Contraception Scenario 11_2_12
advertisement
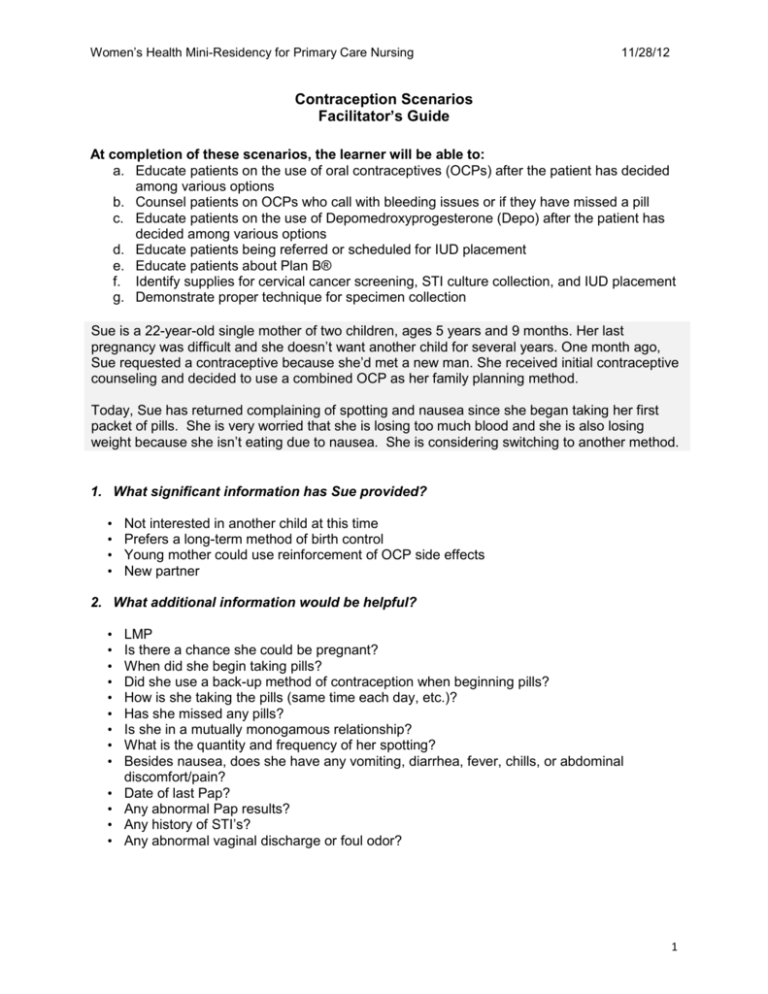
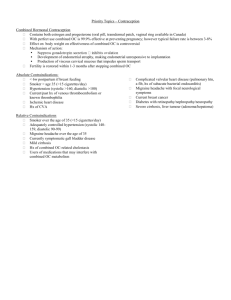
Women’s Health Mini-Residency for Primary Care Nursing 11/28/12 Contraception Scenarios Facilitator’s Guide At completion of these scenarios, the learner will be able to: a. Educate patients on the use of oral contraceptives (OCPs) after the patient has decided among various options b. Counsel patients on OCPs who call with bleeding issues or if they have missed a pill c. Educate patients on the use of Depomedroxyprogesterone (Depo) after the patient has decided among various options d. Educate patients being referred or scheduled for IUD placement e. Educate patients about Plan B® f. Identify supplies for cervical cancer screening, STI culture collection, and IUD placement g. Demonstrate proper technique for specimen collection Sue is a 22-year-old single mother of two children, ages 5 years and 9 months. Her last pregnancy was difficult and she doesn’t want another child for several years. One month ago, Sue requested a contraceptive because she’d met a new man. She received initial contraceptive counseling and decided to use a combined OCP as her family planning method. Today, Sue has returned complaining of spotting and nausea since she began taking her first packet of pills. She is very worried that she is losing too much blood and she is also losing weight because she isn’t eating due to nausea. She is considering switching to another method. 1. What significant information has Sue provided? • • • • Not interested in another child at this time Prefers a long-term method of birth control Young mother could use reinforcement of OCP side effects New partner 2. What additional information would be helpful? • • • • • • • • • • • • • LMP Is there a chance she could be pregnant? When did she begin taking pills? Did she use a back-up method of contraception when beginning pills? How is she taking the pills (same time each day, etc.)? Has she missed any pills? Is she in a mutually monogamous relationship? What is the quantity and frequency of her spotting? Besides nausea, does she have any vomiting, diarrhea, fever, chills, or abdominal discomfort/pain? Date of last Pap? Any abnormal Pap results? Any history of STI’s? Any abnormal vaginal discharge or foul odor? 1 Women’s Health Mini-Residency for Primary Care Nursing 11/28/12 As you query Sue’s contraception use, she informs you that although she started her OCPs right away after the first clinic visit, she didn’t use a backup method of birth control when initiating the prescription. She states, “I am really nervous it about?” Sue believes that her last Pap was “probably” at the first OB visit for her second child, which was approximately 18 months ago. Today, she admits to smoking one pack of cigarettes daily and drinking alcohol on occasion. 3. What would you tell Sue about Plan B®? • • • • • • • Available by prescription and over-the-counter For occasional use as emergency birth control; should not replace regular birth control method Prevents egg from fully developing; also prevents attachment of egg to uterine wall Plan B® tablets − Take one tablet as soon as possible not more than 120 hours (5 days) after unprotected sex or after failure of another birth control method. Most effective if taken within 24 hours. Take second tablet 12 hours after the first dose. Plan B® One-Step tablet − One tablet taken as soon as possible not more than 72 hours (3 days) after unprotected sex or after failure of another birth control method. Most effective if taken within 24 hours. If vomit within 2 hours of taking medicine, call your doctor right away. May need to prescribe another tablet for you. Common side effects: nausea, abdominal pain, fatigue, headache, menstrual changes You offer Sue the opportunity to empty her bladder and hand her a gown and sheet. 4. What tests might the provider perform? What supplies would you make available? Tests • Serum pregnancy test • Pelvic exam with STI cultures • Hepatitis B and C- RPR (for Hepatitis C and syphilis) • Hematocrit and hemoglobin (to rule out anemia) Supplies: • Gloves • Specula (Graves and Pederson) • Chlamydia and GC cultures, bacterial culture tube • KOH • Water-soluble lubricant • Large cotton-tipped swabs • Patient education handout 2 Women’s Health Mini-Residency for Primary Care Nursing 11/28/12 5. What is Sue at highest risk for and what education would you provide? • Pregnancy • STIs • Educate on testing and outcomes for each diagnosis 6. What education would you reinforce regarding oral contraceptives? • • • • • Proper initiation and side effects What to do when one or more pills are missed When to seek further care for vaginal bleeding Plan B Emergency Contraception Add barrier method for STI protection 7. What education would you reinforce regarding STIs? • Condom use is the only way to practice safe sex • Should have an HIV test at this time During the exam, Sue states that she’s “not very good at remembering daily medication”. 8. What contraceptive options are viable for a patient who voices concerns about her ability to comply? Why? • • • • Depo-Provera injection Nexplanon (Implanon) implant Mirena IUD ParaGard IUD Sue decides that she would like to have a Mirena IUD inserted. 9. What would you tell Sue about IUD placement? A. How should she prepare? • Taking ibuprofen one to two hours before the procedure can help reduce cramping. B. How is the procedure performed? • Provider will insert a speculum into the vagina. Vagina and cervix will be cleansed with an antiseptic solution. • A special instrument will gently align the cervical canal and uterine cavity. • Another instrument will measure the depth of the uterine cavity. • Provider will fold Mirena's horizontal arms and place it inside an applicator tube. The tube will be inserted into the cervical canal and the Mirena will be carefully placed in the uterus. When the applicator tube is removed, the Mirena will remain in place. • Provider will trim Mirena's strings so that they don't protrude too far into the vagina. 3 Women’s Health Mini-Residency for Primary Care Nursing 11/28/12 • During Mirena insertion, you may experience moderate to severe cramping, dizziness, fainting, nausea, low blood pressure or a slower than normal heart rate. Rarely, it’s possible for the IUD to perforate the uterine wall or cervix. C. What are post-procedure recommendations? • After every period, or every two months if no menstrual flow, ensure that Mirena's strings are protruding from the cervix. Don't pull on the strings. • Four to six weeks after Mirena is inserted, provider may want re-examine you to check for infection and to make sure Mirena hasn't moved. • Expect irregular bleeding and/or cramps during first weeks after insertion • Record the date of Mirena insertion, recommended date for Mirena removal, and lot number. Keep this information in a safe place. • Contact provider if… − Severe abdominal pain or pain during sex − IUD strings are missing or suddenly seem longer, or hard plastic can be felt − Extreme lightheadedness or fainting − Signs of pregnancy − Unusually heavy vaginal bleeding − Unexplained fever − Unusual or foul-smelling vaginal discharge, lesions, or sores − Very severe headaches or migraines − Exposed to a sexually transmitted infection HAVE THESE SUPPLIES AVAILABLE ON THE SHOW-AND-TELL TABLE Graves and Pederson specula Sterile tenaculum Sterile scissors Sterile uterine sound Mirena IUD Patient education handout 4