Audio: National blood services act Promoting blood donation

Audio:
1.
National blood services act a.
Promoting blood donation, regulating blood banks, provides penalties b.
Philippines (1994) - a lot of commercial blood banks cutting corners - no Hepa B screening; no history
2.
Declaration of policy a.
Backbone of what's happening today b.
Promote encourage voluntary blood donation c.
Instill public consciousness that donation is a humanitarian act i.
Encourage blood donors - helping someone, countrymen d.
Blood donation is a professional medical service, not a sale of commodity e.
Adequate safe, affordable, equitable distribution of blood supply f.
Inform public for the need for donation to curb hazards of commercial sale g.
Teach benefits and rationale voluntary blood donation i.
Start at the early age - schools (pisay has a curriculum for blood donors) h.
Mobilize all sectors of community i.
Mandate DOH to establish a network i.
Not depend on family ii.
Hospitals interconnected to a particular hospital for blood supply j.
Provide adequate assistance k.
Require blood banks to operate on a non-profit basis l.
Establish scientific and professional standards i.
Standardized criteria, machines m.
Regulate and ensure safety of activities n.
Require upgrading of blood banks i.
Upgrade machines for patient safety
3.
Donor selection - very stringent a.
Target groups i.
Healthy individuals
1.
Before, only men (pregnancies no longersexceptions )
2.
Encourage regular donation
3.
Emphasize humanitarian values
4.
Blood donors given the highest regard ii.
Good general health
1.
Free of major organ diseases or cancer iii.
Pre-donation interview, education and counseling
1.
Introduction
2.
Confidentiality a.
Even families
3.
Information a.
Risk of giving blood b.
Blood tests and reasons why i.
Hepa B screen, HIV screen c.
Steps to be followed d.
Healthcare during and after donation i.
Puncture site e.
Provide necessary leaflets, information sheets etc.
i.
Concise and complete; encourage future donations b.
Donor screening process - one of the most important steps i.
Elements of medical history and physical examination
1.
Medical history
2.
Physical examination a.
Done by qualified physician b.
Limited; done on the same day - determine if giving blood can harm donor or recipient c.
Ensures privacy i.
Auditory and visual privacy ii.
Always apprehensions
Females allowed to have a companion iii.
Time for necessary discussion or explanation ii.
Self-administered donor forms
1.
Medical declaration form
2.
Filled up by donor - yes or no
3.
Specific; small; very detailed questions;
4.
Ensures safety for donor and recipient iii.
Between 18-65 iv.
Below 18, with parental consent v.
Take pulse vi.
Take blood pressure
1.
Not hypertensive, no hypotension vii.
Take temperature viii.
Take hemoglobin -before test
1.
Taking blood from someone with low levels will push her towards anemia
2.
Those with low levels will be referred to physicians ix.
Donation interval
1.
Whole blood 200 ml - 8 weeks
2.
Whole blood 400 ml - 12 weeks
3.
Infrequent plasmapheresis - 4 weeks
4.
Leukapharesis - x.
Pregnancy
1.
Nine months after childbirth or 3 months after weaning whichever is longer xi.
Skin lesions - anti-cubital area (research) xii.
Infectious diseases
1.
Piercing - 12 months after piercing
2.
STD - 12 months after cured b
3.
Defer indefinitely a.
Viral hepatitis b.
Reactive test for..
4.
Malaria after 3 years after treatment a.
According to AAB, 3 years with qualifiers b.
Those who come from malaria areas - 12 months
5.
Immunization and vaccination a.
Category 1 attenuated viral bacterial vaccines - 1 year after vaccination xiii.
Drugs - propose new questions
1.
Marijuana - can still donate
xiv.
Drug therapy - vary depending on drug
1.
Based on Australian red cross a.
Aspirin causes platelet dysfunction xv.
Persons who cannot be allowed to donate
1.
Autoimmune disease (SLE)
2.
Cardiovascular disease
3.
Severe lung disorder
4.
Prostitutes (high risk occupations) xvi.
Deferring and rejecting
1.
Rejection - Filipinos feel like they blood are dirty (groups C and B) - do not tell them they are rejected - connotation
2.
Deferred - careful explanation and wording - can still be allowed to donate later on
3.
Document all of this c.
Blood groups - a hundred groups documented in humans i.
ABO, Rh - common, major ii.
Bombay - rarest blood group documented iii.
Important in choosing blood to be transfused -
1.
ABO - first to be identified (transfusion since middle ages) a.
Presence of A and B antigen b.
H substance - precursor of A and B c.
Anti A and Anti B - isoagglutinins d.
Forward typing - use antigen to determine body type e.
Back typing - antigen for agglutination f.
Antigen A and B - clumping; O, no clumping
2.
Rh - second most important a.
No defined function i.
E/e, D, C/c ii.
Inherited as haplotype iii.
Presence of D antigen - Rh positive iv.
E/e - autoimmune hemolytic anemias v.
Exposure of Rh negative to RH: production of anti-d alloantibody - leads to immune mediated hemolytic anemia d.
Principals of clinical transfusion practice i.
Not the cure; just part of management ii.
Prescribing based on national guidelines (DOH) iii.
Look foe things minimizing blood loss iv.
Those with acute blood loss should receive effective resuscitation v.
hemoglobin value should not be sole consideration
1.
Clinical signs, symptoms
2.
Clinician should be aware of risks
3.
Prescribed when benefits outweigh costs
4.
Record reason for tranfusion
5.
Train person to monitor vi.
Checklist for clinician
1.
Every patient - think of them as your family, consider implications e.
Blood components i.
Whole blood: 6 components
1.
Platelet rich plasma a.
Platelet concentrate b.
Fresh frozen plasma c.
Cryoprecipitate d.
Cryosupernate
2.
RBC ii.
Whole blood - contains all blood components
1.
After 24 hours, no longer fresh; becomes red cells suspended in a protein
2.
Contents a.
Red cells b.
Plasma volume i.
Stable coagulation factors
3.
Packed RBC a.
Longer survival than whole blood (42 days depending on anitcoagulant preservative) b.
Red cell
4.
Platelet concentrates - from whole blood or PRP a.
Contains platelets and small amount of plasma
5.
Fresh frozen plasma (FPP) - can be stored for 5 years a.
Processed into albumin and or imune globuline
6.
Cryoprecipitate antihemophilic factor - can be stored for a year iii.
Pediatric age group - 2 groups (neonates and older infants)
1.
Almost same guidelines iv.
Indication for transfusion
1.
Restore oxygen carrying capacity to meet tissue demands
2.
Whole blood: a.
Used for patients with massive hemorrage (25% total blood volume loss) i.
How do you know if its 25%? - physical exam (cardiac rate, blood pressure - indications for hypertension) b.
Not indicated for those with chronic anemia (increase of red cell is slow; body increases plasma volume, hemoglobin decreases; push patient into volume overload or congestion; it should be packed RBC) and incipient cardiac failure
3.
Packed red cell a.
Adult - same as whole blood b.
Pedia - added guidelines; clinical manifestations of patient and hemo levels taken into consideration
4.
Platelet concentrate - hard to determine a.
Lower the platelet count, higher risk for spontaneous bleeding (20K lower limit) b.
Bone marrow failure, bleeding - give platelet concentrate c.
Low platelet, and clinical manifestation - transfusion d.
Generally avoided for prophylaxis unless warranted by emergency situations e.
Not indicated for thromobocytopenia - treat first, because patient may recover; sepsis does not warrant for platelet concentrate
5.
Fresh frozen plasma - for deficiency a.
Severe clotting deficiency
b.
Dilutional coagulapathy and bleeding c.
Not indicated for nutritional support, volume expansion, wound healing; but some doctors in the province continue this practice
6.
Cryoprecipitate a.
Alternative to factor 8 concentrate for inherited deficiencies i.
Not generally considered for factor 8 deficiency ii.
Why? US they have specific factor 8 concentrate - in the Philippines, it is very expensive, use cryoprecipitate iii.
Factor 8 concentrate first, then cryoprecipitate
7.
Time limits for infusion a.
Whole blood - 4 hours b.
Platelet concentrate, the rest - 20 minutes
8.
Red cell transfusion a.
Same type to patient b.
There must be ABO and Rh compatibility i.
Cross-match for incompatibilities ii.
Group AB - AB, also from A, B, O - order increasing immunogenicity
(reaction to different types)
9.
Plasma transfusion - different matches
10.
Compatibility label, checking blood pack (check for leakages, hemolysis (rbc should be pink), clots in plasma (contamination))
11.
Final identity check - most common cause of transfusion reactions: giving blood to the wrong patient
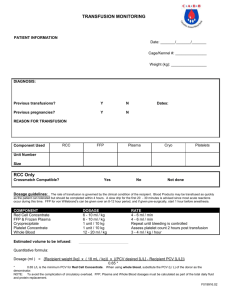
4.
Monitoring the transfused patient a.
Reactions most common in first 15 minutes - even irritability is a reaction b.
Warming of blood - done in the province i.
No evidence that warming blood is beneficiary ii.
It must never be heated in a bowl of warm water iii.
Cold blood may be a contributing factor in cardiac arrest
5.
Transfusion reaction a.
Immediate effects (3 days to 10 days) b.
Delayed effects c.
Manifestations: i.
Fever, chills, BP changes d.
Reactions i.
Mild ii.
Moderate-severe
1.
Collecting urine - urine bilirubin - hemolytic reaction occurring intramuscularly
iii.
Life-threatening
Questions: o Role of urine bilirubin (negative reaction)
Hemolytic transmission reaction
Bilirubin - conjugated to unconjugated (lipid-soluble) - goes to liver; glycosylation for conjugation to become water-soluble - increased amounts then spills into urine
Indicates massive intravascular accumulation of bilirubin