Pathology Chapter Two [12-27
advertisement
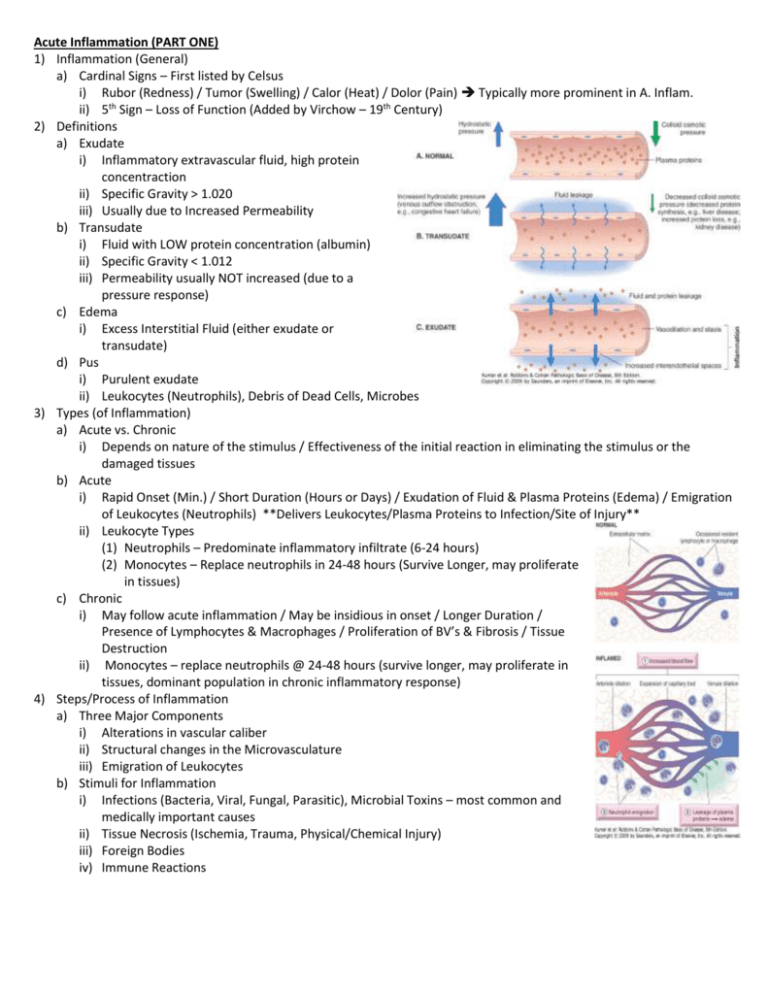
Acute Inflammation (PART ONE) 1) Inflammation (General) a) Cardinal Signs – First listed by Celsus i) Rubor (Redness) / Tumor (Swelling) / Calor (Heat) / Dolor (Pain) Typically more prominent in A. Inflam. ii) 5th Sign – Loss of Function (Added by Virchow – 19th Century) 2) Definitions a) Exudate i) Inflammatory extravascular fluid, high protein concentraction ii) Specific Gravity > 1.020 iii) Usually due to Increased Permeability b) Transudate i) Fluid with LOW protein concentration (albumin) ii) Specific Gravity < 1.012 iii) Permeability usually NOT increased (due to a pressure response) c) Edema i) Excess Interstitial Fluid (either exudate or transudate) d) Pus i) Purulent exudate ii) Leukocytes (Neutrophils), Debris of Dead Cells, Microbes 3) Types (of Inflammation) a) Acute vs. Chronic i) Depends on nature of the stimulus / Effectiveness of the initial reaction in eliminating the stimulus or the damaged tissues b) Acute i) Rapid Onset (Min.) / Short Duration (Hours or Days) / Exudation of Fluid & Plasma Proteins (Edema) / Emigration of Leukocytes (Neutrophils) **Delivers Leukocytes/Plasma Proteins to Infection/Site of Injury** ii) Leukocyte Types (1) Neutrophils – Predominate inflammatory infiltrate (6-24 hours) (2) Monocytes – Replace neutrophils in 24-48 hours (Survive Longer, may proliferate in tissues) c) Chronic i) May follow acute inflammation / May be insidious in onset / Longer Duration / Presence of Lymphocytes & Macrophages / Proliferation of BV’s & Fibrosis / Tissue Destruction ii) Monocytes – replace neutrophils @ 24-48 hours (survive longer, may proliferate in tissues, dominant population in chronic inflammatory response) 4) Steps/Process of Inflammation a) Three Major Components i) Alterations in vascular caliber ii) Structural changes in the Microvasculature iii) Emigration of Leukocytes b) Stimuli for Inflammation i) Infections (Bacteria, Viral, Fungal, Parasitic), Microbial Toxins – most common and medically important causes ii) Tissue Necrosis (Ischemia, Trauma, Physical/Chemical Injury) iii) Foreign Bodies iv) Immune Reactions c) Actions of Inflammation i) Vascular Changes – Vasodilation (1) Earliest Manifestation, follows transient constriction of arterioles (2) Last a few seconds, first involves the arterioles (3) Leads to opening of new capillary beds Increased blood flow (cause heat and redness (erythema) at site of inflammation) (4) Induced by Histamine and NO ii) Vascular Changes – Increased permeability of microvasculature (follows vasodilation) – HALLMARK of Inflammation (1) Outpouring of protein rich fluid into extravascular tissues CAUSES EDEMA (2) Mechanisms (a) Contraction of endothelial cells (i) Increased interendothelial spaces, common mechanism of vascular leakage (ii) Elicited by histamine, bradykinin, leuotrienes, the neuropeptide substance P and other mediators (iii) Immediate transient response (occurs rapidly after exposure to mediator, usually short-lived ~15-30 min) (b) Endothelial Injury (i) Results in endothelial cell necrosis/detachment (ii) Direct damage to the endothelium (c) Transcytosis (i) Increased transport of fluids and proteins through the endothelial cell iii) Vascular Changes – Loss of Fluid / Increased Vessel Diameter (1) Leads to slower blood flow, conc. of RBC’s in small vessels, increased viscosity Dilation of small vessels (packed with slowly moving red cells) Stasis iv) Stasis progresses (1) Neutrophils accumulate along the vascular endothelium (2) Endothelial cells activated by mediators produced at site of infection/tissue damage (3) Neutrophils adhere to the endothelium (migrate through vascular wall into interstitial tissue) v) Lymph Flow (1) Increased, helps drain edema fluid, accumulates due to increased vascular permeability (2) Lymph vessels proliferate during inflammatory reactions (3) Lymphatics may become inflamed due to inflammation (Lymphangitis), Draining Lymph nodes may become inflamed (lymphadenitis) (a) Hyperplasia of lymphoid follicles, increased numbers of lymphocytes and macrophages vi) Leukocytes (1) Recruited from blood into extravascular tissue, recognize microbes and necrotic tissue, REMOVE offending agent (2) Recruitment: Extravasation (Journey of Leukocytes – lumen Tissue) (a) Margination (i) Blood Flow slows early in inflammation (stasis) (ii) Hemodynamic conditions change (wall shear stress decreases) (iii) More White Cells assume peripheral position on endothelial surface (b) Rolling on Vessel Wall (i) Individual, then rows of leukocytes adhere transiently to endothelium, detach then bind again (c) Adhere (i) Cells finally come to rest, firmly attach (“pebbles which a stream runs over w.o disturbing”) (d) Migration through Endothelium (i) Diapedesis, mainly in post-capillary venules (ii) Chemokines act on adherent leukocytes (Stim. cells to migrate through interendothelial spaces, pierce the basement membrane Toward site of injury/infection where chemokines are being produced) (3) Chemotaxis of Leukocytes (a) Movement: Extend Filopodia (Pull back of cell in direction of extension) – migrate toward inflammatory stimulus **Emigrate toward site via CHEMOTAXIS – locomotion oriented along a chem. gradient) (b) Chemoattractants (i) Exogenous Substances (Bacterial Products/Lipids) (ii) Endogenous Substances (Chem Mediators- Cytokines, Components of Complement, Arachidonic Acid) (4) Leukocytic Infiltrate (a) Nature of Infiltrate depends on age of inflammatory response and type of stimulus (b) Generally (i) Acute Inflammation – Neutrophils predominate (6-24 hours), replaced by monocytes (24-48 hours), survive longer, may proliferate in tissues, become dominant population in chronic inflammatory reaction (c) Exceptions (i) Pseudomonas Bacteria – Infiltrate dominated by recruited Neutrophils for several days (ii) Viral Infections – Lymphocytes may be first cells to arrive (iii) Hypersensitivity Reactions – Eosinophils may be main cell type (5) Recognition of Microbes/Dead Tissue (a) Leukocyte – must be activated to perform function (Recognition of offending agents – activated to ingest/destroy offending agents and amplify the inflammatory response) (6) Phagocytosis (Three Steps) (a) Leukocyte recognizes/attaches particle to be ingested (b) Engulfment and formation of a phagocytic vacuole (i) Particle bound to phagocyte receptors – extensions of cytoplasm (pseudopods) pull it in, plasma membrane pinches off to form vesicle (phagosome) which fuses with lysosomal granule, degrading it (c) Kill or degrade ingested material (i) Final step of elimination of infectious agents/necrotic cells (happens within neutrophils/macrophages) (ii) Microbial killing (Reactive Oxygen Species / Reactive Nitrogen Species) 1. Also occurs through substances in leukocyte granules a. Elastase, Defensins (toxic to microbes), Cathelicidins (anti-microbial proteins), Lysozyme (Hydrolyzes bond in glycopeptide coat of bacteria), Lactoferrin (Iron-binding protein), Major basic protein (Protein of eosinophils – Limited bactericidal activity, Cytotoxic to many parasites), Bactericidal Increasing protein (binds bacterial endotoxin) (7) Functional Response of Activated Leukocytes (a) Produce Growth Factors (i) Stim. proliferation of endothelial cells / fibroblasts, Stim. synthesis of collagen, Stim. enzymes that remodel connective tissues, Drive process of repair after tissue injury vii) Defects in Leukocyte Function (1) Cause (a) Increased Vulnerability to Infections, Impaired Leukocyte Function, Inherited Defects in Leukocyte Adhesion, Inherited Defects in phagolysosome function (2) Chediak-Higashi Syndrome (a) AR condition, defective fusion of phagosomes with lysosomes (susceptible to infection) (b) Abnormal: Melanocytes (albinism), Cells of Nervous System (Nerve Defects), Platelets (Bleeding Disorders), Leukocytes (Neutropenia, Defective Degranulation, Delayed microbial killing) (3) Inherited Defects in Microbicidial Acitivity (a) Chronic Granulomatous disease – defect in bacterial killing (susceptible to recurrent bacterial infections) (b) Inherited Defect in gene encoding components of phagocyte oxidase (c) Initial neutrophil defense = inadequate (collection of activated macrophage Wall off Microbes – granulomas) (4) Acquired Deficiency (a) Bone Marrow Suppression (i) Decreased Production of Leukocytes (ii) Seen following therapy for cancer (radiation, chemotherapy) (iii) Marrow Space compromised by tumors (leukemias, metastatic from other sites) Acute and Chronic Inflammation (PART TWO) 1) Mediators of Inflammation a) Generated from cells or plasma proteins b) Types (Derived From) i) Cell-Derived Mediators (1) Generally (a) Normally sequestered in intracellular granules (b) Can be rapidly secreted by granule exocytosis (Histamine in mast cell granules) (c) Synthesized de novo in response to stimulus (Prostaglandins, Cytokines) (2) Cells producing Mediators (a) Platelets, Neutrophils, Monocytes/Macrophages, Mast Cells (b) Mesenchymal Cells (Endothelium, SM, Fibroblasts) (c) Most Epithelia ii) Plasma derived Mediators (1) Generally (a) Produced in the Liver (b) Complement proteins, Kinins (c) Present in circulation as inactive precursors (must be activated to acquire biological properties) c) Characteristics i) Active Mediators (1) Produced in response to various stimuli (a) Microbial Products, Substances released from necrotic cells (b) Proteins of complement, kinin and coagulation systems – activated by microbes and damaged tissues (ensures inflammation is normally triggered only when/where needed (2) Short Lived (once activated/released) (a) Quickly Decay (Arachidonic Acid Metabolites) (b) Inactivated by enzymes (Kininase inactivates bradykinin) (c) Scavenged or Inhibited (i) Antioxidants scavenge toxic oxygen metabolites (ii) Inhibited: Complement regulatory proteins break up and degrade activated complement components d) Cell-Derived Mediators Cell-Derived Mediators – Vasoactive Amines (stored pre-formed, among 1st released during inflammation) Histamine Serotonin MAST CELLS (CT adjacent to BV’s), Basophils & Platelets Physical Injury (Trauma, Cold, Hot) Ab’s to Mast Cells (Allergic Reaction) Complement (Anaphylatoxins- C3a/C5a) Hist.-releasing proteins (leukocyte) Neuropeptide (Substance P) Cytokines (IL-1, IL-8) Platlets, Neuroendocrine Cells (GI Tract) Actions Dilation of Arterioles, Inc. Permeability (Venules) Dilation of Arterioles, Inc. Permeability (Venules) Key Principal Mediator of Immediate transient phase of increased vascular permeability (make interendnothelial gaps in venules) Found In Released in Reponse To Platelets Aggregate (After contact w. collagen, thrombin, adenosine diphosphate and Ag-Ab complexes) Arachidonic Acid (AA) Metabolites (From dietary source – linoleic acid) **Not free in cell, esterified in membrane phospholipids (damaged mem. = release) – Mechanical, Chemical, Physical Stimuli (Release through action of cellular phospholipases)** Eicosanoids: Prostaglandins Leukotrienes Lipoxin Class Cycloocygenases Lipoxygenases Lipoxygenases Produced By Mast Cells, Macrophages, Endothelial Cells, Others Secreted mainly by leukocytes Generated from AA by lipoxygenase pathway Actions Key Action of Two Cyclooxgenases (Expressed COX-1, inducible enzyme COX2) Bind to G protein coupled receptors (mediate virtually every step of inflammation) Involved in vascular and systemic reactions of inflammation Leukocytes (esp Neutrophils) – produce intermediates in lipoxin syntehesis (converted to lipoxins by platelets interacting with leukocytes Lipoxygenase enzymes Bind to G protein coupled receptors (mediate virtually every step of inflammation) Bind to G protein coupled receptors (mediate virtually every step of inflammation) Chemo-attractants for Leukkocytes, Vascular Effects Inhibitors of Inflammation Inhibit leukocyte recruitment & other cellular components of inflammation Inhibit Neutrophil Chemotaxis & adhesion to endothelium Inverse relationship (lipoxin/leukotrienes) – negative regulators of leukotrienes (resolution of inflammation) Prostaglandins (Divided based on structural features – subscript = # of double bonds) PGI2 (Prostacyclin) Vasodilator, Potent inhibitor of Platelet Aggregation, Markedly potentiates permeability-increasing and chemotactic effects of other mediators PGD2 Major Prostaglandin (Prod. by Mast Cells) Vasodilation, Inc. Permeability of post-capillary venules EDEMA PGE2 Major Prostaglandin (Prod. by Mast Cells)- More widely distributed than PGD2 Hyperalgesic, Makes skin hypersensitive to PAIN, Involved in cytokine-induced fever (infections) PGF2α Stim. Contraction of Uterine/Bronchial SM & Small Arterioles Leukotrienes 5- Lipoxygenase LTB4 LTC4, LTD4, LTE4 Predominant in NEUTROPHILS Converts AA 5-hydrocyeicosatetraenoic acid (chemotactic for neutrophils, precursor for Leukotrienes) Potent Chemotactic Agent and Activator of Neutrophils, Cause aggregation & adhesion (venular endothelium), Generate ROS (damaging in large amounts), Releases Lysosomal Enzymes Cysteinyl-containing leukotrienes Intense Vasoconstriction, Bronchospasm and Increased Vascular Permeability i) Inhibition of Eicosanoid Synthesis (1) Anti-inflammatory drugs work by inhibiting synthesis of eicosanoids! (a) Cyclooxygenase Inhibitors (i) Ex: Aspirin, Non-steroidal anti-inflammatory drugs (Indomethacin) 1. Inhibit both COX-1/COX-2 (Prostaglandin Synthesis) (b) Lipoxygenase Inhibitors (5-lipoxygenase – not affected by NSADIs) (i) Ex: Zileuton: Inhibit leukotriene production (ii) Ex: Montelukast: Block leukotriene receptors (helpful for asthma) (c) Broad-Spectrum Inhibitors (i) Corticosteroids 1. Powerful anti-inflammatory agents 2. Reduce transcription of genes encoding COX-2, Phospholipase A2, Pro-inflammatory cytokines (IL-1, TNF) (d) Modify Dietary Lipid Intake (i) Increase consumption of Fish Oil 1. Poly unsaturated FA’s – poor substrate for conversion to active metabolites, excellent for production of anti-inflammatory lipid products (Resolvins, Protectins) 2) Platelet-Activating Factor (PAF) a) Phospholipid-derived b) Actions i) Platelet Aggregation, Vasoconstriction, Bronchoconstriction ii) Increased leukocyte adhesion, chemotaxis, degranulation, and oxidative burst iii) Boost synthesis of other mediators (Eicosanoids) iv) Low Concentrations: Induces Vasodilation, Increased Venular Permeability c) Elaborated By: Platelets, Basophils, Mast Cells, Neutrophils, Macrophages, Endothelial Cells 3) Nitric Oxide a) Soluble Gas, released from Endothelial Cells, Macrophages, some neurons b) Microbicidal – mediator of host defense against infection c) Actions i) Vasodilation ii) Paracrine manner on target cells (relaxation of vascular SM cells) iii) Inhibits cellular component of inflammatory response- inhibits several features of mast cell induced inflammation, inhibits leukocyte recruitment d) In vivo – half life is only SECONDS, gas acts only on cells in close proximity to where its produced) 4) Cytokines and Chemokines a) Cytokines i) Proteins produced by many cell types (Principally activated lymphocytes and macrophages), also endothelial, epithelial and CT’s ii) Involved in Cell IR iii) Major Cytokines Mediating Inflammation (1) TNF and IL-1 (a) Secretion stimulated by endotoxin, microbial products, immune complexes, physical injury and other inflammatory stimuli (b) Actions (i) Endothelial Activation, Induce expression of endothelial adhesion molecules (ii) Synthesize chemical mediators (Cytokines, Chemokines, Growth Factors, Eicosanoids and NO) (iii) Produce Enzymes associated with matrix remodeling (iv) Augments response of neutrophils to other stimuli (bacterial endotoxin) (v) Induce systemic acute-phase response (associated with infection/injury) (vi) Regulates energy balance – promote lipid/protein mobilization and suppress appetite 1. Sustained production Cachexia (Weight Loss/Anorexia) – accompanies some chronic infections and neoplastic diseases 4 b) Chemokines i) General (1) Chemo-attractants for specific types of leukocytes ii) Groups (Four Major) – According to arrangement of cysteine residues in mature proteins (1) C-X-C (α- chemokines) (a) Act primarily on Neutrophils – IL-8 is typical (b) Induced by: Microbial Products, other cytokines (mainly IL-1/TNF) (c) Secreted by: Activated Macrophages, Endothelial Cells (d) Causes: Activation/Chemotaxis of Neutrophils, limited activity on Monocytes and Eosinophils (2) C-C (β-chemokines) (a) Attract monocytes, eosinophils, basophils, lymphocytes (NOT NEUTROPHILS) (3) C (γ-chemokines) (a) Lymphotacin (relatively specific for lymphocytes) (4) CX3C chemokines (a) Fractalkine (Cell Surface bound protein OR Soluble Form) iii) Actions (1) Stim. Leukocyte recruitment in inflammation (2) Control normal migration of cells through various tissues 5) Neuropeptides a) Secreted by: Sensory nerves and Various Leukocytes b) Actions: Role in initiation and propogation of inflammation c) Substance P / Neurokinin A i) Produced in CNS/PNS ii) Functions (1) Transmit Pain Signals / Regulate BP / Stim. Secretion by Endocrine Cells / Increase Vascular Permeability 6) Lysosomal Constituents of Leukocytes a) Neutrophils/Monocytes : Lysosomal Granules b) Neutrophils i) Primary (Azurophil) Granules (1) Myeloperoxidase, Bactericidal Factors, Acid Hydrolases, Neutral Proteases ii) Secondary (Specific) Granules (1) Lysozyme, Collagenase, Gelatinase, Lactoferrin, Plasminogen activator, Histaminase, Alkaline phosphatase 7) Reactive Oxygen Species a) Oxygen derived free radicals (may be released extracellulary from leukocytes) – after exposure to microbes, chemokines, and immune complexes b) Production – dep. on activation of NADPH oxidase system c) Superoxide anion, hydrogen peroxide, hydroxyl radical i) Major species prod. within cells (combine with NO to form reactive nitrogen species) d) Implicated in response in inflammation i) Endothelial cell damage, resulting in increased vascular permeability ii) Injury to other cell types (parenchymal cells, RBC’s), Inactivation of antiproteases (α1-antitrypsin) 8) Antioxidants a) Superoxide dismutase: Found or activated in variety of cell types b) Catalase: Detoxifies H202 c) Glutathione peroxidase: Powerful H202 detoxifier d) Ceruloplasmin: Copper-containing serum protein e) Serum Transferrin: Iron-free ffraction 9) Plasma Protein-Derived Mediators a) THREE INTERRELATED sytems! i) Complement, Kinin, Clotting Systems Inflammation Functional Categories of COMPLEMENT C3a, C5a – Stim. Histamine release (mast cells), Inc. Vascular Permeability, Cause Vasodilation **Anaphylatoxins** Phagocytosis C5a – Powerful Chemotactic Factor (Neurtophils, Monocytes, Eosinophils, Basophils) – Activate lipoxygenase pathway of AA metabolism in neutrophils/monocytes (Inc. Inflamm. Response) C3b, iC3b (inactive) – Fixed to Microbial act as opsonins Promote phagocytosis by neutrophils/macrophages Deposition of MAC on cells (Cells permeable to water and ions Cell Death by lysis Cell Lysis ii) C3a/C5a (1) Most important inflammatory mediators (cleaved by several enzymes present in inflammatory exudate) (a) Plasmin, Lysosomal enzymes released from neutrophils (Self-perpetuating cycle of neutrophil recruitment) b) Coagulation/Kinin Systems i) Culminate in activation of THROMBIN and Formation of FIBRIN ii) Intrinsic Clotting Pathway (1) Series of Plasma Proteins (2) Activated by Hageman Factor (Factor XII) – synthesized in liver, circulates in inactive form (activated upon contact with negatively charged surface) iii) Kinin Casacade (1) Active form of Factor XII (Factor XIIA) (a) Converts plasma pre-kallikrein into active form (kallikrein) (b) Kallikrein then cleaves kininogen to produce BRADYKININ (2) Bradykinin (a) Increase Vascular Permeability, Contracts SM’s, Dilates BV’s, Causes Pain when injected into Skin (b) SHORT lived – quickly inactivated by kininase 1) Activated Hageman factor (factor XIIa) a) Initiates four systems (inflammatory response) i) Kinin system (1) Produces Bradykinin ii) Clotting system (1) Induces formation of thrombin iii) Fibrinolytic system (1) Produces plasmin (Lyse Fibrin Clots, Cleave C3 C3 fragments, Degrade Fibrin to Fibrin Split Products) (2) Degrades fibrin to produce fibrinopeptides iv) Complement system (1) Produces anaphylatoxins and other mediators Inflammation 1) Outcomes of Acute Inflammation a) Complete Resolution (Usual Outcome – Injury limited/short-lived, little tissue destruction, parenchymal cells can regenerate) i) Restoration of site to normal: Removal of cellular debris/microbes by macrophage, resorption of edema fluid by lymphatic b) CT Replacement (Fibrosis) i) Substantial Tissue Destruction (Inflamm. of Tissues incapable of Regeneration, Abundant fibrin exudation in tissues or serous cavities that can’t be adequately cleared) ii) CT grows in damaged area – converts it into a mass of fibrous tissue c) Progression to Chronic Inflammation i) May follow acute, may be chronic from onset ii) Acute Chronic (1) Acute Inflamm. Response can’t be resolved (a) Persistance of Injury, Interference with normal healing (Bacterial infection in lung – Acute inflamm. (pneumonia) Extensive Tissue destruction & formation of cavity = Chronic Lung Abscess) \ Serous Inflammation Outpouring of Thin Fluid (From plasma/secretions of mesothelial cells) – Peritoneal, pleural, and pericardial cavities (accumulation of fluid in these cavities = effusion) Skin Blister – Burn or Viral Infection Serosanginous Effusion of Bilateral Pleural Cavities Chylous inflammation of peritoneal cavity Serous Effustion of R Pleural Cavity Vascular Leaks are large, Pro-coagulant Stimulus (Cancer Cells), Lining Body Cavities (meninges, pericardium, pleura) Fibrinous Inflammation Fibrinous Exudate (Eosinophilic meshwork of threads, amorphous coagulum), removed by fibrinolysis and clearing of other drbeis by macrophages Fibrin not removed – Stimulates ingrowth of fibroblast/BV’s (scarring) Suppurative Inflammation “Bread & Butter” – Fibrin Strands Fibrinous Pericarditis Large amounts of purulent exudate (Neutrophils, Liquefactive Necrosis, Edema Fluid, Bacteria produces localized suppuration“pyogenic-pus producing” Ex: Acute Appendicitis Suppurative Inflammation of the alveolar space Suppurative Inflammation of the Meningal Space Suppurative Inflammation of Pericardial Cavity Abscesses Suppurative Inflammation Localized Collection of purulent inflammatory tissue (buried deep in a tissues, organ or confined space), produced by deep seeding pyogenic bacteria Central Region – mass of necrotic leukocytes and tissue cells High Power of Slide to the Right: Marked Acute Inflammation within Abscess Cavity Ulcers Necrotic Focus – Around it (zone of preserved neutrophils) Outside it (vascular dilation and parenchymal/fibroblast proliferation) Local Defect or Excavation of the surface of an organ or tissue (produced by sloughing of inflamed necrotic tissue) Most Common: Mouth, Stomach, Intestines, Genitourinary Tract, Skin of Lower Extremities Stomach Ulcer Chronic Duodenal Ulcer Chronic Inflammation 1) Prolonged Inflammation (weeks or months) – may follow acute or begin insidiously a) Causes i) Persistent Infections by micro-organisms (Mycobacteria, certain viruses, fungi, and parasites, Delayed Type Hypersensitivity) ii) Immune Mediated Inflammatory Disease iii) Autoimmune Diseases iv) Artherosclerosis (Chronic Inflammatory process of arterial wall – induced by endogenous toxic plasma lipid components) b) Morphology i) Infiltration with mononuclear cells (macrophages, lymphocytes, plasma cells – think CHRONIC (“clock face” with eccentric nucleus)) ii) Proliferation of small blood vessels (angiogenesis) iii) Fibrosis The * = collection of chronic inflammatory cells, Triangles indicate destruction of parenchyma (normal alveoli replace by spaces), Arrows indicate replacement by connective tissue (fibrosis) c) Cells in Chronic Inflammation i) Mononuclear Phagocyte System (AKA Reticuloendothelial System) (1) Closely related Cells of Bone Marrow Origin (a) Mononuclear Phagocytes (i) Arise from common prescursor in the BM – give rise to BLOOD Monocytes 1. Monocytes migrate from blood Tissues (half-life ~1 day) a. Emigrate into tissues during early acute inflammation (predominate cell type within 48 hours) 2. Differentiate into macrophages (life span of tissue macrophage several months to years) a. Transformation activated by microbial products, cytokines, other chemical mediators (b) Tissue Macrophages (i) Scattered through CT, Liver (Kupffer Cells), Spleen, Lymph Nodes, Lungs, CNS (Microglia) (2) THE MACROPHAGES (a) Activation of Macrophages (i) Increased levels of lysosomal enzymes and reactive oxygen/nitrogen species (ii) Production of cytokines, growth factors and other mediators of inflammation (b) Products of Activated Macrophages (i) Eliminate injurious agents, initiate repair, responsible for TISSUE injury in chronic inflammation (c) TISSUE DESTRUCTION = HALLMARK OF CHRONIC INFECTION!! ii) Lymphocytes iii) Plasma Cells (1) Develop from activated B lymphocytes (produce Ab’s) - against persistent foreign or self Ag’s iv) Eosinophils (1) Abundant in Immune reactions (mediated by IgE), parasitic infections (2) Eotaxin: Chemokine that recruits Eosinophils (3) Granules (Major Basic Protein) (a) Toxic to Parasites, lysis of mammalian epithelial cells (b) Contribute to tissue damage in immune reactions (allergies) v) Mast Cells (1) Widely distributed in CT’s (In Acute & Chronic Inflammatory Responses) (2) Degranulation/Release of Mediators (a) Histamine, Prostaglandins (b) Allergic Reaction to foods, insects, venom or drugs – catastrophic results (anaphylactic shock) 2) Granulomatous Inflammation a) Distinctive pattern of chronic inflammation – attempt to contain an offending agent that is difficult to eradicate i) Strong activation of T-lymphocytes Macrophage activation (injury to normal tissues) b) Most Commonly Seen In i) Tuberculosis, Sarcoidosis, Cat-scratch disease, Lymphogranuloma inguinale, Leprosy, Brucellosis, Syphilis, Mycotic infections, Berylliosis c) Morphology i) Microscopic aggregation of macrophages – transformed into epithelium like cells, surrounded by a collar of mononuclear leukocytes (lymphocytes, occasionally plasma cells) d) Granuloma i) Epitheliod Cells (1) Pale Pink Granular Cytoplasm, indistinct cell boundaries (2) Fuse to Form Giant Cells – periphery or center of granulomas ii) Types (1) Foreign Body Granuloma (a) Incited by relatively inert foreign bodies (sutures, talc-IV drug users) (b) Foreign Body can be identified in center of granuloma – refractile (2) Immune Granulomas (a) Caused by a variety of agents capable of inducing cell-mediated immune response (i) Granuloma produces when inciting agent is poorly degradable or particulate (b) Prototype – caused by infection with Mycobacterium tuberculosis (i) Granuloma referred to as tubercle (ii) Presence of central caseous necrosis (RARE in other granulomatous diseases) Caseous Granuloma (Cells dying, becoming degraded) Non-caseous Granuloma (Cells present) 3) Systemic Effects of Inflammation a) Acute-Phase Response i) **AKA systemic inflammatory response syndrome** ii) Reactions to cytokines whose prod. is stimulated by bacterial products iii) Clinical/Pathological changes (1) Fever (Elevated 1-4 degrees) – One of MOST prominent manifestations (response to pyrogens) (2) “Symptoms”: Increased Pulse/BP, Decreased Sweating (blood flow directed to deep vascular beds), Rigor (Shivers), Chills, Anorexia, Somnolence (3) Acute Phase Proteins (a) Plasma Proteins, Synthesized in the Liver, Concentrate in plasma in response to inflammatory stimuli (b) Three best known proteins (i) C-reactive protein (CRP) (ii) Fibrinogen (iii) Serum amyloid A (SAA Protein) (4) Leukocytosis (a) Esp. common to inflammatory reactions induced by bacterial infections (Leukocyte count usually climbs to 15000 – 20000 cell/microliter) (b) May reach crazy high levels (40000 – 100000 cells/microliter) (i) Leukemoid Reaction – similar to WBC counts observed in leukemia (c) Accelerated Release of cells from BM (Rise in number of immature neutrophils in blood) (5) Bacterial Infections : Increase in Blood Neutrophil Count (6) Viral Infections (Infectious Mono, Mumps, and German Measles) : Absolute increase in number of lymphocytes (7) Bronchial Asthma, Allergy, Parasitic Infestations (Absolute increase in eosinophils) (8) Infections (Typhoid fever and viruses, Rickettsiae, and certain protozoa: Decrease in circulating WBC’s b) Consequence of Defective or Excessive Inflammation i) Defective (1) Increased susceptibility to infections (2) Delayed wound healing ii) Excessive (1) Basis of many types of human disease (2) Allergies (disorders in which fundamental cause of tissue injury is inflammation)