-BB (PDGF-BB) markedly downregulated p27Kip1 protein level in SV, but this was much less pronounced in IMA. Thus, sustained p27Kip1 expression in spite of growth stimuli may contribute to the resistance to growth of VSMCs from IMA and to the longer patency of arterial versus venous grafts. While basic fibroblast growth factor (bFGF or FGF2) is a potent stimulator of medial VSMC proliferation after balloon angioplasty [40-42], neutralizing antibodies to FGF2 failed to inhibit intimal VSMC proliferation after balloon angioplasty [43], and only a small increase in proliferation was seen when bFGF was added to arteries with existing intimal lesions [40,42]. Attenuated bFGF-dependent proliferation of intimal VSMCs occurred despite a robust activation of the MAPK/extracellular signal-regulated kinase (ERK) pathway and induction of positive cell cycle regulators (e. g., cyclin D, cyclin E, CDK2 and CDK4) [42]. Interestingly, intimal VSMCs expressed high levels of p15 Ink4b and p27Kip1 compared with medial VSMCs, and bFGF infusion did not reduce the level of these inhibitors in arteries with established intimal lesions. Collectively, these studies suggest that high level of expression of p15Ink4b and p27Kip1 can attenuate VSMC 7 proliferation in cultures displaying MAPK activation and expression of positive cell cycle regulators. We have investigated whether VSMCs from vessels with different atherogenicity exhibit distinct growth and migratory potential, and investigated the underlying mechanisms [31]. We found increased cell proliferation and atheroma formation in the aortic arch versus the femoral artery of fat-fed rabbits. When examined in culture, VSMCs isolated from the aortic arch (ASMCs) displayed a greater capacity for inducible proliferation and migration than paired cultures of VSMCs isolated from the femoral artery (FSMCs). Two lines of evidence suggested that distinct regulation of p27Kip1 contributes to establishing these phenotypic dissimilarities. First, p27Kip1 expression was comparably lower in ASMCs. Importantly, ASMCs exhibited a higher fraction of p27Kip1 phosphorylated on threonine 187 and ubiquitinated, two posttranslational modifications implicated in proteasome-dependent degradation of p27Kip1 [44]. Second, forced p27Kip1 overexpression in ASMCs impaired their proliferative and migratory potential. We found that PDGF-BB-dependent induction of the ERK pathway was comparably higher in ASMCs. Importantly, pharmacological inhibition of ERKs increased p27Kip1 expression and attenuated ASMC proliferation and migration. In contrast, forced ERK activation diminished p27Kip1 expression and markedly augmented FSMC proliferation and migration. These findings suggest that intrinsic differences in the regulation of MAPKs and p27Kip1 play an important role in creating variance in the proliferative and migratory capacity of VSMCs, which might in turn contribute to establishing regional variability in atherogenicity (Fig. (4)). Role of p27Kip1 as a regulator of the phenotypic response of VSMCs to mitogenic and hypertrophic stimuli. 8 VSMC hypertrophy is associated with cardiovascular disease in the elderly and in hypertensive patients. Angiotensin II (Ang II) stimulates hypertrophy but not hyperplasia of quiescent VSMCs in serum-free media, in spite of increased expression of several protooncogenes and autocrine growth factors [45-48]. Braun-Dullaeus et al. reported that while both serum and Ang II treatment of quiescent VSMCs led to upregulation of positive cell-cycle regulators (e. g., proliferating cell nuclear antigen, cyclin D1, CDK2 and CDC2), only serum-treated VSMCs induced CDK2 and CDC2 activity [49]. These authors provided compelling evidence implicating p27Kip1 as a molecular switch that regulates the phenotypic response of VSMCs to mitogenic and hypertrophic stimuli. Indeed, Ang II-induced hypertrophy of quiescent VSMCs correlated with sustained expression of p27Kip1, unlike serum-dependent cell-cycle reentry of starvationsynchronized cells, which correlated with a marked downregulation of p27Kip1 protein level. Importantly, forced overexpression of p27Kip1 inhibited serum-stimulated proliferation and induced VSMC hypertrophy. Moreover, p27Kip1 inactivation increased [3H]-thymidine incorporation and the percentage of S-phase cells in Ang II-treated VSMC cultures. These results demonstrate that Ang II treatment of quiescent VSMCs is associated with cell-cycle entry, but hypertrophic rather than hyperplastic growth may prevail by the failure of cells to downregulate p27Kip1. In another study, Servant et al. compared the effects of Ang II and PDGF-BB on cultured VSMCs [50]. While both factors stimulated the accumulation of G1 cyclins and CDKs, only PDGF-BB activated CDK2 in late G1. Lack of CDK2 activity in Ang II-treated cells correlated with sustained p27Kip1 protein level. In contrast, PDGF-BB downregulated p27Kip1 expression due to a reduced rate of synthesis and an increased rate of protein degradation. Moreover, PDGFBB-dependent downregulation of p27Kip1 synthesis correlated with diminished p27Kip1 gene transcription and decreased mRNA accumulation. Collectively, these studies identify 9 p27Kip1 as an important regulator of the phenotypic response of VSMCs to mitogenic and hypertrophic stimuli. Role of p27Kip1 in the control of VSMC growth by extracellular matrix components. Specific ECM components and integrins have been implicated in cell cycle control during atherosclerosis and restenosis [51]. VSMCs within atherosclerotic lesions synthesize novel ECM components and induce the expression of matrix-degrading proteases that remodel the surrounding ECM. For example, matrix-degrading metalloproteinase expression is induced within atherosclerotic plaques and after balloon angioplasty [52-55]. Moreover, metalloproteinase inhibitors repressed VSMC proliferation in vitro and after angioplasty in vivo [56-58]. Accordingly, these ECM enzymes have been implicated in the induction of neointimal VSMC hyperplasia during atherosclerosis and restenosis. Several animal models of atherosclerosis and angioplasty have demonstrated significant changes in collagen content within the arterial wall [59-61]. To investigate whether these alterations may regulate VSMC proliferation, Koyama et al. studied the growth properties of VSMCs cultured on monomer collagen fibers and on polymerized collagen [62]. The rationale for these studies is that polymerized collagen may resemble the scenario of a normal artery composed of quiescent VSMCs, and monomer collagen might mimic the ECM surrounding proliferating VSMCs within atherosclerotic and restenotic plaques. Consistent with this notion, mitogen-stimulated VSMCs proliferated when grown on monomer collagen, but were arrested in G1 when seeded on polymerized collagen. The inhibitory effect of polymerized collagen on VSMC growth appeared to be mediated by 2 integrins, and was associated with suppression of p70S6K and upregulation of p27Kip1 (and to a lesser extent induction of the related protein p21Cip1). Thus, regulation 10 of CKIs in response to changes in specific ECM components might regulate the ability of VSMCs to respond to growth signals in vitro. Interestingly, the quiescent phenotype of nonadherent NRK fibroblasts correlated with an increased association of p27Kip1 and p21Cip1 to cyclin E-containing holoenzymes [63]. Further studies are required to determine whether cell cycle control in the arterial wall is linked in vivo to integrins and ECM components through changes in CKI expression. p27Kip1 and neovascularization De novo vessel formation (neovascularization) plays a critical role during physiological and pathological processes. Several studies have demonstrated the presence of microvessels within human atherosclerotic plaques [64-67]. Arteries with higher degree of stenosis and more predisposition to plaque rupture displayed more neovascularization within the intima [68]. Moreover, microvessels appeared absent in 97% of human coronary atheromas displaying an intima-to-media ratio less than 0.54, whereas 98% of arteries with larger lesions (intima-to-media ratio higher than 0.54) disclosed evidence of neovascularization [67]. Importantly, the angiogenesis inhibitors endostatin and TNP-470 significantly reduced atheroma growth in a murine model of atherosclerosis [69]. Collectively, these studies suggest that neovascularization of the atherosclerotic plaque plays an important role during experimental and human atherosclerosis. Neovascularization requires ECM remodeling and abundant cell proliferation and migration. We have demonstrated that ectopic overexpression of p27Kip1 inhibits both proliferation and migration of VSMCs and HUVECs [30,31] (also Díez-Juan and Andrés, unpublished work - submitted for publication). Moreover, p27Kip1 overexpression inhibited the formation of tube-like structures by HUVECs growing on Matrigel substrate, and impaired neovascularization in a murine model of ischemia-induced neovascularization [30]. 11 p27Kip1 and restenosis Balloon angioplasty in rat and porcine arteries resulted in the induction of p27Kip1 in VSMCs at late time points that correlated with reduced CDK2 activity and the decline in VSMC proliferation [20,70]. Moreover, overexpression of p27Kip1 efficiently blocked mitogen- and c-fos-dependent induction of cyclin A promoter activity in cultured VSMCs [70,71]. Thus, upregulation of p27Kip1 may contribute to the reestablishment of the quiescent phenotype that normally occurs at late time points after angioplasty. In agreement with this hypothesis, we have shown that local delivery of adenovirus encoding for p27Kip1 reduced neointimal hyperplasia in the rat carotid artery when applied at the time of angioplasty [70]. Likewise, adenovirus-mediated overexpression of p27Kip1 attenuated neointimal thickening in a porcine model of balloon angioplasty [72]. Of note in this regard, chimaeric p27Kip1p16Ink4a proteins appear to have a more potent antiproliferative activity than p27Kip1 and p16Ink4a [73]. p27Kip1 and arteriosclerosis We have recently established a causal relationship between p27Kip1 and atherosclerosis in apolipoprotein E (apoE)-null mice [8]. p27Kip1–deficient mice challenged with a high-fat diet for 1 month remained normocholesterolemic and had essentially no visible atheromas. However, when generated in an apoE-null genetic background that leads to severe hypercholesterolemia in response to the atherogenic diet, deletion of p27Kip1 enhanced arterial cell proliferation (~4-fold) and accelerated atherogenesis (~6-fold) as compared to apoE-deficient mice with an intact p27Kip1 gene. Analysis of apoE-null mice bearing only one p27Kip1 allele inactivated revealed that a moderate decrease in p27Kip1 protein expression in the setting of hypercholesterolemia is sufficient to predispose to atherogenesis. These studies establish a molecular link between diminished p27Kip1 protein 12 expression and atherogenesis in hypercholesterolemic animals. Regarding human atherogenesis, Tanner et al. reported abundant p27Kip1 expression in nonproliferating VSMCs and macrophages within coronary arteries ranging from normal to advanced atherosclerosis, suggesting an inverse correlation between arterial cell proliferation and expression of p27Kip1 [20]. Moreover, TGF- present in human atherosclerotic tissue might mediate its growth suppressive activity through p27Kip1-dependent blockade of cyclin ECDK2 activity [28]. It is noteworthy that inactivation of either p27Kip1 [8] or p53 [74] by itself is not sufficient to promote atherosclerosis in mice challenged with an atherogenic diet for 4-10 weeks. Importantly, fat-fed p27Kip1- and p53-null mice remained normocholesterolemic at the end of the experimental protocol. However, when generated in an apoE-null genetic background that leads to severe hypercholesterolemia in response to the atherogenic diet, ablation of either p27Kip1 or p53 accelerated the underlying atherogenic process triggered by hypercholesterolemia. These findings support the notion that excessive vascular cell proliferation is subsidiary to injury to the vessel wall initiated by atherogenic stimuli (i. e., hypercholesterolemia) rather than the cause of this process [1]. Another example of a synergistic pathological response involving p27Kip1 concerns tumor development. Indeed, spontaneous tumorigenesis in p27Kip1-deficient mice appears limited to pituitary adenomas [75-77]. However, when challenged with tumorigenic agents (e. g., chemical carcinogens or ionizing radiation), p27Kip1-null mice displayed increased tumor predisposition in multiple tissues [78]. These studies suggest that p27Kip1 safeguards against the hyperproliferative response triggered by a variety of pathological stimuli. Hence, future studies in animal models and human tissue should thoroughly investigate the temporal and spatial pattern of expression of p27Kip1 during atherogenesis, and elucidate molecular mechanisms underlying the regulation of p27Kip1 expression in vascular cells. Such 13 information would find application not only in vascular proliferative diseases, but also in human neoplastic disorders in which tumor progression and patient mortality might be associated with reduced p27Kip1 expression [44]. Acknowledgements This work is dedicated to the memory of Dr. Jeffrey M. Isner, whose intellectual stimulation was enjoyed by all who were fortunate to work with him. Work in the laboratory of V. Andrés is supported by the Spanish Ministry of Science and Technology and Fondo Europeo de Desarrollo Regional (FEDER) (grants SAF2001-2358 and SAF2002-1443) and by Generalitat Valenciana (grants GV01-488 and CTGCA/2002/04). C. Castro and M. D. Edo are recipients of a fellowship from Agencia Española de Cooperación Internacional and Generalitat Valenciana, respectively. A. Díez-Juan was partially supported from the Spanish DGESIC and FEDER (grant 1FD97-1035-C02-02), and from Fondo Social Europeo (CSIC-Programa I3P fellowship). 14 References [1]. Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med 1999; 340: 11526. [2]. Owens GK. Regulation of differentiation of vascular smooth muscle cells. Physiol Rev 1995; 75: 487-517. [3]. Thyberg J. Phenotypic modulation of smooth muscle cells during formation of neointimal thickening following vascular injury. Histol Histopathol 1998; 13: 871-91. [4]. Bauters C, Isner JM. The biology of restenosis. Prog Cardiovasc Dis 1997; 40: 107-16. [5]. Andrés V. Control of vascular smooth muscle cell growth and its implication in atherosclerosis and restenosis. Int J Molec Med 1998; 2: 81-9. [6]. Libby P, Tanaka H. The molecular basis of restenosis. Prog Cardiovasc Dis 1997; 40: 97-106. [7]. Cortés MJ, Díez-Juan A, Pérez P, Pérez-Roger I, Arroyo-Pellicer R, Andrés V. Increased early atherogenesis in young versus old hypercholesterolemic rabbits by a mechanism independent of arterial cell proliferation. FEBS Letters 2002; 522: 99-103. [8]. Díez-Juan A, Andrés V. The growth suppressor p27Kip1 protects against dietinduced atherosclerosis. FASEB J 2001; 15: 1989-95. [9]. Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993; 362: 801-9. [10]. Spraragen SC, Bond VP, Dahl LK. Role of hyperplasia in vascular lesions of cholesterol-fed rabbits studied with thymidine-3H autoradiography. Circ Res 1962; 11: 32936. 15 [11]. McMillan GC, Stary HC. Preliminary experience with mitotic activity of cellular elements in the atherosclerotic plaques of cholesterol-fed rabbits studied by labeling with tritiated thymidine. Ann N Y Acad Sci 1968; 149: 699-709. [12]. Rosenfeld ME, Ross R. Macrophage and smooth muscle cell proliferation in atherosclerotic lesions of WHHL and comparably hypercholesterolemic fat-fed rabbits. Arteriosclerosis 1990; 10: 680-7. [13]. Burrig KF. The endothelium of advanced arteriosclerotic plaques in humans. Arterioscler Thromb 1991; 11: 1678-89. [14]. Gordon D, Reidy MA, Benditt EP, Schwartz SM. Cell proliferation in human coronary arteries. Proc Natl Acad Sci U S A 1990; 87: 4600-4. [15]. Katsuda S, Coltrera MD, Ross R, Gown AM. Human atherosclerosis. IV. Immunocytochemical analysis of cell activation and proliferation in lesions of young adults. Am J Pathol 1993; 142: 1787-93. [16]. Kearney M, Pieczek A, Haley L, Losordo DW, Andrés V, Schainfield R, et al. Histopathology of in-stent restenosis in patients with peripheral artery disease. Circulation 1997; 95: 1998-2002. [17]. O'Brien ER, Alpers CE, Stewart DK, Ferguson M, Tran N, Gordon D, et al. Proliferation in primary and restenotic coronary atherectomy tissue. Implications for antiproliferative therapy. Circ Res 1993; 73: 223-31. [18]. Orekhov AN, Andreeva ER, Mikhailova IA, Gordon D. Cell proliferation in normal and atherosclerotic human aorta: proliferative splash in lipid-rich lesions. Atherosclerosis 1998; 139: 41-8. [19]. Rekhter MD, Gordon D. Active proliferation of different cell types, including lymphocytes, in human atherosclerotic plaques. Am J Pathol 1995; 147: 668-77. 16 [20]. Tanner FC, Yang Z-Y, Duckers E, Gordon D, Nabel GJ, Nabel EG. Expression of cyclin-dependent kinase inhibitors in vascular disease. Circ Res 1998; 82: 396-403. [21]. Veinot JP, Ma X, Jelley J, O'Brien ER. Preliminary clinical experience with the pullback atherectomy catheter and the study of proliferation in coronary plaques. Can J Cardiol 1998; 14: 1457-63. [22]. Wei GL, Krasinski K, Kearney M, Isner JM, Walsh K, Andrés V. Temporally and spatially coordinated expression of cell cycle regulatory factors after angioplasty. Circ Res 1997; 80: 418-26. [23]. Pickering JG, Weir L, Jekanowski J, Kearney MA, Isner JM. Proliferative activity in peripheral and coronary atherosclerotic plaque among patients undergoing percutaneous revascularization. J Clin Invest 1993; 91: 1469-80. [24]. Isner JM. Vascular remodeling. Honey, I think I shrunk the artery. Circulation 1994; 89: 2937-41. [25]. Nobuyoshi M, Kimura T, Ohishi H, Horiuchi H, Nosaka H, Hamasaki N, et al. Restenosis after percutaneous transluminal coronary angioplasty: pathologic observations in 20 patients. J Am Coll Cardiol 1991; 17: 433-9. [26]. Dartsch PC, Voisard R, Bauriedel G, Hofling B, Betz E. Growth characteristics and cytoskeletal organization of cultured smooth muscle cells from human primary stenosing and restenosing lesions. Arteriosclerosis 1990; 10: 62-75. [27]. Nurse P. Ordering S phase and M phase in the cell cycle. Cell 1994; 79: 547-50. [28]. Ihling C, Technau K, Gross V, Schulte-Monting J, Zeiher AM, Schaefer HE. Concordant upregulation of type II-TGF-beta-receptor, the cyclin- dependent kinases inhibitor p27Kip1 and cyclin E in human atherosclerotic tissue: implications for lesion cellularity. Atherosclerosis 1999; 144: 7-14. 17 [29]. Vidal A, Koff A. Cell-cycle inhibitors: three families united by a common cause. Gene 2000; 247: 1-15. [30]. Goukassian D, Díez-Juan A, Asahara T, Schratzberger P, Silver M, Murayama T, et al. Overexpression of p27Kip1 by doxycycline-regulated adenoviral vectors inhibits endothelial cell proliferation and migration and impairs angiogenesis. FASEB J 2001; 15: 1877-85. [31]. Castro C, Díez-Juan A, Cortés MJ, Andrés V. Distinct regulation of mitogenactivated protein kinases and p27Kip1 in smooth muscle cells from different vascular beds: A potential role in establishing regional phenotypic variance. J Biol Chem 2003; In Press. [32]. Sun J, Marx SO, Chen H-J, Poon M, Marks AR, Rabbani LE. Role for p27Kip1 in vascular smooth muscle cell migration. Circulation 2001; 103: 2967-72. [33]. Gallo R, Padurean A, Jayaraman T, Marx S, Rogue M, Adelman S, et al. Inhibition of intimal thickening after balloon angioplasty in porcine coronary arteries by targeting regulators of the cell cycle. Circulation 1999; 99: 2164-70. [34]. Sousa JE, Costa MA, Abizaid A, Abizaid AS, Feres F, Pinto IM, et al. Lack of neointimal proliferation after implantation of sirolimus-coated stents in human coronary arteries: a quantitative coronary angiography and three-dimensional intravascular ultrasound study. Circulation 2001; 103: 192-5. [35]. Chang MW, Barr E, Lu MM, Barton K, Leiden JM. Adenovirus-mediated overexpression of the cyclin/cyclin-dependent kinase inhibitor, p21 inhibits vascular smooth muscle cell proliferation and neointima formation in the rat carotid artery model of balloon angioplasty. J Clin Invest 1995; 96: 2260-8. [36]. Yang Z-Y, Simari RD, Perkins ND, San H, Gordon D, Nabel GJ, et al. Role of p21 cyclin-dependent kinase inhibitor in limiting intimal cell proliferation in response to arterial injury. Proc Natl Acad Sci USA 1996; 93: 7905-10. 18 [37]. Condorelli G, Aycock JK, Frati G, Napoli C. Mutated p21/WAF/CIP transgene overexpression reduces smooth muscle cell proliferation, macrophage deposition, oxidationsensitive mechanisms, and restenosis in hypercholesterolemic apolipoprotein E knockout mice. FASEB J 2001; 15: 2162-70. [38]. Fukui R, Shibata N, Kohbayashi E, Amakawa M, Furutama D, Hoshiga M, et al. Inhibition of smooth muscle cell migration by the p21 cyclin-dependent kinase inhibitor (Cip1). Atherosclerosis 1997; 132: 53-9. [39]. Yang Z, Oemar BS, Carrel T, Kipfer B, Julmy F, Lüscher TF. Different proliferative properties of smooth muscle cells of human arterial and venous bypass vessels: role of PDGF receptors, mitogen-activated protein kinase, and cyclin-dependent kinase inhibitors. Circulation 1998; 97: 181-7. [40]. Lindner V, Lappi DA, Baird A, Majack RA, Reidy MA. Role of basic fibroblast growth factor in vascular lesion formation. Circ Res 1991; 68: 106-13. [41]. Lindner V, Reidy MA. Proliferation of smooth muscle cells after vascular injury is inhibited by an antibody against basic fibroblast growth factor. Proc Natl Acad Sci USA 1991; 88: 3739-43. [42]. Olson NE, Kozlowski J, Reidy MA. Proliferation of intimal smooth muscle cells. Attenuation of basic fibroblast growth factor 2-stimulated proliferation is associated with increased expression of cell cycle inhibitors. J Biol Chem 2000; 275: 11270-7. [43]. Olson NE, Chao S, Lindner V, Reidy MA. Intimal smooth muscle cell proliferation after balloon catheter injury. The role of basic fibroblast growth factor. Am J Pathol 1992; 140: 1017-23. [44]. Philipp-Staheli J, Payne SR, Kemp CJ. p27Kip1: regulation and function of a haploinsufficient tumor suppressor and its misregulation in cancer. Exp Cell Res 2001; 264: 148-68. 19 [45]. Geisterfer AA, Peach MJ, Owens GK. Angiotensin II induces hypertrophy, not hyperplasia, of cultured rat aortic smooth muscle cells. Circ Res 1988; 62: 749-56. [46]. Gibbons GH, Pratt RE, Dzau VJ. Vascular smooth muscle cell hypertrophy vs. hyperplasia. Autocrine transforming growt factor-1 expression determines growth response to angiotensin II. J Clin Invest 1992; 90: 456-61. [47]. Naftilan AJ, Pratt RE, Dzau VJ. Induction of platelet-derived growth factor Achain and c-myc gene expression by angiotensin II in cultured rat vascular smooth muscle cells. J Clin Invest 1989; 83: 1419-24. [48]. Naftilan AJ, Gilliland GK, Eldridge CS, Kraft AS. Induction of the protooncogen c-jun by angiotensin II. Mol Cell Biol 1990; 10: 5536-40. [49]. Braun-Dullaeus RC, Mann MJ, Ziegler A, von der Leyen HE, Dzau VJ. A novel role for the cyclin-dependent kinase inhibitor p27Kip1 in angiotensin II-stimulated vascular smooth muscle cell hypertrophy. J Clin Invest 1999; 104: 815-23. [50]. Servant MJ, Coulombe P, Turgeon B, Meloche S. Differential regulation of p27Kip1 expression by mitogenic and hypertrophic factors: involvement of transcriptional and posttranscriptional mechanisms. J Cell Biol 2000; 148: 543-56. [51]. Assoian RK, Marcantonio EE. The extracellular matrix as a cell cycle control element in atherosclerosis and restenosis. J Clin Invest 1996; 98: 2436-9. [52]. Bendeck MP, Zempo N, Clowes AW, Gelardy RE, Reidy MA. Smooth muscle cell migration and matrix metalloproteinase expression after arterial injury in the rat. Circ Res 1994; 75: 539-45. [53]. Galis S, Sukhova GK, Lark MV, Libby P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest 1994; 94: 2493-503. 20 [54]. Zempo N, Kenagy RD, Au T, Bendeck M, Clowes MM, Reidy MA, et al. Matrix metalloproteinases of vascular wall cells are increased in balloon-injured rat carotid artery. J Vasc Surg 1994; 20: 209-17. [55]. Southgate KM, Fisher M, Banning AP, Thurston VJ, Baker AH, Fabunmi RP, et al. Upregulation of basement membrane-degrading metalloproteinase secretion after balloon injury of pig carotid artery. Circ Res 1996; 79: 1177-87. [56]. Southgate KM, Davies M, Booth RFG, Newby AC. Involvement of extracellular matrix degrading metalloproteinases in rabbit aortic smooth muscle cell proliferation. Biochem J 1992; 288: 93-9. [57]. Zempo N, Koyama M, Kenagy RD, Lea HJ, Clowes AW. Regulation of vascular smooth muscle cell migration and proliferation in vitro and in injured rat arteries by a synthetic matrix metalloproteinase inhibitor. Arterioscler Throm Vasc Biol 1996; 16: 28-33. [58]. Cheng L, Mantile G, Pauly R, Nater C, Felici A, Monticone R, et al. Adenovirus-mediated gene transfer of the human tissue inhibitor of metalloproteinase-2 blocks vascular smooth muscle cell invasiveness in vitro and modulates neointimal development in vivo. Circulation 1998; 98: 2195-201. [59]. Strauss BH, Chisholm RJ, Keeley FW, Gotlieb AI, Logan RA, Armstrong PW. Extracellular matrix remodeling after balloon angioplasty injury in a rabbit model of restenosis. Circ Res 1994; 75: 650-8. [60]. Karim MA, Miller DD, Farrar MA, Elefheriades E, Reddy BH, Brelan CM, et al. Histomorphometric and biochemical correlates of arterial procollagen gene expression during vascular repair after experimental angioplasty. Circulation 1995; 91: 2049-57. [61]. Coats WD, Jr., Whittaker P, Cheung DT, Currier JW, Han B, Faxon DP. Collagen content is significantly lower in restenotic versus nonrestenotic vessels after balloon angioplasty in the atherosclerotic rabbit model. Circulation 1997; 95: 1293-300. 21 [62]. Koyama H, Raines EW, Bornfeldt KE, Roberts JM, Ross R. Fibrillar collagen inhibits arterial smooth muscle proliferation through regulation of cdk2 inhibitors. Cell 1996; 87: 1069-78. [63]. Zhu X, Ohtsubo M, Böhmer RM, Roberts JM, Assoian RK. Adhesion-dependent cell cycle progression linked to the expression of cyclin D1, activation of cyclin E-cdk2, and phosphorylation of the retinoblastoma protein. J Cell Biol 1996; 133: 391-403. [64]. Barger AC, Beeuwkes R, 3rd, Lainey LL, Silverman KJ. Hypothesis: vasa vasorum and neovascularization of human coronary arteries. A possible role in the pathophysiology of atherosclerosis. N Engl J Med 1984; 310: 175-7. [65]. Kaartinen M, Penttila A, Kovanen PT. Mast cells accompany microvessels in human coronary atheromas: implications for intimal neovascularization and hemorrhage. Atherosclerosis 1996; 123: 123-31. [66]. Kumamoto M, Nakashima Y, Sueishi K. Intimal neovascularization in human coronary atherosclerosis: its origin and pathophysiological significance. Hum Pathol 1995; 26: 450-6. [67]. Zhang Y, Cliff WJ, Schoefl GI, Higgins G. Immunohistochemical study of intimal microvessels in coronary atherosclerosis. Am J Pathol 1993; 143: 164-72. [68]. Paterson JC. Capillary rupture with intimal hemorrhage as a causative factor in coronary thrombosis. Arch Pathol 1938; 25: 474-87. [69]. Moulton KS, Heller E, Konerding MA, Flynn E, Palinski W, Folkman J. Angiogenesis inhibitors endostatin or TNP-470 reduce intimal neovascularization and plaque growth in apolipoprotein E-deficient mice. Circulation 1999; 99: 1726-32. [70]. Chen D, Krasinski K, Chen D, Sylvester A, Chen J, Nisen PD, et al. Downregulation of cyclin-dependent kinase 2 activity and cyclin A promoter activity in 22 vascular smooth muscle cells by p27Kip1, an inhibitor of neointima formation in the rat carotid artery. J Clin Invest 1997; 99: 2334-41. [71]. Sylvester AM, Chen D, Krasinski K, Andrés V. Role of c-fos and E2F in the induction of cyclin A transcription and vascular smooth muscle cell proliferation. J Clin Invest 1998; 101: 940-8. [72]. Tanner FC, Boehm M, Akyürek LM, San H, Yang Z-Y, Tashiro J, et al. Differential effects of the cyclin-dependent kinase inhibitors p27Kip1, p21Cip1, and p16Ink4 on vascular smooth muscle cell proliferation. Circulation 2000; 101: 2022-5. [73]. Lamphere L, Tsui L, Wick S, Nakano T, Kilinski L, Finer M, et al. Novel chimeric p16 and p27 molecules with increased antiproliferative activity for vascular disease gene therapy. J Mol Med 2000; 78: 451-9. [74]. Guevara NV, Kim HS, Antonova EI, Chan L. The absence of p53 accelerates atherosclerosis by increasing cell proliferation in vivo. Nat Med 1999; 5: 335-9. [75]. Nakayama K, Ishida N, Shirane M, Inomata A, Inoue T, Shishido N, et al. Mice lacking p27Kip1 display increased body size, multiple organ hyperplasia, retinal dysplasia, and pituitary tumors. Cell 1996; 85: 707-20. [76]. Fero ML, Rivkin M, Tasch M, Porter P, Carow CE, Firpo E, et al. A syndrome of multiorgan hyperplasia with features of gigantism, tumorigenesis, and female sterility in p27Kip1-deficient mice. Cell 1996; 85: 733-44. [77]. Kiyokawa H, Kineman RD, Manova-Todovora KO, Soares VC, Hoffman ES, Ono M, et al. Enhanced growth of mice lacking the cyclin-dependent kinase inhibitor function of p27Kip1. Cell 1996; 85: 721-32. [78]. Fero ML, Randel E, Gurley KE, Roberts JM, Kemp CJ. The murine gene p27Kip1 is haplo-insufficient for tumour suppression. Nature 1998; 396: 177-80. 23 FIGURE LEGENDS FIGURE 1: Arterial cell proliferation in the aortic arch of fat-fed rabbits. Male New Zealand rabbits received either control chow or a high-cholesterol diet for 2 months [31]. Prior to sacrifice, animals were injected with BrdU to assess arterial cell proliferation. The photomicrographs show representative examples of cross-sections of the aortic arch of rabbits fed the cholesterol-rich or control diet. Specimens were counterstained with eosin. Arrowheads point to the internal elastic lamina. While cell proliferation was negligible in control arteries, abundant nuclear BrdU incorporation was detected in aortic tissue from fatfed rabbits, particularly in cells within the atheromatous lesion. FIGURE 2: Arterial cell proliferation after balloon angioplasty in the rat carotid artery. Angioplasty and BrdU in vivo labeling was performed as described [71]. The photomicrographs show representative cross-sections of control vessels (left) and 10 days after balloon angioplasty (right). Black and white arrowheads point to the internal and the external elastic lamina, respectively. Note abundant nuclear BrdU incorporation in ballooninjured arteries. FIGURE 3: Coordinate regulation of cell proliferation and migration by p27Kip1. High level of p27Kip1 expression in cultured VSMCs, ECs, and fibroblasts is associated with reduced cell proliferation and migration [30,31]. Mutations that rendered p27Kip1 unable to abrogate CDK activity prevented both growth arrest and migration blockade (Díez-Juan And Andrés, unpublished work – submitted for publication). These findings suggest that changes in p27Kip1 expression can modulate vascular cell proliferation and locomotion in a coordinated manner via regulation of CDK activity. FIGURE 4: Differential regulation of MAPKs and p27Kip1 is associated with distinct proliferative and migratory capacity of VSMCs isolated from vessels with 24 different atherogenicity. The schematic summarizes the phenotypic profile of rabbit VSMCs isolated from vessels that responded differently to a high-fat diet [31]. 25