Appendix B: Oral Care with Chlorhexidine (CHG)
advertisement
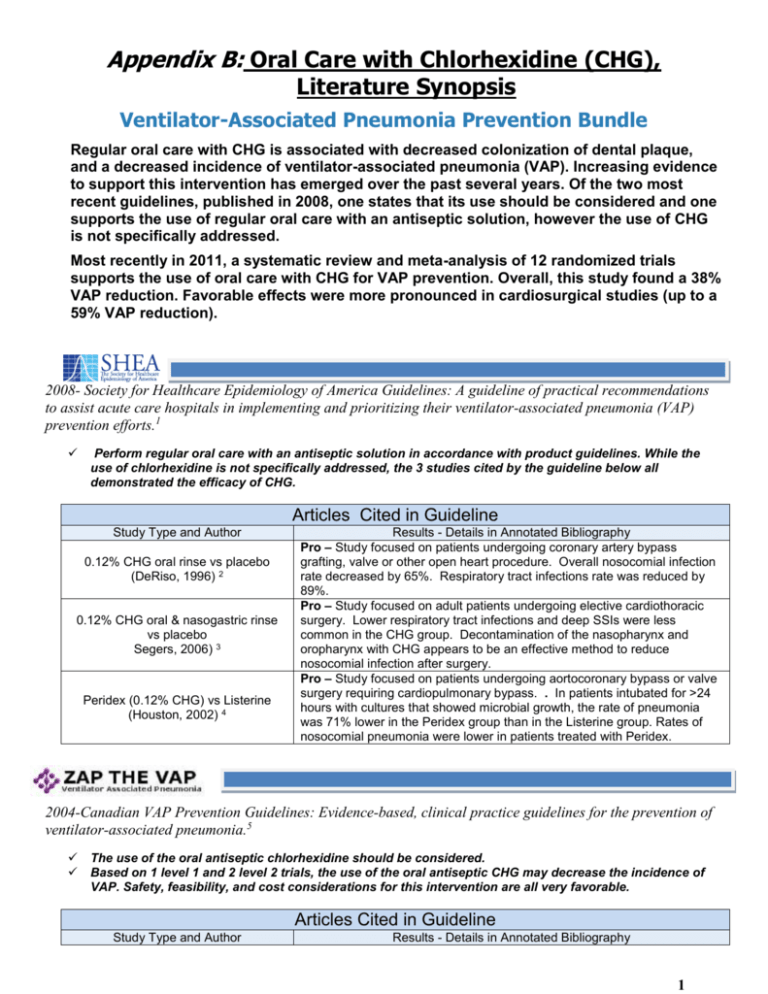
Appendix B: Oral Care with Chlorhexidine (CHG), Literature Synopsis Ventilator-Associated Pneumonia Prevention Bundle Regular oral care with CHG is associated with decreased colonization of dental plaque, and a decreased incidence of ventilator-associated pneumonia (VAP). Increasing evidence to support this intervention has emerged over the past several years. Of the two most recent guidelines, published in 2008, one states that its use should be considered and one supports the use of regular oral care with an antiseptic solution, however the use of CHG is not specifically addressed. Most recently in 2011, a systematic review and meta-analysis of 12 randomized trials supports the use of oral care with CHG for VAP prevention. Overall, this study found a 38% VAP reduction. Favorable effects were more pronounced in cardiosurgical studies (up to a 59% VAP reduction). 2008- Society for Healthcare Epidemiology of America Guidelines: A guideline of practical recommendations to assist acute care hospitals in implementing and prioritizing their ventilator-associated pneumonia (VAP) prevention efforts.1 Perform regular oral care with an antiseptic solution in accordance with product guidelines. While the use of chlorhexidine is not specifically addressed, the 3 studies cited by the guideline below all demonstrated the efficacy of CHG. Articles Cited in Guideline Study Type and Author 0.12% CHG oral rinse vs placebo (DeRiso, 1996) 2 0.12% CHG oral & nasogastric rinse vs placebo Segers, 2006) 3 Peridex (0.12% CHG) vs Listerine (Houston, 2002) 4 Results - Details in Annotated Bibliography Pro – Study focused on patients undergoing coronary artery bypass grafting, valve or other open heart procedure. Overall nosocomial infection rate decreased by 65%. Respiratory tract infections rate was reduced by 89%. Pro – Study focused on adult patients undergoing elective cardiothoracic surgery. Lower respiratory tract infections and deep SSIs were less common in the CHG group. Decontamination of the nasopharynx and oropharynx with CHG appears to be an effective method to reduce nosocomial infection after surgery. Pro – Study focused on patients undergoing aortocoronary bypass or valve surgery requiring cardiopulmonary bypass. . In patients intubated for >24 hours with cultures that showed microbial growth, the rate of pneumonia was 71% lower in the Peridex group than in the Listerine group. Rates of nosocomial pneumonia were lower in patients treated with Peridex. 2004-Canadian VAP Prevention Guidelines: Evidence-based, clinical practice guidelines for the prevention of ventilator-associated pneumonia.5 The use of the oral antiseptic chlorhexidine should be considered. Based on 1 level 1 and 2 level 2 trials, the use of the oral antiseptic CHG may decrease the incidence of VAP. Safety, feasibility, and cost considerations for this intervention are all very favorable. Articles Cited in Guideline Study Type and Author Results - Details in Annotated Bibliography 1 0.2% CHG vs placebo (Fourrier, 2005) 6 0.2% CHG vs standard oral care (Fourrier, 2000) 7 2% CHG vs 2% CHG+2% colistin vs placebo (Koeman, 2006) 8 Con – Study focused on a population of nonedentulous patients requiring endotracheal intubation and mechanical ventilation. Gingival and dental plaque antiseptic decontamination significantly decreased the oropharyngeal colonization by aerobic pathogens. Efficacy was insufficient to reduce the number of respiratory infections due to MDR bacteria. No difference was observed in the incidence of ventilator-associated pneumonia per ventilator or intubation days. Pro – Study focused on patients admitted to ICU requiring mechanical ventilation with an expected >5 day stay. There was a trend to a reduction of mortality, length of stay and duration of mechanical ventilation. Decreases dental bacterial colonization and may reduce incidence of nosocomial infections. Pro – Study focused on patients needing mechanical ventilation for ≥ 48 hours. Risk of VAP reduced in both CHG groups. CHG+Colistin provided significant reduction in oropharyngeal colonization with both gram-negative and gram-positive microorganisms, whereas CHG mostly affected grampositive microorganisms. Endotracheal colonization was reduced for CHG+Colistin patients and to a lesser extent for CHG patients.. 2004-Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcareassociated pneumonia.9 Recommends regular oral care. States that chlorhexidine has prevented hospital-acquired pneumonia in specific populations such as those undergoing coronary bypass grafting, However, also states that routine use is not recommended until more data is available. Articles Cited in Guideline Study Type and Author 0.12% CHG oral rinse vs placebo (DeRiso, 1996) 2 Results - Details in Annotated Bibliography Pro – Study focused on patients undergoing coronary artery bypass grafting, valve or other open heart procedure. Overall nosocomial infection rate decreased by 65%. Respiratory tract infections rate was reduced by 89%. (Previously cited in SHEA Guidelines, above) 2003-CDC Guidelines for preventing Health-Care-Associated Pneumonia10 No recommendation can be made for the routine use of an oral chlorhexidine rinse for the prevention of health-care–associated pneumonia in all postoperative or critically ill patients and/or other patients at high risk for pneumonia (Unresolved issue) (II) Articles Cited in Guideline Study Type and Author 0.12% CHG oral rinse vs placebo (DeRiso, 1996) 2 Results - Details in Annotated Bibliography Pro – Study focused on patients undergoing coronary artery bypass grafting, valve or other open heart procedure. Overall nosocomial infection rate decreased by 65%. Respiratory tract infections rate was reduced by 89%. (Previously cited in SHEA Guidelines, above) 2 Post Guideline Publications: Post Guideline Publications, 2007-2012 Study Type and Author Systematic Review (no metaanalysis) (CHG and toothbrushing) (Roberts, 2011) 11 Review and Meta-analysis (CHG vs povidone-iodine) (Labeau, 2011) 12 0.12% CHG vs placebo (Jacomo, 2011) 13 Results - Details in Annotated Bibliography Pro – Analyzed RCTs assessing the effectiveness of CHG and toothbrushing to reduce VAP rates. CHG has been proven to be of value in reducing VAP. 0.12% CHG+swab bid, toothbrushing tid, 0.12% CHG+toothbrushing tid and usual care (Munro, 2009) 20 Pro – Analyzed RCTs of mechanically ventilated adult patients receiving oral care with CHG or povidone-iodine. CHG shown to be effective. Effect more pronounced in cardiac surgery patients. Con – Study focused on children undergoing surgery for congenital heart disease. There was a non-statistical increase of VAP in the treatment group. Pro – Study focused on trauma patients requiring endotracheal intubation. Treatment group had lower CPIS scores at 48 and 72 hours and a statistically insignificant lower rate of VAP. In patients without pneumonia at baseline, the reduction in the incidence of VAP was greater. Con – There is no evidence to support the use of one oral rinse over another in mouth care, exception of CHG in the cardiac surgery population. Pro – Used a “bundle development strategy” to choose the most effective interventions to include in a VAP Care Bundle. Oral care with chlorhexidine is number 5 in the European care bundle. Neutral – Study focused on intubated patients in a trauma ICU. Nonsignificant reduction in pneumonia rate noted in groups treated with CHG. Con – This study does not specifically look at patients on mechanical ventilation. Study focused on patients admitted to the ICU with a prospective length of stay of over 48 hours. Overall incidence of respiratory tract infections similar between treatment and control groups. Pro – Study focused on oral colonization in 65 children receiving mechanical ventilation. On day 2, number of children with an increase in positive samples was higher in the control group. However, the difference was not significant. Pro – Study focused on adult patients enrolled within 24 hours of intubation. Significantly reduced the incidence of pneumonia on day 3. CHG reduced early ventilator-associated pneumonia in patients without pneumonia at baseline. 0.12% CHG+gauze application vs 0.12% CHG+electric toothbrush application (Pobo, 2009) 21 Neutral – This study did not specifically address the effectiveness of CHG, but addressed the appropriate use of CHG. Study focused on adult patients intubated for >48 hours. Groups had similar rates of suspected VAP. Single dose 5 mL CHG w/oral swab vs control (no swab) (Grap, 2011) 14 Consensus development (Berry, 2011) 15 Consensus development (Rello-2010) 16 0.12% CHG vs placebo(Scannapieco, 2009) 17 0.12% CHG vs placebo (Bellissimo-Rodrigues, 2009) 18 0.12% CHG vs placebo (Pedreira, 2009) 19 Review and Meta-analysis (Chan, 2007) 22 Review (Gastmeier, 2007) 23 Pro – This analysis did not specifically address the use of CHG, but addressed the effect of using antibiotics and antiseptics for the prevention of VAP. Analyzed RCTs evaluating the efficacy of daily oral application of antibiotics or antiseptics with no prophylaxis on mechanically ventilated adult patients. Oral decontamination can reduce the incidence of VAP. Of the evaluated studies, only one did not use CHG. CHG efficacy may be dependent on concentration. Pro – Reviewed articles published since 2004 dealing with infection control measures for prevention of VAP. Special emphasis was placed on RCTs, meta-analyses, systematic reviews and studies reviewing multimodal interventions. The data lead to the conclusion that topical use of chlorhexidine for oral care is beneficial. 3 Annotated Bibliography 1. Coffin S, MD, Klompas M, MD, Classen D, MD, et al. Strategies to prevent Ventilator‐Associated pneumonia in acute care hospitals • . Infection Control and Hospital Epidemiology. 2008;29(S1, A Compendium of Strategies to Prevent Healthcare‐Associated Infections in Acute Care Hospitals):pp. S31-S40. Available from: http://www.jstor.org/stable/10.1086/591062. 2. DeRiso AJ,2nd, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest. 1996;109(6):1556-1561. Pro – 0.12% CHG oral rinse vs placebo – This study looked at all HAIs in 353 cardiac surgery patients ondergoing coronary artery bypass grafting, valve or other open heart procedure. The overall nosocomial infection rate was decreased in the CHG-treated patients by 65% (24/180 vs 8/173; p<0.01). We also noted a 69% reduction in the incidence of total respiratory tract infections in the CHG-treated group (17/180 vs 5/173; p<0.05). Gram-negative organisms were involved in significantly less (p<0.05) of the nosocomial infections and total respiratory tract infections by 59% and 67%, respectively. No change in bacterial antibiotic resistance patterns in either group was observed. The use of nonprophylactic IV antibiotics was lowered by 43% (42/180 vs 23/173; p<0.05). A reduction in mortality in the CHG-treated group was also noted (1.16% vs 5.56%). Inexpensive and easily applied oropharyngeal decontamination with CHG oral rinse reduces the total nosocomial respiratory infection rate and the use of nonprophylactic systemic antibiotics in patients undergoing heart surgery. This results in significant cost savings for those patients who avoid additional antibiotic treatment. [[ for respiratory infections, NNT= 15.25 ]] 3. Segers P, Speekenbrink RG, Ubbink DT, van Ogtrop ML, de Mol BA. Prevention of nosocomial infection in cardiac surgery by decontamination of the nasopharynx and oropharynx with chlorhexidine gluconate: A randomized controlled trial. JAMA. 2006;296(20):2460-2466. Pro – 0.12% CHG oral & nasogastric rinse vs placebo – This study looked at all HAIs in 954 cardiac surgery patients. The incidence of nosocomial infection in the chlorhexidine gluconate group and placebo group was 19.8% and 26.2%, respectively (absolute risk reduction [ARR], 6.4%; 95%confidence interval [CI], 1.1%11.7%; P=.002). In particular, lower respiratory tract infections and deep surgical site infections were less common in the chlorhexidine gluconate group than in the placebo group (ARR, 6.5%; 95% CI, 2.3%-10.7%; P=.002; and 3.2%; 95% CI, 0.9%-5.5%; P=.002, respectively) [[ for lower respiratory tract infections, NNT= 15.38 ]] 4. Houston S, Hougland P, Anderson JJ, LaRocco M, Kennedy V, Gentry LO. Effectiveness of 0.12% chlorhexidine gluconate oral rinse in reducing prevalence of nosocomial pneumonia in patients undergoing heart surgery. Am J Crit Care. 2002;11(6):567-570. Pro – Peridex (0.12% CHG) vs Listerine – Study focused on a population of 561 patients undergoing aortocoronary bypass or valve surgery requiring cardiopulmonary bypass. The rate of nosocomial pneumonia was reduced by 52% (4/270 vs 9/291; p=.21) in the Peridex-treated patients. Among patients intubated for more than 24 hours who had cultures that showed microbial growth (all pneumonias occurred in this group), the pneumonia rate was reduced by 58% (4/19 vs 9/18; p=.06) in patients treated with Peridex. In patients intubated for > 24 hours , with cultures showing the most growth, the rate was 71% lower in the Peridex group (2/10 vs 7/10; p=.02). [[ for nosocomial pneumonia, for patients intubated for >24 hours, NNT= 3.45; for pneumonia among patients intubated for more than 24 hours who had cultures that showed microbial growth, NNT=2 ]] 5. Muscedere J, Dodek P, Keenan S, et al. Comprehensive evidence-based clinical practice guidelines for ventilator-associated pneumonia: Diagnosis and treatment. J Crit Care. 2008;23(1):138-147. 6. Fourrier F, Dubois D, Pronnier P, et al. Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: A double-blind placebo-controlled multicenter study. Crit Care Med. 2005;33(8):1728-1735. Con – 0.2% CHG vs placebo - Study focused on a population of 228 nonedentulous patients requiring endotracheal intubation and mechanical ventilation. The incidence of nosocomial infections was 17.5% (13.2 per 1000 ICU days) in the placebo group and 18.4% (13.3 per 1000 ICU days) in the plaque antiseptic decontamination group (not significant). No difference was observed in the incidence of ventilator-associated pneumonia per ventilator or intubation days, mortality, length of stay, and care loads (secondary end points). On day 10, the number of positive dental plaque cultures was significantly lower in the treated group (29% vs. 66%; p < .05). Highly resistant Pseudomonas, Acinetobacter, and Enterobacter species identified in late-onset ventilator-associated pneumonia and previously cultured from dental plaque were not eradicated by the antiseptic decontamination. 7. Fourrier F, Cau-Pottier E, Boutigny H, Roussel-Delvallez M, Jourdain M, Chopin C. Effects of dental plaque antiseptic decontamination on bacterial colonization and nosocomial infections in critically ill patients. Intensive Care Med. 2000;26(9):1239-1247. Pro - 0.2% CHG vs standard oral care - Study focused on patients admitted to the ICU with a medical condition suggesting an ICU stay of 5 days and requiring mechanical ventilation. Sixty patients were included; 30 in the treated group and 30 in the control one (mean age: 51 +/- 16 years; mean Simplified Acute Physiological Score II: 35 +/- 14 points)````. On admission, no significant differences were found between both groups for all clinical and dental data. Compared with the control group, the nosocomial infection rate and the incidence densities related to risk exposition were significantly lower in the treated group (18 vs 33% days in the ICU and 10.7 vs 32.3% days of mechanical ventilation; P < 0.05). These results were consistent with a significant preventive effect of the antiseptic decontamination (Odds Ratio: 0.27; 95% CI: 0.09; 0.80) with a 53% relative risk reduction. There was a trend to a reduction of mortality, length of stay, and duration of mechanical ventilation. 8. Koeman M, van der Ven AJ, Hak E, et al. Oral decontamination with chlorhexidine reduces the incidence of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2006;173(12):1348-1355. Pro - CHG vs CHG+Colistin vs placebo - Study focused on 385 patients needing mechanical ventilation for ≥ 48 hours. 130 received placebo, 127 CHG and 128 CHG+Colistin. The daily risk of VAP was reduced in both treatment groups compared with placebo: 65% (hazard ratio [HR] 0.352; 95% confidence interval [CI], 0.160, 0. 791; p _ 0.012) for CHG and 55% (HR _ 0.454; 95% CI, 0.224, 0. 925; p _ 0.030) for CHG+Colistin. CHG+Colistin provided significant reduction in oropharyngeal colonization with both gram-negative and gram-positive microorganisms, whereas CHG mostly affected gram-positive microorganisms. Endotracheal colonization was reduced for CHG+Colistin patients and to a lesser extent for CHG patients. 9. American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416. 10. Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidleines for preventing healthcare-associated pneumonia, 2003: Recommendations of CDC and the healthcare infection control practices advisory committee. MMWR Recomm Rep. 2004;53:1-36. 11. Roberts N, Moule P. Chlorhexidine and tooth-brushing as prevention strategies in reducing ventilator-associated pneumonia rates. Nurs Crit Care. 2011;16(6):295-302. Pro – Systematic Review of 17 papers addressing the use of CHG and toothbrushing to reduce VAP rates. The use of chlorhexidine has been proven to be of some value in reducing VAP, although may be more effective when used with a solution which targets gram-negative bacteria. Tooth-brushing is recommended in providing a higher standard of oral care to mechanically ventilated patients and reducing VAP when used with chlorhexidine. However, limitations in study design and inconsistency in results suggest that further research is required into the effects of tooth-brushing. [[Pooled estimates of efficacy not calculated]] 12. Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI. Prevention of ventilator-associated pneumonia with oral antiseptics: A systematic review and meta-analysis. Lancet Infect Dis. 2011. Pro – Review and meta-analysis of 14 papers looking at the effect of oral care with CHG or povidone-iodine vs. standard oral care to reduce VAP rates. 12 studies looked at CHG and 2 at povidone-iodine. Chlorhexidine application was shown to be effective (RR 0·72; 95% CI 0·55–0·94; p=0·02), whereas the effect resulting from povidone-iodine remains unclear (RR 0·39; 95% CI 0·11–1·36; p=0·14). Heterogeneity was moderate (I²=29%; p=0·16) for the trials using chlorhexidine and high (I²=67%; p=0·08) for those assessing povidone-iodine use. Favourable eff ects were more pronounced in subgroup analyses for 2% chlorhexidine (RR 0·53, 95% CI 0·31–0·91), and in cardiosurgical studies (RR 0·41, 95% CI0·17–0·98) 4 13. Jacomo AD, Carmona F, Matsuno AK, Manso PH, Carlotti AP. Effect of oral hygiene with 0.12% chlorhexidine gluconate on the incidence of nosocomial pneumonia in children undergoing cardiac surgery. Infect Control Hosp Epidemiol. 2011;32(6):591-596. Con – CHG vs placebo - Study focused on 160 children undergoing surgery for congenital heart disease. There was no difference between the two groups.CHG vs placebo - The incidence of nosocomial pneumonia was 29.8% versus 24.6% (p=0.46) and the incidence of VAP was 18.3% versus 15% (p=0.57) in the chlorhexidine and the control group, respectively. There was no difference in intubation time (p=0.34), need for reintubation (p=0.37), time interval between hospitalization and nosocomial pneumonia diagnosis (p=0.63), time interval between surgery and nosocomial pneumonia diagnosis (p=0.10), and time on antibiotics (p=0.77) and vasoactive drugs (p=0.16) between groups. Median length of PICU stay (3 vs 4 days; p=0.53), median length of hospital stay (12 vs 11 days; p=0.67), and 28-day mortality (5.7% vs 6.8%; p=0.77) were also similar in the chlorhexidine and the control group. 14. Grap MJ, Munro CL, Hamilton VA, Elswick RK,Jr, Sessler CN, Ward KR. Early, single chlorhexidine application reduces ventilatorassociated pneumonia in trauma patients. Heart Lung. 2011;40(5):e115-22. Pro – Single dose 5 mL CHG w/oral swab vs control (no swab) - Study focused on 145 trauma patients requiring endotracheal intubation. A significant treatment effect was found on CPIS scores both from admission to 48 hours (P =.020) and to 72 hours (P = .027). In those subjects without pneumonia at baseline (CPIS < 6) (n=17), 55.6% of the control patients (10/18) had developed VAP by 48 or 72 hours versus only 33.3% of the intervention patients (7/21). [[ for VAP rates, NNT = 4.5 ]] 15. Berry AM, Davidson PM, Nicholson L, Pasqualotto C, Rolls K. Consensus based clinical guideline for oral hygiene in the critically ill. Intensive Crit Care Nurs. 2011;27(4):180-185. Pro – Consensus development process - At the present time there is no evidence to support the use of one oral rinse over another in mouth care: The exception is the use of chlorhexidine gluconate 0.12% in the cardiac surgical patient population. 16. Rello J, Lode H, Cornaglia G, Masterton R, VAP Care Bundle Contributors. A european care bundle for prevention of ventilatorassociated pneumonia. Intensive Care Med. 2010;36(5):773-780 Pro - Consensus development process - Through a “bundle development strategy” a bundle of interventions for the prevention of VAP was developed. Oral care with CHG was considered to be number 5 in the list of included items for VAP prevention. 17. Scannapieco FA, Yu J, Raghavendran K, et al. A randomized trial of chlorhexidine gluconate on oral bacterial pathogens in mechanically ventilated patients. Crit Care. 2009;13(4):R117. Neutral – 0.12% CHG once or twice per day vs placebo - This study focused on oral colonization in 175 intubated patients in a trauma unit. 60 patients were dropped due to insufficient data. Using intent-to-treat analysis (n=175), a 41% of reduction in the rate of pneumonia was noted between the treated and placebo group (odds ratio (OR) = 0.54, 95% confidence interval (CI): 0.23 to 1.25, P = 0.1459); however, the differences were found not to be statistically significant. The incidence of pneumonia by survival analysis showed that the onset of pneumonia tended to be delayed in the treated groups when compared with the control group; however, these differences were not statistically significant (hazards ratio (HR) = 0.555, 95% CI: 0.256 to 1.201, P = 0.1348). A nonsignificant reduction in pneumonia rate was noted in groups treated (n=116) with chlorhexidine compared with the placebo group (n=59) (OR = 0.54, 95% CI: 0.23 to 1.25, p= 0.15). No evidence for resistance to chlorhexidine was noted, and no adverse events were observed. No differences were noted in microbiologic or clinical outcomes between treatment arms. However, it did reduce the number of S. aureus in dental plaque of trauma intensive care patients. [[ for VAP rates in the intent-to-treat analysis, NNT = 11.5 ]] 18. Bellissimo-Rodrigues F, Bellissimo-Rodrigues WT, Viana JM, et al. Effectiveness of oral rinse with chlorhexidine in preventing nosocomial respiratory tract infections among intensive care unit patients. Infect Control Hosp Epidemiol. 2009;30(10):952-958. Neutral – CHG vs placebo - Study focused on patients admitted to the ICU with a prospective length of stay greater than 48 hours, regardless of whether they received mechanical ventilation. This study was not specifically targeted at mechanically ventilated patients. The overall incidence of respiratory tract infections in the treatment group vs placebo was 21 (n=98) and 25 (n=96), respectively (RR, 1.0 [95% CI, 0.63–1.60) and the rates of ventilator-associated pneumonia per 1,000 ventilator-days were similar in both experimental and control groups (22.6 vs 22.3; p=0.95). Respiratory tract infection–free survival time (7.8 vs 6.9 days; p=0.61), duration of mechanical ventilation (11.1 vs 11.0 days; p=0.61), and length of stay (9.7 vs 10.4 days; p=0.67) did not differ between the chlorhexidine and placebo groups. However, patients in the chlorhexidine group exhibited a larger interval between ICU admission and onset of the first respiratory tract infection (11.3 vs 7.6 days; p=0.05). [[ for respiratory tract infections, NNT= 21 ]] 19. Pedreira ML, Kusahara DM, de Carvalho WB, Nunez SC, Peterlini MA. Oral care interventions and oropharyngeal colonization in children receiving mechanical ventilation. Am J Crit Care. 2009;18(4):319-28; quiz 329. Pro - 0.12% CHG vs placebo - Study focused on 56 children (47 intubated and 9 with < 24 hours intubation) admitted to the PICU. They evaluated colonization of the oropharynx at day 0, 2, 4, and PICU discharge. During the first 48 hours of PICU admission, the number of children colonized with pathogenic microorganisms decreased in the experimental group and increased in the control group. Colonization by pathogenic bacteria did not differ between the 2 groups of children. From day 0 to day 2, the number of children with an increase in the number of samples positive for pathogenic flora was greater in the control group than in the experimental group, but the difference was not significant. Similarly, the colonization of the oral cavity by normal flora did not differ between the 2 groups of children. The 2 groups did not differ significantly in the colonization of normal (P= .72) or pathogenic (P= .62) flora, in the duration of mechanical ventilation (P= .67), or in length of stay in the intensive care (P= .22). 20. Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults. Am J Crit Care. 2009;18(5):428-37; quiz 438. Pro - 0.12% CHG+swab bid, toothbrushing tid, 0.12% CHG+toothbrushing tid and usual care - Study focused on 547 adult patients enrolled within 24 hours of intubation. However, chlorhexidine significantly reduced the incidence of pneumonia on day 3 (n=87) among patients who had CPIS <6 at baseline (P = .006). Toothbrushing had no effect on CPIS and did not enhance the effect of chlorhexidine. Chlorhexidine, but not toothbrushing, reduced early ventilatorassociated pneumonia in patients without pneumonia at baseline. 21. Pobo A, Lisboa T, Rodriguez A, et al. A randomized trial of dental brushing for preventing ventilator-associated pneumonia. Chest. 2009;136(2):433-439. Neutral – This study looks at the effect of adding toothbrushing to care with CHG. Standard care, defined as 0.12% CHG oral care (20 mL applied with gauze and a 10 mL rinse) vs standard care with the addition of an electronic toothbrush - Study focused on adult patients expected to be mechanically ventilated for >48 hours (n=147) The standard care and standard care + toothbrush groups had similar rates of suspected VAP (20.3% vs 24.7%; p _ 0.55). After adjustment for severity of illness and admission diagnosis, the incidence of microbiologically documented VAP was also similar in the two groups (hazard ratio, 0.84; 95% confidence interval, 0.41 to 1.73). The groups did not differ significantly in mortality, antibiotic-free days, duration of MV, or hospital ICU LOS. [[ to assess the effect of toothbrushing added to oral care with CHG, NNT=23 5 22. Chan EY, Ruest A, Meade MO, Cook DJ. Oral decontamination for prevention of pneumonia in mechanically ventilated adults: Systematic review and meta-analysis. BMJ. 2007;334(7599):889. Pro - This study does not specifically address the use of CHG. Rather, it assesses the effect of antibiotics and antiseptics in general. Study focused on 11 RCTs enrolling mechanically ventilated adults that compared the effects of daily oral application of antibiotics or antiseptics with no prophylaxis. In seven trials with 2144 patients, however, oral application of antiseptics significantly reduced the incidence of ventilator associated pneumonia (0.56, 0.39 to 0.81). Of the evaluated studies, only one did not use CHG. CHG efficacy may be dependent on concentration. Oral decontamination of mechanically ventilated adults using antiseptics is associated with a lower risk of ventilator associated pneumonia. 23. Gastmeier P, Geffers C. Prevention of ventilator-associated pneumonia: Analysis of studies published since 2004. J Hosp Infect. 2007;67(1):1-8. Pro - Systematic review - Special emphasis was placed on randomized controlled trials (RCTs), meta-analyses or systematic reviews and studies applying multi-module interventions. A total of 15 RCTs and seven meta-analyses or systematic reviews were found. In addition to these, five cohort studies were identified where multi-module programmes were introduced for reducing VAP rates. The data lead to the conclusion that topical use of chlorhexidine for oral care is beneficial and subglottic secretion drainage may lead to delayed onset of VAP. Often simple interventions are useful for the reduction of VAP rates, for which the best chances appeared to be the application of multi-module programmes. On average a reduction of more than 40% seems to be possible. 5