reader`s question - Spectrum MRI Imaging Center, Inc.
advertisement
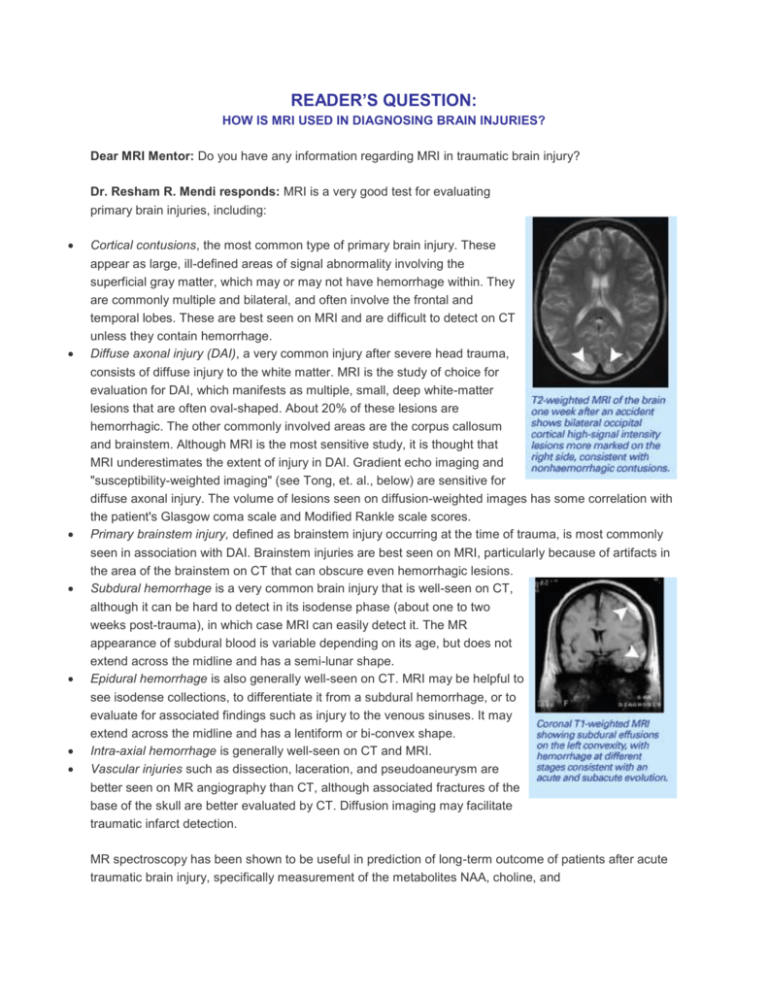
READER’S QUESTION: HOW IS MRI USED IN DIAGNOSING BRAIN INJURIES? Dear MRI Mentor: Do you have any information regarding MRI in traumatic brain injury? Dr. Resham R. Mendi responds: MRI is a very good test for evaluating primary brain injuries, including: Cortical contusions, the most common type of primary brain injury. These appear as large, ill-defined areas of signal abnormality involving the superficial gray matter, which may or may not have hemorrhage within. They are commonly multiple and bilateral, and often involve the frontal and temporal lobes. These are best seen on MRI and are difficult to detect on CT unless they contain hemorrhage. Diffuse axonal injury (DAI), a very common injury after severe head trauma, consists of diffuse injury to the white matter. MRI is the study of choice for evaluation for DAI, which manifests as multiple, small, deep white-matter lesions that are often oval-shaped. About 20% of these lesions are hemorrhagic. The other commonly involved areas are the corpus callosum and brainstem. Although MRI is the most sensitive study, it is thought that MRI underestimates the extent of injury in DAI. Gradient echo imaging and "susceptibility-weighted imaging" (see Tong, et. al., below) are sensitive for diffuse axonal injury. The volume of lesions seen on diffusion-weighted images has some correlation with the patient's Glasgow coma scale and Modified Rankle scale scores. Primary brainstem injury, defined as brainstem injury occurring at the time of trauma, is most commonly seen in association with DAI. Brainstem injuries are best seen on MRI, particularly because of artifacts in the area of the brainstem on CT that can obscure even hemorrhagic lesions. Subdural hemorrhage is a very common brain injury that is well-seen on CT, although it can be hard to detect in its isodense phase (about one to two weeks post-trauma), in which case MRI can easily detect it. The MR appearance of subdural blood is variable depending on its age, but does not extend across the midline and has a semi-lunar shape. Epidural hemorrhage is also generally well-seen on CT. MRI may be helpful to see isodense collections, to differentiate it from a subdural hemorrhage, or to evaluate for associated findings such as injury to the venous sinuses. It may extend across the midline and has a lentiform or bi-convex shape. Intra-axial hemorrhage is generally well-seen on CT and MRI. Vascular injuries such as dissection, laceration, and pseudoaneurysm are better seen on MR angiography than CT, although associated fractures of the base of the skull are better evaluated by CT. Diffusion imaging may facilitate traumatic infarct detection. MR spectroscopy has been shown to be useful in prediction of long-term outcome of patients after acute traumatic brain injury, specifically measurement of the metabolites NAA, choline, and glutamate/glutamine. MRI is also a good test for evaluating secondary traumatic injuries to the brain, such as infarction, herniation, and ischemia. I hope this was helpful to you. Thank you for your question. For further reading on this topic, see: Tong, K.A., Ashwal, S., Holshouser, B.A., Shutter, L.A. Herigault, G., Haacke, E.M. and Kido, D.K. “Hemorrhagic Shearing Lesions in Children and Adolescents with Post-Traumatic Diffuse Axonal Injury: Improved Detection and Initial Results.” Radiology 2003; 227: 332-339. Gentry, L.R. “Imaging of Closed Head Injury.” Radiology 1994; 191: 1-17. Schaefer, P.W., Huisman, T., Sorensen, A.G., Gonzalez, R.G., and Schwamm, L.H. “Diffusion-Weighted MR Imaging in Closed Head Injury: High Correlation with Initial Glasgow Coma Scale Score and Score on Modified Rankin Scale at Discharge.” Radiology 2004; 233: 58-66. Ross, B.D., Ernst,, T., Kreis, R., Haseler, L.J., Bayer, S., Danielsen, E., Blüml, S., Shonk, T., Mandigo, J.C., Caton, W., Clark, C., Jensen, S.W., Lehman, N.L., Arcinue, E., Pudenz, R., Shelden, C.H. “1H MRS in Acute Traumatic Brain Injury.” Journal of Magnetic Resonance Imaging, Volume 8, Issue 4, July/August 1998: 829-840 Shutter, L., Tong, K.A., Holshouser, B.A. “Proton MRS in Acute Traumatic Brain Injury: Role for Glutamate/Glutamine and Choline for Outcome Prediction.” Journal of Neurotrauma, 2004, 21(12): 16931705. Herskovits, E.H., Gerring, J.P., Davatzikos, C., and Bryan, R.N. “Is the Spatial Distribution of Brain Lesions Associated with Closed-Head Injury in Children Predictive of Subsequent Development of PostTraumatic Stress Disorder?” Radiology 2002; 224: 345-351.