Medications (see attached) Student Name _____Jessica
advertisement

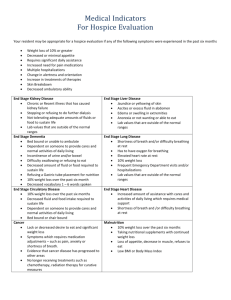
Medications (see attached) IV Sites/Fluids/Rate Left Hand: 18 ½ NS @ 80 cc/hr and Vancomycin @ 166 cc/hr State lab values and identify trends. Student Name _____Jessica Thompson____ Client Initials ___MLV___ Date __1/30/12___ Age __43___ Gender __M___ Room # __24__ Admit Date __1/29/12___ 1/30/12 143 │ 112H │ 26 5.4H │21 │ 2.21H 105 CODE Status ____Full____ Allergies ___NKA____ Diet ___Clear Liquid___ Activity ___Up As Tolerated___ Braden Score ___16___ Monitoring: ___Ca ___Mg PO4 10.3 10.5L 317 32.6L State other appropriate lab results Chief Complaint/Admitting Diagnosis(es): External/non-invasive 5 lead, pulse ox, BP cuff Shortness of breath, cough with clear phlegm and shaking chills. Labored breathing with wheezing. Reddened right lower extremity (calf). Medical/Surgical Diagnosis(es): Respiratory failure with left lower lobe Pneumonia with left-sided pleural effusion. Sepsis with acute renal failure. ECG Interpretation (see attached) 1.) 43 year old male with morbid obesity was brought to the emergency room because of a one week history of SOB and clear productive cough. Pt c/o unusual labored breathing with walking a flight of stairs and being unable to catch his breath at which time an ambulance was called to his home. 2.) The “development of acute pneumonia implies a defect in host defenses, a particularly virulent organism, or an overwhelming inoculation event” (Urden, 2010, p.614). In this case, the pneumonia was community-acquired; possibly related to Streptococcus pneumoniae, Legionella spp., Haemophilus influenza, or respiratory viruses for example, which will be determined through the pending blood culture. Sepsis is a complex over-response of the immune system in response to an infection. “Sepsis is the most common cause of acute kidney failure in the critically ill; by creating hemodynamic instability and reduced perfusion to the kidneys” (Urder, 2010, p. 798). 3.) A head to toe assessment preformed 1/30/12 found the following: Vitals: HR- 160(increased heart rate is common in patients with sepsis, as the body is compensating for decreased blood pressure), RR- 30 (a common manifestation in these patients related to the lungs compensating for their decreased function), BP124/66(although this is an acceptable blood pressure, pressures are lowered with sepsis), T- 99.0F (elevated temperature points to the presence of infection)and pulse 1/29/12: ABGs- metabolic acidosis PH: 7.29L pCO2: 38.8 pO2: 73L bicarb: 18.3L base: -7.6L O2 saturation: 92.5% 1/30/12: Renal Labs AST: 15 ALT: 10L State diagnostic test results 1/29/12:PCXR- complete opacification of lower half of left hemithorax consistent with pleural effusion. Atelectasis and consolidation; right lung is clear; enlarged heart –cardiomegaly. 1/29/12: Blood Culture- results pending 1/30/12: Duplex scan of bilateral lower extremities- no echogenic Past Medical/Surgical History Relevant to this admission Obstructive sleep apnea Hx of smoking- quit 10 years ago NIDDM morbidly obese HTN oximetry- 98% with NC 14Lpm(Increased need for oxygen supply relates to the decreased function of lungs to provide the blood stream with adequate amounts of oxygen). Pain is reported as 5/10: general all over and lower back (this may be related to the acute kidney failure). A&Ox3, pt c/o feeling “woozy” with standing(disorientation and hypoxemia related to both pneumonia and sepsis can lead one to feel dizzy with position changes), all extremities strong and equal. Pt states he is normally confined in his home due to his anxiety related to agoraphobia. PERRLA, normal sinuses and glands, no drainage from ears, nose, eyes. Mucous membranes pink and moist. Skin is warm and dry with normal capillary refill and turgor. Lower extremities with bilateral edema pitting +2(septic shock increases membrane permeability, allowing for fluid moving into the third space). Redness noted on entire length of posterior right lower extremity(discomfort may be related to the increased fluid and stretch of the skin of the edematous extremities) with little associated pain. Heart sounds are rhythmic but tachycardic(as previously noted, heart rate increases to compensate for decreased blood pressure with sepsis) Lungs are clear, equal but diminished (Alterations in lung function relate to abnormal lung sounds). Abdomen is large and firm with hypoactive bowel sounds. LBM was 1/28/12. Voiding pattern q3hr. 4.) With sepsis, “ABG values reveal metabolic acidosis”, as seen in this case (Urden, 2010, p. 994), as well as hemodynamic changes such as increased WBCs. Metabolic acidosis relates directly to the decreased renal functioning; as kidney perfusion is changed, urine output is altered and laboratory results in turn are abnormal(decreased renal labs and abnormal ABG results). Blood and sputum cultures will reveal what factor has caused this medical condition, however, until those results are revealed a resuscitation bundle was administered. This bundle “measures serum lactate, provides broad spectrum antibiotics, maintains or improves blood pressure with fluids and vasopressors” (Urden, 2010, p. 994). At this time broad spectrum antibiotic are being given to help fight any organism that is causing the infection; as specific laboratory details are noted medications can be narrowed to fight the exact organism. A focus for this patient is preventing further sepsis and sepsis related shock. Nursing interventions include administering prescribed fluids and medications, promoting comfort and emotional support, monitoring for further complications, practicing and most importantly, teaching hand washing. As noted by the patient, he lives a more secluded and isolated lifestyle, because of this, he had not received vaccinations, anytime spent out in the community or in conversing with his family allowed him to contract a microorganism leading to pneumonia and sepsis; hygiene and hand filling noted. 1/30/12: Chest Ultrasound 1/30/12: Sputum Culture and Sensitivity- results pending Treatments/ Medical and Nursing Interventions 1/29/12: Bipap 2hr on/2hr off 40% and prn 16/11 titrate O2 to keep >92%, nonrebreather mask 55% alternate with NC 14Lpm. 1/29/12:aerosol albuterol 2.5mg q6hr and q2hr prn. 1/29/12:thoracentesis of left pleural effusion- removal of 2640mL pinkish milky colored pleural fluid. This fluid shows markedly elevated triglycerides, suspicious for chylothorax 1/29/12: ACHS blood sugar checks 1/29/12: consultations with infectious disease and pulmonology washing could have prevented him from becoming ill. Chest radiography, sputum and blood cultures, chemistry panel, and ABG are common tests relating to pneumonia. Treatment of pneumonia includes the use of antibiotics, oxygen therapy and possible mechanical ventilation. In this case, the patient has been ordered bipap therapy alternated with oxygen flow via nasal cannula, as well as aerosol treatments to help open the airway. This patient also underwent a thoracentesis to remove excess pleural fluid. Nursing interventions once again, include practicing and promoting the prevention of spreading infection, as well as positioning the patient in comfortable ways allowing for adequate ventilation and exercises to improve lung function, such as coughing and deep breathing and use of the incentive spirometer. Primary Nursing Diagnosis with Relational Statement Short Term Goal Relevant to Nursing Diagnosis Ineffective breathing pattern related to decreased lung expansion and function. 6 Nursing Diagnosis with Relational Statement 1. The client will demonstrate improved gas exchange in the lungs as seen in improving ABG results and respirations of normal levels (12-20 breaths per minute) within 24 hours of admission 2. 3. 4. During my shift, the patient’s oxygen saturation remained in normal levels, his respirations remained high but were lower than previously noted. 5. 6. Definition (State definition and source) Ineffective breathing pattern: “The state in which an individual experiences an actual or potential loss of adequate ventilation related to an altered breathing pattern” (Carpenito-Moyet, 2006, p.263). Outcome Criteria (Must be specific and measurable) 1.) The client’s ABGs will be within a normal range within 24 hours of hospitalization: Goal not met, Activity intolerance related to morbid obesity and decreased lung function Excess fluid volume related to decreased renal function Impaired gas exchange related to decreased lung function Social isolation related to fear of crowds Ineffective tissue perfusion related to decreased lung function and sedentary lifestyle Knowledge deficit related to current health status. AEB DM, obesity, HTN, acute renal failure, sepsis AEB: Defining characteristics specifically exhibited by your patient that support primary nursing diagnosis Pneumonia: left lower lobe consolidation, atelectasis and pleural effusion Pulse oximetry of 98% with NC at 14 Lpm RR rate of 30 Sinus tachycardic at a rate of 160 ABG showing metabolic acidosis Morbid obesity Continuation of admitting complaints (SOB, labored breathing) however, levels have improved since initial ABG analysis. 2.) The client will be able to move pulmonary secretions after education in coughing and deep breathing: Goal met, the patient was able to produce a sputum specimen for culture and sensitivity after using this expectoration technique. 3.) While on my shift, the client’s oxygen saturation will maintain status above 92%: Goal met, monitoring of oxygen saturation did not dip below 95% throughout my shift. 4.) While on my shift, the client’s lung sounds will improve: Goal not met, lung sounds remained clear, equal and diminished. Identify nursing interventions that you implemented with this patient. Evaluate patient progress towards achieving outcome criteria as a result of nursing interventions. 1.) Distracted patient from nervous thinking by having him tell me about his family; this allowed his respiratory and heart rates to decrease for that time period, further allowing for improved breathing pattern and oxygenation. 2.) Raised head of bed to allow for improved lung expansion; this allowed for less labored breathing and for adequate oxygenation. 3.) Educated on coughing and deep breathing techniques to help remove fluid from lungs; this allowed for the production of a sputum sample and increased numbers of available alveoli to increase amount of gas exchange. 4.) Assisting in bathing activities with nasal cannula and oxygen, allowing for bodily movement to help remove fluid from lungs. What I Would Do Differently I would have asked more questions about the bipap settings and the reasoning behind alternating the bipap with nasal cannula. I would have provided the client with information and/or support therapy for his fear of crowds. Emphasized the importance of hand washing and hygiene to prevent further infection and spreading the current infection. References Carpenito-Moyet, L.J. (2006). Nursing Diagnosis Application to Clinical Practice. Philadelphia, PA: Lippincott, Williams & Wilkins. Urden, L. (2010) Critical Care Nursing: Diagnosis and Management (6th ed.). St. Louis, MO: Mosby Elsevier.