Pediatric Intensive Care
advertisement

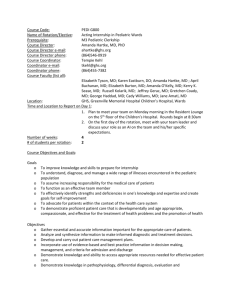
Pediatric Intensive Care (1 month) PGY-2 Rotation Description The resident will spend one month on the Pediatric Intensive Care Unit Service at the University of Kentucky Hospital. This rotation is part of a fully accredited Pediatric Residency Program. The resident will admit at least 15 patients to the Pediatric ICU and 30 patients will be seen during this rotation. The resident will be responsible for direct patient care under the supervision of the Faculty and Senior Level Residents of the Department of Pediatrics. The resident will have some supervisory responsibility over the nursing staff in the ICU. The resident will take call every third night. Goals 1. The resident is to gain knowledge and experience in the evaluative, cognitive, and procedural skills used in the care of the pediatric patient with acute severe illness is important to the practice of emergency medicine. 2. This rotation will foster the knowledge and experience base of the resident as well as provide insight into the practice style of pediatric colleagues. Competency Objectives 1. Following this rotation, the Resident will be able to assess the pediatric patient with acute, severe illness, to identify key problems and identify a differential diagnosis, diagnostic appraisal and therapeutic plan for each problem (PC, MK) 2. Following this rotation, the resident will have gained knowledge in causes of respiratory distress and failure in the pediatric patient, etiology, diagnosis, and treatment of fluid and electrolyte abnormalities seen in the pediatric ICU patient, evaluation and treatment of the pediatric patient with coma, evaluation and treatment of seizures and status epilepticus, classification, diagnosis, and management of pneumonia seen in the Pediatric ICU patient, identify common pathogens and initial treatment for the pediatric patient with meningitis, and understand the syndrome of occult bacteremia and sepsis in the pediatric patient. (MK) 3. Following this rotation, the resident will be able to perform endotracheal intubation on infants and children, perform venous and arterial blood sampling, perform lumbar puncture on infants and children, start intravenous catheters on infants and children, and central line placement in infants and children. (PC) 4. Initiate and execute the appropriate “time out” procedures with the health care team (SBP) 5. Demonstrate the ability to self reflect on learning deficiencies and develop a plan for improvement (PBLI) 6. Communicate essential information to other health care teams in order to enhance the quality of care (ICS) Description of Didactic Experiences There are weekly scheduled emergency medicine conferences (5 hours per week), which the residents attend, if possible. Core reading is assigned for self-study. In addition, the resident may attend conferences sponsored by the Department of Pediatrics. Evaluation Process The resident receives a verbal feedback and written evaluation from all Department of Pediatrics Faculty that have contact with that resident during the month. Feedback Mechanisms The resident receives verbal feedback from the individual Pediatric faculty as needed and the EM program director if required. The resident fills out a written evaluation of the rotation at the end of the month as well as a self-evaluation. New innovations will be utilized for evaluations.