Ebola Haemorrhagic Fever Outbreak in Guinea
advertisement

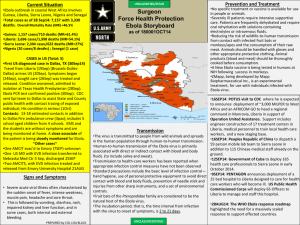
ALERT TO HEALTHCARE WORKERS: EBOLA HAEMORRHAGIC FEVER OUTBREAK IN GUINEA LIBERIA AND SIERRA LEONE, WEST AFRICA Summary of current outbreak in Guinea, Liberia and Sierra Leone The Ebola virus has been confirmed as the cause of an outbreak of haemorrhagic fever in Guinea, West Africa. This is the first recorded outbreak of Ebola haemorrhagic fever (EHF) in Guinea, where Lassa fever is commonly reported. The most recent outbreaks of EHF were reported from the Democratic Republic of Congo and Uganda in 2012. This outbreak is reported to have started in early February 2014. According to the World Health Organization (WHO), as of 28March 2014 the total number of cases in the ongoing EHF outbreak in Guinea has increased to 112, including 70 deaths(CFR=62.5%). New suspected cases have been reported from Conakry (n=4), Gueckedou (n=4), Macenta (n=1) and Dabola (n=1) prefectures. The date of hospital admission of the most recent suspected case is 28 March 2014. All age groups have been affected, but most of the cases are adults aged 15-59 years. To date, all cases have been in persons or healthcare workers attending to cases or attending burials from three districts (Gueckedou, Macenta and Kissidougo) in the forested rural areas of south eastern Guinea, and also the capital city Conakry (Figure). Two of thenew suspected cases are healthcare workers, indicating the need to further strengthen health facility-based infection prevention and control. Active contact tracing is proceeding. To date,24 clinical samples from Guinea have tested positive by PCR for the Ebola virus in samples from cases in Conakry, Gueckedou and Macent. Laboratory studies demonstrated that Zaire Ebola virus is the virus responsible for the outbreak. Ebola Zaire virus is highly lethal with CFR of up to 90% reported in previous outbreaks. In addition, Liberia has reported two laboratory-confirmed cases in persons who had travelled to Guinea. To date, Sierra Leone has reported two suspected cases, both of whom died. All of the confirmed and suspected cases reported by Liberia and Sierra Leone had travelled to Guinea before illness onset. Investigations into these suspected cases are ongoing. In accordance with the International Health Regulations (IHR 2005), the Ministries of Health of Guinea, Sierra Leone and Liberia together with WHO and other response partners are implementing a coordinated response to the outbreak. WHO and response partners are continuing to support the outbreak response through mobilising international expertise Page 1 of 5 (clinical care, infection prevention and control including isolation services, surveillance and epidemiology, laboratory diagnosis and reference, logistics and social mobilisation). Ebola haemorrhagic fever: the basics The ecology of the Ebola virus is not completely understood. The current prevailing hypothesis is that the virus is introduced into the human population through close contact with infected animals (including chimpanzees, gorillas, bats, monkeys, forest antelope and porcupines). The likely reservoir of the virus includes specific species of arboreal bats, and contact with these animals and/or their excretions/secretions may also result in transmission of the virus to humans. Human-to-human transmission often occurs, and is a predominant feature of outbreaks. The disease can be spread from person to person through contact with blood, secretions, organs, or other body fluids. Ebola haemorrhagic fever outbreaks have been reported most commonly from the Democratic Republic of Congo, Uganda, South Sudan, Congo and Gabon. The incubation period of the disease is 2 - 21 days. An acute onset of prodromal symptoms which include fever, malaise, myalgia, diarrhoea, vomiting and abdominal pain is usual, followed by progressive multisystem disease with bleeding as a cardinal feature in the majority of patients. Currently, there is no known specific treatment or preventative vaccine for this highly contagious virus. Risk of imported Ebola haemorrhagic fever cases Since the current outbreak is reported in predominantly rural areas which are not frequented by many tourists or travellers, the risk of Ebola haemorrhagic fever cases being imported into South Africa is low. However, healthcare or international agency workers etc. involved in the outbreak response may travel to and present in South Africa for medical care, and a high index of suspicion is important for such cases. A detailed history regarding travel and level of contact with suspected/confirmed Ebola haemorrhagic fever cases is extremely important. Recommendations for travel to/from Guinea and West Africa The World Health Organization (WHO) does not recommend that any travel or trade restrictions be applied to Guinea, Liberia or Sierra Leone based on the current information available for this event. There are no special precautions or directives for commercial flights, passengers or crew departing on flights bound for or returning to Guinea, Liberia or Sierra Leone. The regulations for evidence of a valid yellow fever vaccination certificate apply. Page 2 of 5 Any ill persons reported on flights from Guinea, Liberia or Sierra Leone and neighbouring countries will need to be evaluated by the relevant Port Health officials. All requests for medical evacuation of persons from Guinea, Liberia or Sierra Leone with febrile illness or suspected infectious disease will need careful evaluation by the Port Health officials. While the risk of introduction of Ebola virus into South Africa is considered low, we strongly recommend that surveillance for viral haemorrhagic fevers (and at present, particularly Ebola haemorrhagic fever), be strengthened. This should be done primarily through Port Health services, but it is also extremely important that public and private practitioners are on the alert for any ill persons that have travelled to viral haemorrhagic fever risk areas. There needs to be a high index of suspicion for EHF in health workers from the affected region with unexplained fever. Evaluation of illness in travellers from Guinea and West Africa It is critical to maintain a very high index of suspicion for common causes of febrile illness in persons who have travelled to Guinea and surrounding countries, including: malaria, dengue fever, Lassa fever and other endemic diseases (e.g. typhoid fever). These may be severe and life-threatening, and healthcare workers are urged to do appropriate tests and institute appropriate therapy as a matter of urgency. Malaria is the most likely cause of an acute febrile in returning travellers from most African countries and has to be prioritised for testing. However, Lassa fever is endemic in certain West African countries, including Nigeria, Sierra Leone, Guinea and Liberia - and needs to be considered in the differential diagnosis for any traveller from these countries who has unexplained febrile illness and has visited rural areas. Lassa fever virus is transmitted to humans through direct contact with urine and droppings of infected multi-mammate rats, which contaminate the environment and food items. Transmission can also occur through the inhalation of aerosolised infected rodent excreta. Person-to-person transmission is also important, being common in both village and healthcare settings, and occurs through direct contact with blood, tissue, secretions or excretions of an infected person; therefore, VHF isolation precautions are recommended for nursing patients with Lassa fever. The incubation period is 1-3 weeks; symptoms include fever, retrosternal pain, sore throat, back pain, cough, abdominal pain, vomiting, diarrhoea, facial swelling and mucosal bleeding. Mortality rates approach 20%, with pregnant women in their third trimester being at highest risk for severe disease and death. Given that the incubation periods and clinical presentations of Lassa fever and Ebola haemorrhagic fever may overlap, both diseases must be excluded in persons who have a suggestive travel history and present with a febrile illness. Suspected Ebola haemorrhagic fever case definition and laboratory testing Page 3 of 5 The case definition for suspected Ebola haemorrhagic fever is as follows: Any person* presenting with an acute onset of fever that has: Visited or been resident in Guinea, Liberia or Sierra Leone in the 21 days prior to onset of illness AND had direct contact or cared for suspected/confirmed Ebola haemorrhagic fever cases in the 21 days prior to onset of illness, or been hospitalised in Guinea OR Has unexplained multisystem illness that is malaria-negative *Healthcare workers in particular are at high risk Testing for viral haemorrhagic fever viruses (including Ebola virus) in South Africa is only available at the NICD. Ebola haemorrhagic fever testing is neither warranted nor useful for persons that are not suffering from a clinical illness compatible with Ebola haemorrhagic fever, even in the event of compatible travel histories. The tests cannot be used to determine if the patient has been exposed to the virus and may develop the disease later. Requests for testing (with a detailed clinical, travel and exposure history) should be directed to the NICD Hotline at 082 883 9920 (a 24-hour service, for healthcare professionals only). Page 4 of 5 Figure.Geographic distribution of Ebola haemorrhagic fever in Guinea and Liberia, as at 28 March 2014.World Health Organization Regional Office for Africa. Page 5 of 5