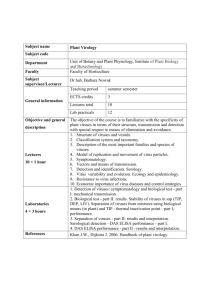
01_virology-cell-cultures
advertisement

Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Authors: Prof Estelle Venter Licensed under a Creative Commons Attribution license. TABLE OF CONTENTS INTRODUCTION........................................................................................................................................... 3 Terminology ............................................................................................................................................. 3 SAFETY IN THE LABORATORY ................................................................................................................. 5 CELL CULTURE LABORATORY ................................................................................................................ 6 Basic requirements .................................................................................................................................. 7 Cleaning of tissue culture items ............................................................................................................... 8 CELL CULTURE PROCEDURES .............................................................................................................. 10 Cell culture media .................................................................................................................................. 10 Basic salt media ..................................................................................................................................... 10 Tissue culture technique ........................................................................................................................ 15 Sub-culturing of cell lines ....................................................................................................................... 21 Quantification of cells ............................................................................................................................. 23 The use of different cell cultures ............................................................................................................ 24 Contamination of cell cultures ................................................................................................................ 27 Cryopreservation .................................................................................................................................... 28 Demonstration / confirmation of the presence of viruses in infected cell cultures ................................. 30 Viral quantification .................................................................................................................................... 42 Infectivity assays for viruses .................................................................................................................. 42 1|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Dose response curve and significance of ID50/TCID50 ........................................................................... 42 Plaque assay.......................................................................................................................................... 44 STORAGE OF ANTIGEN ........................................................................................................................... 46 Frequently Asked Questions ................................................................................................................... 47 2|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures INTRODUCTION Viruses cannot reproduce independently of living cells. For many years viruses were grown in natural hosts, embryonated chicken eggs and laboratory animals. Currently many viruses are grown in monolayers of animal cells. This technique was made possible by the development of growth media for animal cells and the advent of antimicrobial drugs that can prevent bacterial and fungal contamination. Terminology In vitro tissue culture: Tissue culture is commonly applied as a generic term that encompasses, and is concerned with, the study of cells, tissues and organs maintained and grown in vitro. Culture systems can be grouped into the following main categories based on their degree of complexity and related in vivo topography: Tissue culture: sometimes used as a specific term to denote the maintenance or growth of tissue fragments in vitro. The original or characteristic architecture, and often the biochemical properties associated with it, are not necessarily maintained. Cell culture: denotes the maintenance and culture of cells in vitro including the culture of a single type of cell. In cell cultures, the cells are no longer organized into tissues and are, therefore, usually devoid of their histiotypic architecture and often of the biochemical properties associated with it. Cells are cultured either as adherent mono- or multilayers on a solid substrate, or as a suspension in culture medium. Some cells will grow in free suspension if mechanically agitated; otherwise they will grow attached to the substrate. Primary culture: cells derived directly from a particular organ or tissue. All such cultures are considered primary until the first successful subculture, after which they become a serial culture. Such cultures are usually heterogeneous and largely representative of the tissue from which they were derived. Serial cultures, in which growth of a single histological cell type has been selected for, are termed cell lines. These may be of continuous, established or finite nature. Continuous cell lines are populations of cells within serial cultures which are apparently capable of an unlimited number of population doublings and are often referred to as immortal cell lines. Such cell lines may or may not express the characteristics of in vitro neoplastic or malignant transformation. Established cell lines: A cell line in which the potential to be sub-cultured indefinitely in vitro has been demonstrated. Finite cell cultures or cell lines are capable of only a limited number of population doublings after which the cells cease to proliferate. Both finite cell lines of sufficient doubling potential and continuous cell lines can be propagated, expanded to produce large numbers of aliquots with characterized and defined cell populations, and then preserved for future use by freezing. 3|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Explant: An excised fragment of a tissue or organ used to initiate an in vitro culture. Monolayer: A single layer of cells growing on a surface (substrate). Suspension culture: A culture arising from the passage of a primary culture. Diploid cell line: A cell line in which, arbitrarily at least 75% of the cells have the same karyotype as the normal cells of the species from which the cells were originally obtained. Heteroploid cell line: A cell line having less than 75% of cells with a diploid chromosome constitution. Pseudo-diploid cell line: A cell line in which the cells have the same number of chromosomes sets as the normal cell of the species from which the cells were obtained, but which possess an altered karyotype. Cell strain: A cell strain can be derived either from a primary culture or cell line by the selection or cloning of cells having specific properties or markers. The properties of markers must persist during subsequent cultivation. Sub-strain: A sub-strain can be derived from a strain by isolating a single cell or group of cells having properties or markers not shared by all cells of the strain. Clone: A population of cells derived from a single cell. Cloned strain or line: A strain or line descended directly from a clone. Passage: The transplantation of cells from one culture vessel to another. Split: Synonymous with “passage”. Subculture: Synonymous with “passage”. Subculture (passage) number: The number of subcultures the line has undergone, from the primary material to the culture in question. This term is loosely synonymous to generation number. Fibroblasts: Cells of spindle or irregular shape which, as their name implies are responsible for fibre formation. Fibroblast-like cells: In cell cultures various types of cells acquire a similar morphology. Cells acquiring an irregular or spindle shape are often referred to as “fibroblasts”. However, their derivation or potentialities, such as production of fibers, are usually not known. Such cells are then called “fibroblast-like” Epithelial cells: Cells opposed to each other, forming mosaic-like sheets with very little intercellular substance, as seen in vitro or in tissue or organ culture. Epithelial-like cells: In cell cultures epithelial cells may assume various shapes to form sheets of closely adherent polygonal cells. The degree of cohesion of the cells can vary. 4|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Transformation: Often used synonymously with “cell alteration”. It is recommended that this term is used only for heritable changes, such as those brought about by the action of various viruses and chemicals. SAFETY IN THE LABORATORY Micro-organisms may enter a laboratory in diagnostic specimens. Excretions, secretions, blood, serum, tissues and cell cultures may be infectious, particularly, but not only when they are derived from sick animals. In order to infect a laboratory worker, an agent must gain access to the body by inhalation or ingestion, or through broken skin, the conjunctiva or other mucous membranes. Aerosols: Infectious agents may become aerosolized by spillage or breakage of containers and centrifuge tubes or through the use of high speed blenders. Aerosols may occur on opening evacuated blood collection tubes, specimen containers, and culture tubes or when a needle is withdrawn e.g. from a stoppered vaccine bottle. Aerosols may also occur when using pipettes, by applying a hot inoculating loop to a culture, and by expelling air bubbles from syringes containing infectious agents. In tissue cultures some cell types do generate gas during their normal metabolism which can cause aerosols of infectious agents to develop when tubes or other containers are opened. Larger droplets fall and may contaminate the underlying surfaces. suspended in the air for considerable periods and inhaled. Small particles may remain Eyes: May be infected by aerosols, splashing or rubbing with an infected finger resulting in conjunctival and/or corneal infections. Oral infection can result from the dangerous technique of mouth-pipetting, from smoking, eating or drinking in the laboratory, or from unwashed contaminated hands. Skin: Injuries from needles, broken glassware and scratches or bites of laboratory animals may serve as portals of infection for viruses such as hepatitis virus, rabies virus and arboviruses. The skin can directly be infected by dermotropic viruses, e.g. vaccinia. Vectors: Mosquitoes, ticks, fleas, mites, and other ectoparasites are potential sources of laboratoryacquired infection unless properly controlled or contained, whether they are being used in experimental work or just happen to be present on animals or in material brought into the laboratory. High risk pathogens: Any diagnostic virology laboratory must maintain sufficiently high safety standards to avoid danger in the event that a specimen, probably unrecognized, happens to contain one of the pathogens of high risk. For practical purposes the following may be regarded as the ‘Category A Pathogens’ primarily dangerous to man: the haemorrhagic fever viruses (Lassa fever virus, Marburg virus, Ebola fever virus and Crimean-Congo fever virus), rabies virus, simian herpes B virus and smallpox virus. Routine diagnostic laboratories are unlikely to have the techniques and equipment required to safely handle and identify these viruses, and when one or more of them is suspected the investigation should immediately be transferred to an approved reference laboratory for testing. Nevertheless, if the diagnostic laboratory is liable to receive specimens containing dangerous pathogens, it is useful to have a small room away from the main laboratory activities in which they can 5|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures be managed. This room must have facilities for controlled access and entry through an airlock with changing and washing facilities, and be provided with an exhaust protective cabinet, filtered exhaust ventilation and minimal essential equipment for work with potentially high-risk materials, e.g. preparation of electron microscope grids and the setting up of other tests. Dangerous chemicals: Dangerous chemicals fall into several categories. Special care must be taken in handling or storing large quantities of these materials, and all containers must be clearly and properly labelled. Caustic or corrosive compounds Included in this category are acids or bases, which may burn or otherwise damage the skin or other human tissue. Such compounds may also cause corrosion of equipment. Poisons This category includes substances that are sufficiently poisonous that the inhalation or ingestion of relatively small amounts of them may induce serious deleterious effects or death. Poisons may be solid, liquid, or gaseous in nature. Flammables These include materials that easily ignite or burn, and serve as fuel for a fire. Explosives Although many explosive materials are also flammable, these compounds may explode under special conditions. They must, therefore, be handled in such a way as to eliminate exposure to, or attainment of, these conditions. Radioactive materials Only government approved laboratories may work with radioactive material. These laboratories are required to follow certain prerequisites, e.g. laboratory benches and floors must be covered with a specific type of material, storage space for radioactive material must be appropriate, and notices informing workers and others of the danger of radioactive material must be prominently displayed. Disposal of infected materials: No infected material should leave the laboratory except as properly packaged samples sent to other laboratories. It is the responsibility of the laboratory staff to ensure that no infected items reach the washing section of the department. CELL CULTURE LABORATORY The major item required by the cell culture scientist is a laminar flow cabinet or a sterile working hood. However, such cabinets should not be seen as an insurance policy against poor technique. A cabinet should be selected so that it has sufficient working space for manipulating the cell system being used. 6|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Remember that there must be room for media, sera, additive bottles, pipettes and measuring devices, provision for gassing cultures where necessary, room for storage of the culture vessels, plus an appropriate place for placing discards. Basic requirements Incubator: If bicarbonate buffering systems are to be used, an incubator containing CO2 is essential Inverted microscope Water baths: one at 37°C and the other at 56°C (for inactivating sera) Centrifuge – normally low speed Pipetting devices Filtration equipment - For filtering media Counting apparatus - Haemocytometer or Coulter counter, if cell counting is to be done Storage of cells - Tubes for storage, as well as an appropriate deep freezer or liquid nitrogen container Safety cabinets - Safety cabinets are either use to protect the substance which one is working with or the operator or both. Potential infectious material should always be handled where possible in a biohazard cabinet. Laminar flow cabinets: Creates a sterile environment for aseptic work Prevents contamination of culture media during pouring and tubing It should not be used for the following: Manipulation of pathogenic or hazardous substances Dispensing of tissue culture cells or any other living material; because even sterile culture cells may contain undetectable slow or oncogenic viruses, which are blown towards the operator’s face or into the room Biological safety cabinets: Mainly for protection of the operator working with, e.g. Pathogenic organism Highly concentrated biological agents known to be hazardous to humans, animals or plants Mutagens Low and moderate risk oncogenic viruses Functions: These cabinets are divided into different classes according to its way of functioning i.e. CLASS I, CLASS II and CLASS III biosafety cabinets. 7|Page Class I biosafety cabinet Applied Veterinary Virology: The isolation and identification of viruses using cell cultures A class 1 cabinet is an open-fronted, negative pressure (drawing air away from the operator), with a HEPA-filtered re-circulated air exhaust, which is suitable for class B agents (bacteria). The operator should always wear gloves. This cabinet is mainly for the protection of the operator against air borne infections. Class II biosafety cabinet A class II cabinet is a vertical-laminar flow cabinet with HEPA-filtered re-circulated airflow in the work area and HEPA-filtered air exhaust. These cabinets are useful for the containment of BSL 2 and 3 agents. This is of particular value in virological procedures, such as work with tissue cultures and embryonated eggs because it offers protection for both the operator and the work against contamination. Class III biosafety cabinet These are used mainly in level 4 or maximum containment Labs where very harzadous viruses are investigated. Class III cabinets are the ultimate in safety cabinet engineering; they are completely enclosed and air tight. The operator works through gloves fitted in the see through front window. Cleaning of tissue culture items General procedure for items that do not come into direct contact with cells All items should be soaked in disinfectant immediately after use Wash properly Rinse in tap water Rinse separately in fresh distilled water Air dry thoroughly Cover and assemble for sterilization; date of sterilization should be clearly marked General procedure for items that come into direct contact with cells Disposable plastic ware should be thrown into separate bags for autoclaving and decontamination Reusable glassware must be decontaminated in a disinfectant, e.g. chlorine solution, and then autoclaved Plastic ware Tissue culture flasks, plastic disposable pipettes, syringes, etc. Culture surface must be totally non-toxic and uniform. Pre-tested batches of disposable tissue culture flasks are generally used. 8|Page Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Table 1: Disposal of laboratory material Material Disposal route Specimen containers Plastic disposable Incinerator bucket incinerate Glass autoclave drumautoclave discard Laboratory glassware Bottles, tubes and vials Firmly closed autoclave drumautoclave recycle or discard Open tubes Upright in basket autoclave drumautoclave recycle Pyrex centrifugation tubes Immerse overnight in corox autoclave drumautoclave Electron microscope glassware recycle Broken glassware Plastic bag sealadditional wrapping and separate autoclavediscard Laboratory plastics Disposable: cellulose nitrate tubes, plastic Plastic bag seal incinerate haemagglutination and microtiter plates Recycle Soak in decon or coroxrinserecycle (radiation) Pipettes Glass Immerse in corox / decon washautoclave Plastic Plastic bag seal incinerate Rubber stoppers Cell culture stoppers Overnight in corox washcover with foil or autoclave plastic bagautoclave recycle Instruments Scissors, forceps, clamps, mortars and pestles, grinders, Immerse in water with corox or decon wash autoclave homogenizers recycle Uninfected tissue Placentas, kidneys, embryonic tissues Plastic bagsealincinerate Contaminated tissue PM specimens, inoculated egg material Seal in containerbagautoclavediscard Protective clothing Gowns Bagsclose securelylaunder Plastic aprons, gloves, etc. Plastic bag (sealed)incinerate Paper products Paper towels, tissue, etc. 9|Page Plastic bag (tie securely) incinerate Applied Veterinary Virology: The isolation and identification of viruses using cell cultures CELL CULTURE PROCEDURES Cell culture media Water: Water represents more than 99% of the material that comes into contact with cells whether as a medium ingredient, in the processing operation or as the final rinse of containers in which the cultures are grown. Purification methods that can be used are: Ion exchange: This involves the use of ion exchange resins for the removal of ionic impurities from water. Reverse osmosis: If a semi-permeable membrane, permeable to the solvent but not to the solute, is placed at an interface between two solutions of different solute concentrations, then solute transport is prohibited and a free energy difference due to the concentration gradient develops across the membrane. Under these circumstances solvent moves through the membrane from the low- to the high-concentration compartment, either until the concentration difference is zero, or until the hydrostatic pressure difference reaches equilibrium with the free energy driving force. The process is known as “osmosis” and the hydrostatic pressure difference which stops the net transfer of solvent is the osmotic pressure. Because it is in a thermodynamic equilibrium, if the pressure applied to the high-concentration side of the membrane is increased above the osmotic pressure, solvent molecules are driven against the concentration gradient. This process is termed “reverse osmosis”. Theoretically, reverse osmosis allows only water molecules to traverse the membranes, although in practice, polar ions up to a molecular weight of 100 can transfer. Molecular weights of 1000 or more are totally excluded, meaning that “reverse osmosis” water is invariably pyrogen-free. “Reverse osmosis” is the most suitable and economic primary system for the preparation of media and cleaning of equipment and glassware. Water purified by “reverse osmosis” has a very low organic content and a small ionic content. Normally a “reverse osmosis“ unit is linked to a water mains by a system incorporating a sealed storage tank (to which is attached a hydrophobic vent filter), a circulating pump, an ion exchange column, an in-line 0,45 μm filter cartridge (to protect an in-line UV system) and a 0,2 μm filter cartridge upstream of the purified water outlets. Distillation: This is the only method for producing water for critical pharmaceutical purposes. Distillation, although producing the highest quality water, is the most expensive method of treatment because of high capital and operational costs, and for that reason it is only appropriate for purifying water for the most critical applications. Basic salt media The culture medium is by far the most important single factor in culturing animal cells. The function of this medium is to provide an environment for survival and also to provide substances required by the cells which they cannot directly synthesize. The composition of early tissue culture media was based on biological fluids such as plasma, lymph and serum, and tissue extracts especially of embryonic 10 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures origin. Basal tissue culture media were developed to include only the minimal components which were essential for growth. Types of basal media: There are four main categories of basal media for mammalian cells and several categories for insect cells. These are: Eagle’s medium and derivatives, e.g. BME (basal medium Eagle’s), EMEM (minimum essential medium with Earle’s salts), AMEM (alpha modification of MEM), DMEM (Dulbecco’s modified Eagle’s medium), GMEM (Glasgow modification of Earle’s medium), and JMEM (Joklik’s modification of MEM) Media designed at Roswell Park Memorial Institute (RPMI), e.g. RPMI 1629, RPMI 1630, and RPMI 1640 Basal media designed for use after serum supplementation, e.g. Fischer’s, Liebovitz, Trowell, and Williams’ Basal medium designed for serum-free formulations, e.g. CMRL 1060, Ham’s F10 and derivatives, TC 199 and derivatives, MCDB and derivatives, NCTC and Waymouth For insect cell cultures, the basal media are: Grace’s medium Schneider’s medium Mitsuhashi and Maramorosch medium IPL-41 medium Chiu and Black medium D-22 medium Constituents of basal media Allowance is usually made for differences in salt concentration to obtain the optimum osmolality. Different incubation temperatures may also require adjustment to be made to the composition of buffering components, since pH may change with temperature due to alterations in the solubility of CO2 and in ionization and pKa of buffers. The following may be considered: Balanced salt solution Most of these solutions do not include nutrients required for most cells for long-term maintenance or growth although glucose may be included Earle’s balanced salt solution Dulbecco’s phosphate-buffered saline Hank’s balanced salt solution Eagle’s spinner salt solution 11 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Dulbecco’s phosphate-buffered saline and Hank’s balanced salt solution are intended for use equilibrated with air, while Earle’s balanced salt solution and Eagle’s spinner salt solution require equilibration with a gas phase containing 5% CO 2 in order to maintain the correct pH. Buffering systems: Phosphate buffering systems are normally used – see discussion below Energy source: Carbohydrates are a major energy source for cultured cells. Glucose is the most frequent used sugar. Other sugars, e.g. maltose, sucrose, fructose, galactose, and mannose, may also be included. Glutamine can also supply a major proportion of the required energy in some cells Amino acids: Most animal cells have a high requirement for glutamine. Glutamine acts both as an energy source and as a carbon source in the synthesis of nucleic acids. Other amino acids are often added to compensate either for a particular cell type’s incapacity to make them or because they are made but lost in the medium Vitamins: Several vitamins of the B group are necessary for cell growth and multiplication. Many vitamins are precursors for cofactors and must be added Hormones and growth factors: These are included in some media (especially serum free media) at relatively low concentrations Proteins and peptides. Although an absolute requirement for proteins and/or peptides by cells in culture has not been established, relatively few media have been formulated in which cells grow rapidly in the total absence of proteins or peptides Fatty acids and lipids: There is no consensus regarding an essential role for lipids in cell culture Accessory factors: Amongst these are the ‘trace’ elements, especially iron, zinc, copper, and selenium Antibiotics Buffering systems A phosphate buffer system is normally used provided by sodium and potassium phosphates, sodium bicarbonate, other natural ingredients such as sera, proteins, amino acids, as well as synthetic, organic molecules, such as HEPES (N-2-hydroxyethylpiperazine-N’-2-ethanesulfonic acid), TRIS (tris-hydroxymethyl-aminomethane), TRICINE (N-tris-(hydroxymethyl)- methylglycine), BES, (N,N’-bis-(2-hydroxy-ethyl)-2-aminoethanesulfonic acid) and others. Three or more of these are simultaneously used to control the pH in most cell culture media. The use of sodium bicarbonate, with or without CO 2 added to the gas phase of the atmosphere in which the cells are grown, significantly improves the buffering situation. The use of sodium bicarbonate, with or without CO2 added to the gas phase of the atmosphere in which the cells are grown, significantly improves the buffering situation. The interrelationship between the bicarbonate ion concentration in the medium, the pH and the partial pressure of carbon dioxide in the gas phase is important. Carbon dioxide gas is very soluble in culture media. A small proportion (less than 1%) combines chemically with water to form the weak carbonic acid which dissociates to yield hydrogen and bicarbonate ions. 12 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures H2O + CO2 H2CO3 H+ + HCO3Thus the acidity will gradually increase as the partial pressure of carbon dioxide is increased. Since sodium bicarbonate is a salt, it will dissociate virtually completely. The concentration of bicarbonate ion will be very close to that of the salt added. Additions from dissociation of carbonic acid or losses due to dissociation of bicarbonate to carbonate are negligible. Thus for a given temperature, one can predict the initial pH if the bicarbonate ion concentration and partial pressure of carbon dioxide are fixed. The levels of CO2 in the atmosphere in which cell culture systems are grown vary from that of ambient air (i.e. about 0,03%) up to 40%. Generally, either no CO2 is added or, alternatively, 5% to 10% CO2 is added to the atmosphere. Prophylactic use of antibiotics The prophylactic use of antibiotics in cells and tissues with a high risk of microbial contamination and in conjunction with aseptic techniques can considerably reduce the overgrowth of bacteria (including mycoplasmas) and fungi. The majority of antibiotics used for controlling microbial contamination of cell or tissue cultures are effective against both Gram-positive and Gram-negative bacteria. Gentamycin and ciprofloxacin exhibit activity against mycoplasmas, and the polyenes, amphotericin B and nystatin are useful in preventing contamination with yeasts and fungi (Wiedemann and Atkinson 1991). The combination of penicillin G at a concentration of 105 U/ℓ, streptomycin sulphate (100 mg/ℓ) has found wide application in preventing bacterial and fungal contamination in cell and tissue cultures. More recently gentamicin sulphate at a concentration of 50 mg/ℓ has been used as an alternative to streptomycin sulphate because of its activity against Pseudomonas species. This combination has been particularly useful in reducing the incidence of bacterial contamination in cell cultures used for isolating viruses from clinical samples. However, the use of gentamicin is not to be encouraged. Several factors should be considered when determining the most appropriate antibiotic or combination of antibiotics for use in cell or tissue culture. The antibiotic’s cytotoxicity and stability in cell culture media and its spectrum of antimicrobial activity should be determined. Also, the types of contaminants that may be encountered and interactions with other antibiotics should be considered. A list of antibiotics and their use can be found in Paul (1975), Schaffner (1979) and Gray & Brenwald (1991). One should always test the toxicity of the antibiotic to cell cultures before using the antibiotic. 13 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Serum Foetal bovine serum (FBS) is now most frequently used at 10% concentration although this may be changed for specific applications. Advantages of serum use include the following: • Serum represents a cocktail of most of the factors required for cell proliferation and maintenance • Serum is an almost universal growth supplement which is effective for most cells. Using serum-supplemented medium therefore reduces the need to spend time developing a specific, optimized medium formulation for every cell type under investigation • Serum buffers the cell culture system against a variety of perturbations and toxic effects, such as those due to pH change, or presence of ions of heavy metals, proteolytic activity, or endotoxin The use of serum also imposes a number of difficulties which impact on the safety, reproducibility, and cost of biopharmaceuticals produced in animal cells. These difficulties can be minimized by careful selection and validation of serum sources. Although almost all new manufacturing processes using animal cells are designed for serum-free media in order to avoid these difficulties, many existing processes still use FBS-supplemented medium. This situation is unlikely to change fundamentally in the near future since regulatory constraints generally make it impractical and uneconomical to alter existing processes. Potential problems with the use of serum There are a number of serious disadvantages incurred when serum is used to supplement a culture medium: • Lack of reproducibility. Serum batches vary considerably depending on such factors as the characteristic of the source animals used, the feed stuffs employed, and on the time of year. Different batches contain different absolute and relative levels of growth factors. Certain factors may be deficient in some batches, while others may be present at excessive, inhibitory levels for some cell types • Risk of contamination. Serum can represent a major route for the introduction into cultures of adventitious agents including bacteria, fungi, mycoplasmas, and viruses. Health checks on donor animals should be applied and the facilities used for the collection and processing of serum must be checked. Serum, after filtration, is checked for the presence of viruses. A standard quality control procedure should be applied • Influence on downstream processing. This is a problem in protein studies when proteins produced by the cell culture need to be harvested and purified. Serum proteins added may inhibit or influence this process because of their high concentration compared to the proteins of interest • Availability and cost. Correctly collected, processed, and validated FBS will always contribute greatly to the cost of a tissue culture laboratory 14 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Serum storage and use Serum is rapidly frozen by the supplier immediately after bottling and is thereafter held at – 20°C. Few data are available on the shelf life of serum held in this way, but 2 years has become accepted as a rule of thumb. However, one study indicated that 2 years at –20°C is a conservative estimate of shelf-life and that this could be extended to 5 years. When required, serum should be thawed rapidly during which process it is gently mixed to minimize protein denaturing due to salt concentration effects. A water bath at 37°C is best although the serum should be removed as soon as fully thawed and not allowed to warm up. Thawed serum should be clear and there should be no significant precipitation. Once thawed, it can be held at 4°C for a maximum of 2 - 3 weeks. Serum should not be re-frozen. Sterilization of cell culture media Sterilization of media is general done by filtration. Tissue culture technique Prevention of contamination by any extraneous organisms (bacteria, yeast, fungi, mycoplasmas, viruses) is a prerequisite in tissue culture. The basic principles of good technique are essentially common sense, but it is worth restating the obvious to ensure that the first principles are correct. Blanket antibiotic cover is to be avoided at all costs. Antibiotics have their place in case of “emergency” or in the early stages of primary isolation of cells from contaminated tissues. However, routine use of them in tissue cultures cannot be justified and should not be a “cover” for poor laboratory practices. Indiscriminate antibiotic use will inevitably lead to problems. Hidden infections can occur, which only become apparent during experimental or production procedures, and may render the cell line unusable for the particular purpose envisaged. Recommended procedures for handling cell lines (valid for all types of facility) Avoid multiple-use facilities, if possible Only handle one cell line at a time. Such a common-sense approach should cut to the minimum the possibility of miss-labelling, mix-ups, and cross-contamination between cell lines Examine cultures daily for evidence of cross-contamination Maintain separate bottles of media (and preferably other reagents) for each cell line Institute quality control procedures for all the reagents used in tissue culture even if purchased from a commercial supplier Keep the working areas uncluttered (consumable supplies should be kept in racks below the work area), swab with a suitable disinfectant between handling cell lines, and allow a minimum of time (15 min) between the handling of different cell lines Dispose of all used materials safely, efficiently and routinely If separate work areas are not available, at least designate separate incubators for different types of materials and carry out procedures done on a daily basis with quality controlled cultures before others 15 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Routine quality control procedures should be carried out more frequently in multi-use facilities Ensure that laboratory coats are regularly changed Wash hands thoroughly before and after commencing laboratory work. If possible, use sterile gloves Avoid the generation of aerosols (e.g. by too vigorous pipetting) in the work area Inside the safety cabinet liberal use of a disinfectant e.g. 70% ethanol) to swab work surfaces/bottles/flasks is recommended Train and monitor junior staff in tissue culture techniques before allowing them to handle particularly valuable material Maintain facilities efficiently Ensure that all incubators, microscopes, centrifuges and other equipment are clean and serviced regularly Discard unused cultures from incubators as soon as they are no longer required If laboratory topography and finance permit, install facilities which can be routinely fumigated Information used to describe a cell line or strain for publication History Population doubling number (subculture number) Culture medium used Growth characteristics Absolute plating efficiency Morphology Frequency of cells with various chromosome numbers in a culture Karyotype characteristic of the stem line Whether sterility tests for mycoplasmas, bacteria and fungi have been done Whether the species of origin of the culture has been confirmed A description of a cell strain should also include the procedure of isolation, the number of population doublings, and the length of time since isolation. Strategies for the derivation of primary cultures and establishment of cell lines Primary cultures are generally derived directly from a particular organ or tissue, although the use of whole embryos (e.g. chick) is common practice for some applications, e.g. virology. To achieve a successful primary culture depends on many factors, such as the species and the age of donor, but a major factor is the choice of tissue. Materials from mature or adult organisms are less reliable as a source of actively dividing cells than embryonic tissues. One notable exception is tumour tissue; but, this gives variable success. Some cell types, such as plasma cells, are the end product of a long sequence of differentiation events and are therefore unlikely to survive in culture. For this reason, embryonic tissue is a recommended source despite the fact that they may have different characteristics from adult cells, and may not ever mature. 16 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Once the primary culture has been established, successful subculture to generate a cell line is usual, and allows the possibility of cloning, characterization and preservation, and thus greater uniformity. It should be remembered that cells from a primary vertebrate culture usually have a finite lifespan dependent on the species. In order to overcome this, and generate an immortal cell line, a transformation event must occur, either as a natural somatic mutation or as an induced event (in vivo or in vitro). The method of tissue dissociation will be dependent upon the type of tissue and the long-term purpose of the culture. In some tissues, like spleen, the cells are loosly associated and mild physical shearing techniques will release them from the tissue. Mechanical techniques can cause significant cell damage. In many cases enzymatic digestion is an absolute necessity. Unfortunately most enzymes have severe deleterious effects on cells. These may be reversible or they may cause lysis. The lack of success in deriving cultures from adult tissue may, at least in part, be due to the extreme conditions necessary for dissociation of cells from the ageing tissue matrix. The criteria for choice of enzyme and dissociation conditions will need to be established by trial and error though previously published data may provide guidance. During the process of adaptation to tissue culture conditions, the cell undergoes a significant loss of many biochemical and morphological characteristics associated with the tissue of origin (Griffiths and Riley 1985). The extent of this de-differentiation will depend on the cell type and the suitability of the culture conditions. Nevertheless, primary cultures are considered more representative than some of the ubiquitous cell lines, in particular in the expression of tissuespecific properties. Tumour tissue is an extremely useful source of cells for primary cultures, especially if an immortalized cell line is required. Such cells tend to lack many differentiated characteristics and, even as primary cultures, display in vitro tumourgenic properties, such as loss of contact inhibition of growth (Griffiths and Riley 1985). It must be borne in mind that most primary cultures are made up of a heterogeneous cell population. However, by careful selection and isolation, it is possible to obtain a homogenous population. Even so, sub-culture will almost certainly lead to loss of more specialized cells and with them differentiated properties unless care is taken to select out the correct lineage. An essential feature of this developmental stage is to identify accurately the characteristics of the cell population of interest by all available techniques. Enzymatic techniques for tissue dissociation The procedure used to isolate cells from tissues must be designed to maximize the yield of functionally viable and dissociated cells remaining after digestion. Before preparing cell cultures the following list of parameters should be addressed so that a decision on the suitability of the prepared material can be made. 17 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Type of tissue, species of origin, age of the animal, dissociation medium used, enzyme(s) used, impurities in any crude enzyme preparation used, concentration(s) of enzyme(s) used, temperature and incubation times. Enzymes which may be used • Collagenase This enzyme, more accurately referred to as purified clostridiopeptidase A, is usually inefficient in dissociating tissue and the collagenase most commonly used for tissue dissociation is a crude preparation containing clostridiopeptidase A in addition to a number of other proteases, polysaccharidases and lipases. Four basic types of collagenase are now identified and available commercially: Type 1 contains average amounts of assayed activities (collagenase, caseinase, clostripain, and tryptic activities). It is generally recommended for obtaining fat cells, adrenal cells and liver cells. Type 2 contains greater clostripain activity. It is generally used for heart, bone, muscle, thyroid, cartilage and liver tissue. Type 3 is selected for low proteolytic activity. It is usually used for obtaining mammary cells. Type 4 is selected because of low tryptic activity. It is commonly used for obtaining the cells of the islets of Langerhans from pancreatic tissue and other such applications where receptor integrity is crucial. • Trypsin Trypsin is a pancreatic serine protease with specificity for peptide bonds involving the carboxyl group of the basic amino acids arginine and lysine. It is one of the most highly specific proteases known, although it also exhibits some esterase and amidase activity. Purified trypsin alone is usually ineffective for tissue dissociation since it shows little selectivity for extracellular proteins. Combinations of purified trypsin and other enzymes, such as elastase, have proven effective for dissociation of the cells of many tissues. ‘Trypsin’ is also the name commercial suppliers have given to pancreatin, a crude mixture of proteases, polysaccharidases, nucleases and lipases extracted from porcine pancreas. Crude ‘trypsins’ (National Formulary (NF) 1:250 or 1:300), are widely used for dissociating tissues, perhaps because the tryptic and contaminating proteolytic and polysaccharidase activities do bring about a preferential attack of the extracellular matrix. It appears, however, that crude trypsin and crude collagenase dissociate tissues by different mechanisms, and difficulties are often encountered when using NF 1:250 preparations - the most common being incomplete solubility, lot-to-lot variability, and cell toxicity. 18 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures In tissue culture laboratories, purified trypsin is used to release cells into suspension from monolayers growing on the interior surfaces of culture vessels. • Elastase Pancreatic elastase is a serine protease with a specificity for peptide bonds adjacent to neural amino acids. It also exhibits esterase and amidase activity. While elastase will hydrolyze a wide variety of protein substrates, it is unique among proteases in its ability to hydrolyze native elastin, a substrate not attacked by trypsin, chemotrypsin or pepsin. It is produced in the pancreas as an inactive zymogen, proelastase, and activated in the duodenum by trypsin. Elastase is also found in blood components and certain bacterial species. Because elastin is found in highest concentrations in the elastic fibres of connective tissues, elastase is frequently used to dissociate tissues which contain extensive intercellular fibre networks. For this purpose, it is usually used with other enzymes, such as collagenase, trypsin and chymotrypsin. Elastase is the enzyme of choice for the isolation of Type II cells from the lung. • Hyaluronidase Hyaluronidase is a polysaccharidase with as specificity for bonds between 2-acetoamido2deoxy-ß-D-glucose and D-glucoronate. It is often used for the dissociation of tissues, usually in combination with crude protease, such as collagenase. • Papain Papain is a sulfhydryl protease from the latex of the paw-paw or papaja tree, Carica papaya. Papain has wide specificity and it will degrade most protein substrates more extensively than pancreatic proteases. It also exhibits esterase activity. In some tissues, papain has proved less damaging and more effective than other proteases. • Deoxyribonuclease 1 Often, as a result of cell damage, nucleic acid leaks into the dissociation medium, increasing viscosity and causing handling problems. Deoxyribonuclease will digest the nucleic acids without damaging the intact cells. • Pronase This protease is a bacterial enzyme derived from Streptomyces frisens. In addition to gentle disaggregation of tissues, it is often used as an alternative to trypsin for sub-culturing cell lines. Because of its mild action, pronase may have to be used in conjunction with other enzymes, e.g. collagenase. • Dispase 19 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures This is a bacterial enzyme, obtained from Bacillus polymyxa. It is a neutral metalloenzyme requiring calcium for activity. It is useful for tissues of low hyaluronic acid content and is usually used in conjunction with other enzymes for complete digestion. • EDTA Ethylenediaminotetraacetic acid at a concentration of 0,02 % (w/v) in calcium- and magnesiumfree phosphate-buffered saline (PBS) can be used in conjunction with trypsin to enhance tissue disaggregation. Acting as a chelating agent, it dissociates intercellular links, such as tight junctions. For this reason it is not suitable for use with dispase. • Trypsin inhibitor (soybean) The trypsin inhibitor from soybean inactivates trypsin, but it exhibits no effects on the esterolytic, proteolytic or elastolytic activities of porcine elastase. Preparation and storage of enzymes Once diluted with medium or buffer, proteolytic enzymes may undergo autolysis. Dissolve them immediately before use. Special care must be taken with the deoxyribonuclease which is very prone to shear denaturation. They must be mixed gently. Reconstituted enzymes should not be stored at 2-8°C. If necessary, they can be aliquoted and frozen at -20°C. Avoid repeated freeze-thaw cycles. All enzymes, upon reconstitution, can be sterile filtered through a 0,22 μm membrane. Generally, all enzymes, except trypsin, can be directly dissolved in a balanced salt solution or buffer of choice. A stock solution of trypsin should be made initially by reconstituting the enzyme in 0,001M HCl. This solution can be diluted into the digestion balanced salt solution (BSS) or buffer immediately prior to use. Optimization of cell dissociation Although optimization of a cell isolation procedure for a particular cell type is dependent upon the adequate recovery of cells having various required characteristics, some guidelines can be established. There is a complex relationship between cell yield and viability. In general, there is an area of optimized recovery balanced between yield and viability; working near the middle of this range will reduce variability in the results of the cell isolation procedure. Trouble shooting • Low yield/low viability Over/under-dissociation, cellular damage. Change to less digestive enzyme and/or decrease working concentration (e.g. from trypsin to collagenase/from Type 2 collagenase to Type 1) 20 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures • Low yield/high viability Under-dissociation and/or incubation time monitor both yield and viability response. If yield remains poor, evaluate a more digestive enzyme and/or the addition of a secondary enzyme(s) • High yield/low viability Good dissociation, cellular damage. Enzyme overly digestive and/or at too high a working concentration. Reduce concentration and/or incubation time and monitor yield and viability response. Try diluting the proteolytic action by adding bovine serum albumin (BSA) (0,1-0,5% w/v) or soybean trypsin inhibitor (0,01-0,1% w/v) to the tissue suspension being dissociated. Try using less proteolytic enzyme although yield may be affected and should be monitored • High yield/high viability The place to be. Consider evaluating the effect of dissociation parameters to learn their limitations for future reference Sub-culturing of cell lines Routine sub-culturing - adherent When an attached cell line has either covered the surface available for growth, or depletes the nutrients in the surrounding medium, it must be sub-cultured into new vessels, e.g. flasks or dishes. Attached cells will exhibit strong to very light adherence, depending on cell type. For example, a confluent monolayer of the dog kidney cell line, MDCK, adheres to surfaces very strongly and requires both a protease, e.g. trypsin and a chelating agent e.g. EDTA to detach the cells. Conversely, the Chinese hamster cell line (CHO) can be loosened by gentle tapping of the culture vessel, or pipetting off the monolayer. However, the majority of attached cell lines will require at least the addition of a protease to dissociate the cells from the surface on which they are growing. To prevent either microbial infection or cross-contamination of cell lines, it is essential to maintain separate reagent bottles for each cell line, e.g. such as PBS, trypsin, medium. If only small quantities are required, aliquot the reagent into individual bottles. Mark each bottle in use with the cell line name and date of use. Additionally, each cell line must be handled separately, always working with those which have been characterized first. Allow a 10 - 15 min ‘clearance time’ between working with different cell lines, making sure that the flow cabinet has been thoroughly decontaminated with 70 % alcohol by wiping all internal surfaces, including the sides and glass screen, and that all reagents for the previous cell line are removed. If gloves are worn, these must also be changed. Hands must be washed after each subculture. 21 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Prewarm all the cell culture medium and PBS to the culture temperature. Allow the trypsin or trypsin-EDTA solution to reach room temperature. Remember that repeated warming will inactivate trypsin Microscopically examine the culture for its level of confluence of the cells, cellular morphological appearance and any signs of microbial contamination Decant the culture medium from the cells by either pouring or pipetting it off. If the medium is poured off (in case of flasks) invert the culture so that the medium runs down the side of the flask opposite to that to which the cells are adhered. Remember that decanting rather than pipetting off medium increases the risk of contamination. It is essential, whenever possible, to exclude antibiotics from the medium, in order to detect any infections at an early stage Wash the cells with a volume of Ca2+/Mg2+ - free PBS equal to at least half the volume of growth medium. Decant the PBS. Repeat, if the cells are of the type known to be strongly adherent Add trypsin or trypsin-EDTA solution to the cells, 1 - 2 ml per 25 cm 2 of flask surface, and gently spread over the entire surface by tilting the vessel. Leave inside the cabinet for 15 60 sec, at room temperature, and then decant or pipette off most of the solution Place the cultures in an incubator at their normal growing temperature, e.g. 24 °C for insect cell lines and 37 °C for mammalian cell lines. The cells should detach after 2 - 10 min as seen by gently tilting the vessel and observing if the cell layer moves. Gently tap the side of the vessel to increase detachment. Detached cells impart a milkiness to the suspension Microscopically examine the culture flask to determine if all the cells have detached. Reincubate if necessary Collect the cells by pipetting culture medium over the surface of the vessel, i.e. 2 - 5 ml per 25 cm2 of flask surface. Mix carefully to disperse the cells into a single-cell suspension. Measure the total suspension volume. Remember that trypsin activity is neutralized by serum proteins. It is important to ensure that the volume of serum in the culture medium of the new culture vessels is equal to, or exceeds, the volume of trypsin in the vessel subcultured. Cells will not attach if the trypsin is not neutralized At this point the cells can be counted . When culturing a new cell line it is advisable to make a viable cell count to estimate the maximum cell density achieved, i.e. cell/cm 2, and the expected viability Transfer the cell suspension into prepared culture vessels by inoculating the appropriate volume of the cell suspension. For routine subculture a split ratio is used (1:2 or 1:3 etc.). This is calculated as the ratio of surface areas; for example, a 75-cm2 has a split ratio of 1 into 3 (1:3), i.e. three 75 cm2 Roux flasks or only one 225 cm 2 flasks 22 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Place the inoculated vessels in an incubator at the correct temperature. If a CO 2 incubator is used leave culture flask caps loose Check the cultures after a few hours for cell attachment and pH. If the cultures are too acid (yellow), or alkaline (purple), the CO2 concentration must be immediately checked and adjusted. To prevent the loss of cultures due to a failure of the supply of CO 2 keep the flask saps tightened after cultures have equilibrated, i.e. 1 – 2 h. The duration between sub-cultures will depend on the incubation temperature and cell type. The majority of mammalian cell lines require sub-culturing every 3 - 7 days. If the duration is longer than 5 days, change the medium of the cultures every 3 - 4 days. Quantification of cells To measure performance, to achieve reproducibility, or to make comparative studies, a means of quantifying the cell population is needed. Classically, direct count of cell numbers using a microscopic counting chamber (haemocytometer), usually in conjunction with a vital dye (e.g. trypan blue) to distinguish viable and non-viable cells, is used. However, all vital stains are subjective and cannot give absolute values, and by counting cell numbers no differences in cell size/mass are taking into account. The method is simple, quick and cheap, and requires only a small fraction of the total cells from a cell suspension. Automation of cell counting is possible with electronic counters, especially for non-clumping single suspension cells. Other methods for total cell numbers include: • counting cell nuclei after dissolving the cytoplasm. This is particularly useful for large clumps of cells where cells are inaccessible (e.g. in matrices), or where cells are difficult to trypsinize off substrates (e.g. micro-carriers) • if cell mass, rather than number is the important factor then a cell constituent has to be measured • an indirect measurement can be used e.g. glucose or oxygen consumption rates. Other metabolites include lactic and pyruvic acid and carbon dioxide. There are reservations about these methods as these metabolic rates are not constant throughout the growth cycle of a specific cell and may also be influenced by changes in the culture, which is the subject of the investigation. These biochemical methods are best used over a time-course in culture so that successive readings will show a definite trend in the culture dynamics, e.g. stationary, growing or dying. A combination of one or two methods is the ideal. Haemocytometer cell counts In order to ensure that cell cultures have reached the optimum level of growth before routine subculture or freezing, it is helpful to obtain an accurate cell count and a measure of the percentage viability of the cell population. 23 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures The most common routine method for cell counting which is efficient and accurate is with the use of a haemocytometer. A thick, flat counting chamber coverslip rests on the counting chamber at a distance of 0,1 mm above the base of the slide. The base of the slide has rulings accurately engraved on it, comprising 1 mm squares, some of which are further divided into smaller squares. When a cell suspension is allowed to fill the chamber, the cells can be observed under a microscope and are counted in a chosen number of ruled squares. From these counts, the cell count per ml of suspension can be calculated. Hybridoma cells and others which grow in suspension may be counted directly. Cell lines which are attached will need to be removed from the tissue culture flask by trypsinization. Since accuracy of counting requires a minimum of approximately 105 cells/ml it may be necessary to re-suspend the cells in a smaller volume of medium. To ensure that a cell culture is growing exponentially, it is useful to know the percentage of dead cells and hence the stage of growth of the cells. This can be estimated by their appearance under the microscope, as live healthy cells are usually round, refractile and relatively small in comparison to dead cells, which may appear larger, crenated and nonrefractile when in suspension. The use of viability stains such as trypan blue ensures a more quantitative analysis of the condition of the culture. Trypan blue is a stain which will only enter across the membranes of dead/non-viable cells. When a cell suspension is diluted with a solution containing trypan blue, viable cells stay small, round and refractile. Non-viable cells become swollen, larger and dark blue. Both the total count of cells/ml and percentage of viable cells can be determined. The use of different cell cultures Monolayer cell culture techniques provide versatile and useful methods for isolating and propagating many viruses and for performing serological tests. The effects of viruses on the cells may manifest as cell degeneration or cytopathic effect (CPE), development of haemagglutinins or other antigens, haemadsorption phenomena, or interference with the effects of an ‘indicator virus’ which is added later. In general four different types of cell cultures can be used. These are primary cultures (directly derived from the disaggregated cells of monkey kidney, human amnion or other tissues), or secondary cultures (derived from the former by passage) in which the cells are still morphologically similar to those in the primary cultures, established cell lines (e.g. Hela) or also refer to as continuous cell lines, which are capable of indefinite serial growth in culture and semi-continuous lines. Established or continuous cell lines have special uses and free the laboratory from dependence on a source of primary tissue. Semi-continuous lines of human embryo cells, unlike established lines, retain their characteristic diploid chromosomal configuration; they are sensitive to a wide range of viruses but unfortunately they cannot be sub-cultured indefinitely and tend to lose their viability between the 30th and 50th passage. Preservation of early passages of these cells at temperatures of – 24 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures 70°C or lower provides an almost unlimited supply from one embryo. Low temperature storage is also useful for keeping stocks of continuous cell lines, which may be lost by microbial contamination, or may lose virus sensitivity with continuous cultivation, and for preservation of freshly trypsinized cells for primary cultures. A number of important conditions must be satisfied for successful cell culture: • The temperature should be 36-37°C (except for certain cells, e.g. epithelial cells, which grow better at a slightly lower temperature • The pH between 7,2 and 7,4. Fortunately, most cells survive and grow in a wider pH range (6,87,8) and at a temperature of 33°C or lower • The osmotic pressure of the medium is critical: it is mainly determined by dissolved crystalloids but may be severely affected by increases in glucose concentration. Inorganic ions essential for immediate survival of cells are sodium, potassium, calcium, magnesium, iron, carbonate, phosphate and possibly sulphate. Cell cultures require amino acids and vitamins (which the addition of serum provides) or they are given as a synthetic mixture. As a source of carbohydrate, glucose is usually added • Both oxygen and carbon dioxide are required, and are provided either as a mixture of CO 2 and air supplied to the culture vessel or by sealing the vessel tightly to retain CO 2 produced by cell metabolism • Aseptic techniques and the most scrupulous preparation of glassware, media and reagents are essential Because of the risks of contamination and infection, cell culture in the diagnostic laboratory is conducted in closed vessels consisting mainly of stoppered tubes or flat-sided bottles. Cultures are set up in an initial growth medium of which the simplest is Hanks Balanced Salt Solution (BSS) supplemented with lactalbumin hydrolysate and serum. Fastidious cells may require more complex chemically-defined media containing amino acids and vitamins such as (Eagle’s MEM or Parker’s Medium 199) which are also supplemented with serum for growth. Once the cells have formed a confluent monolayer, cultures are changed to a maintenance medium designed to maintain cultures for as long as possible in a healthy state without stimulating cell growth. This is achieved by reducing the serum concentration, or omitting it altogether. For growth of viruses in cell cultures, it may be necessary to use a particular inoculation medium whose composition depends more on the growth properties of the virus than of the cells. The use of organ cultures (in contrast to tissue cell cultures) in a diagnostic virus laboratory is at present of limited value. The object of this technique is to maintain the architecture and normal function of the tissue as occurs in vivo and is usually achieved by culturing small fragments of organs in chemically defined media. Organ cultures of ciliated nasal or tracheal epithelium from human embryos have led to the recognition of new human respiratory viruses (e.g. coronaviruses) which are not detectable by conventional methods. More recently these techniques have been adapted to the maintenance of human embryonic intestine for the study of diarrhoea illnesses and of human embryonic conjunctivae for the isolation of some strains of enteroviruses. In Veterinary Clinical Virology, the tracheal rings of chickens are generally used for the identification of coronaviruses. 25 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Table 2: The use of different cell lines for viral isolation Foot- and- mouth disease virus Primary porcine kidney, BHK, Vero Rinderpest virus Bovine kidney, Vero Infectious bovine rhinotracheitis Vero, MDBK Bovine virus diarrhoea virus Primary bovine foetal kidney Bovine ephemeral fever virus BHK Bluetongue virus, African horsesickness virus, and other BHK, Vero, insect cell lines e.g. C6/36 orbiviruses Equine rhinovirus 1 Vero Equine rhinovirus 2 RK-13 Canine distemper virus Vero Canine hepatitis virus Vero, MDCK Newcastle disease virus Vero Rabies virus BHK, Vero Lumpy skin disease virus Primary bovine dermis, Primary equine lung, MDBK Rift Valley fever virus BHK, Vero, insect cells e.g. C6/36 Wesselsbron disease virus Vero, insect cells e.g. C6/36 Canine parvovirus Feline kidney African swine fever virus Leukocytes, porcine kidney Equine herpesvirus Primary equine lung Feline enteric coronavirus CRFK, NLFK Feline herpesvirus CRFK, NLFK Feline calicivirus CRFK, NLFK Equine arthritis virus RK-13, Vero C6/36 Aedes albopictus clone C6/36 CRFK Crandell feline kidney 26 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures NLFK NL- feline kidney VERO African green monkey cells BHK Baby hamster kidney cells RK-13 Rabbit kidney BHK Baby hamster kidney cells MDBK Madin-Darby bovine kidney MDCK Madin-Darby canine kidney Contamination of cell cultures Bacterial and fungal contamination of cell cultures occurs when they are inoculated with clinical material naturally contaminated with micro-organisms. The incorporation of high concentrations of antibiotics into transport medium and other reagents used for clinical specimens, and their routine use in all cell cultures, reduce it to a very low level. Cultures contaminated with bacteria and yeasts rapidly become turbid and the pH generally falls. Under the low power of the microscope, yeasts are distinguished from bacteria by their larger size, budding forms also commonly being present. Mould contamination is characterized by a rapidly proliferating macroscopic mass whose form depends upon the particular contaminant. Mycoplasma is a generic term given to organisms of the order Mycoplasmatales which can infect cell cultures. Those which belong to the families Mycoplasmataceae Acholeplasmataceae (Acholeplasma) are of particular interest. (Mycoplasma) and The first observation of mycoplasma infection of cell cultures was by Robinson et al., (1956). The incidence of such infection has since been found to vary from laboratory to laboratory. Mycoplasmas do not necessarily manifest themselves in the manner of most bacterial or fungal contaminants, e.g. pH change or culture turbidity. It is important therefore to adopt an active routine detection procedure. Mycoplasmas have been shown to elicit various effects, including: • Induction of chromosome aberrations (Aula & Nichols 1967) • • Induction of morphological alterations, including cytopathology (Butler & Leach 1964) Interference in the rate of growth of cells (McGarrity et al., 1980) • Influence nucleic acid (Levine et al., 1968) and amino acid (Stanbridge et al., 1971) metabolism • Induce membrane alteration (Wise et al., 1978) and even cell transformation (MacPherson & Russel 1966) A range of assay techniques are available for the detection of mycoplasma contamination. These include staining, culture, DNA probes and co-cultivation. To remove the risk of false negatives two methods at least should be employed. The enrichment broth and agar culture and Hoechst 33258 DNA staining are recommended techniques. The fluorochrome dye Hoechst 33258 binds specifically to DNA. Cultures infected with mycoplasmas are seen under fluorescence microscopy as fluorescing nuclei with extranuclear mycoplasmal DNA, whereas uninfected cell cultures contain fluorescing nuclei against a negative background. 27 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Mycoplasmas may appear as filamentous forms, some of which may branch, indicating a culture in logarithmic growth, or as cocci, which is typical of an aged mycoplasma culture. Contaminating fungi or bacteria will also stain using this technique but will appear much brighter and larger than mycoplasmas. The main advantage of this dye technique is that it is speedy and that non-cultivable mycoplasma strains, which have been detected in cell cultures, can be observed. Cryopreservation Polge et al. (1949) made the observation that glycerol enhanced the survival of fowl semen at –79°C. The technique was then used for other cell types. Lovelock and Bishop (1959) discovered the cryoprotective properties of DMSO. Mazur (1970) showed that cells cooled slowly in the presence of a cryoprotectant shrink, and do not contain intracellular ice. DMSO increases the membrane permeability and the reversal of intracellular ice formation. The prevention of intracellular damage on thawing is essential to successful cryopreservation (Mazur 1977). A major achievement permitting the development of animal cell technology has been the determination of the parameters for routine cell cryopreservation. The importance of a stable, reliable, secure supply of material held at temperatures below –130°C cannot be overstated. At its most simple, the technology is based on slow freezing and fast thawing, together with high protein concentration and the presence of an agent which increases membrane permeability. The other, perhaps obvious, ingredient is ‘healthy’ cells. The first consideration is whether glass or plastic ampoules should be used; both have their advantages and disadvantages. A correctly sealed glass ampoule will not permit entry of liquid nitrogen which might be the case with a screw-capped plastic ampoule. This is important in two respects: the presence of liquid nitrogen during rapid warming could risk the danger of explosion due to the rapid expansion of gas; liquefied gas is not sterile and could carry contaminating objects into the ampoule. However, glass ampoules are comparatively difficult to seal, and have to be thoroughly tested before freezing. An additional problem with glass is labelling; ceramic ink is needed which requires specialized equipment and a certain degree of expertise. For most users, plastic ampoules are more convenient as they are pre-sterilized and will label with marker pens. In addition, there is a commercially available heat-shrinking sheath which can be placed over the ampoules to minimize the risk of entry of liquid. The means of freezing at a controlled rate is another major consideration. A controlled-rate freezing apparatus is considered by some as an expensive luxury. Nevertheless, successful freezing is virtually guaranteed when alternative methods are used. Some pre-validation of the methodology to be employed is strongly recommended. Long term storage Long-term storage of cell stocks requires good record keeping and maintenance of an inventory with each removal logged to ensure adequate stock levels. 28 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures A wide range of liquid nitrogen refrigerators is available. Whatever the choice, they must be alarmed to prevent accidental drying out. In addition, the ampoules must be kept in more than one location. In the routine handling of cell stocks, it is essential to avoid wide fluctuations in storage temperature. Frequent removal of the inventory system from the refrigerator with the associated variation in storage temperature will reduce viability. It is recommended that stocks are periodically checked for maintenance of viability - every 5 years. Mechanical freezing Cryopreservation using –80°C or –130°C in a mechanical freezer is probably the least reliable of methods. However, low-temperature freezers are widely used to cryopreserve cell lines. To achieve slow cooling, ampoules must be heavily insulated. A block of polystyrene containing individual holes sufficiently large to take ampoules should be prepared. The polystyrene must be 1 - 2 cm deep all around the ampoule, with no air spaces. The insulation required is placed in the block, which is then placed near the middle of the freezer and left overnight (16 –24 h) before being transferred to a liquid nitrogen storage vessel. Before using this method on a regular basis, a series of tests should be made to monitor the cell viability after freezing. If it varies significantly from the viability of the cells prior to freezing, i.e. a drop of more than 15 – 20%, the insulation will have to be modified. This method is not recommended for preparing master or reference stocks for long term storage. Two-stage freezing Ampoules are kept at a holding temperature of –20° to –40°C for up to 24 – 48 h and then transferred directly to –196°C. Similar results can be achieved for a small number of ampoules by using a small device which holds them in liquid nitrogen vapour in the neck of a Dewar flask. After a holding time of 10-20 min the ampoules are plunged into liquid nitrogen and then transferred to their final storage location. Preliminary experimental work is required to determine the optimum conditions. In all cases, the cells should be examined for viability following cryopreservation. For certain specialized cell types, it may be considered necessary to include particular essential growth factors to the freeze medium in order to maintain surface receptor stability during cryopreservation. For example, hybridomas often cause problems on revival. It is essential to use freshly prepared freezing mixture every time. DMSO should be obtained from a supplier who is able to offer the most recently prepared stocks available. Once received, it should be filter sterilized (0, 2 μm) through a filter specifically designed for DMSO and stored in a glass container with an air-tight stopper or lid at –20°C. This will ensure that no problems 29 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures develop due to oxidation of the DMSO. In those cases where DMSO causes differentiation, glycerol should be used instead. Thawing • Achieve rapid thawing by transferring ampoules directly to a water bath containing water at 37°C. If an ampoule contains potentially hazardous material, it is advisable to add 1 - 2% (w/v) chloramine-T to the water in the water bath. • Take care not to submerge the cap of the plastic ampoule in order to prevent contaminated water from entering the ampoule. A simple method is to use a plastic rack designed to hold tubes of the same diameter as that of the ampoules, and to place it in the correct depth of water. Alternatively, a piece of foam polystyrene foam containing holes into which the ampoules are fitted; this will float on the surface of the water. • Once thawed, transfer the ampoules to the sterile work area. Submerge glass ampoules in 70% ethanol for a brief period and thereafter allow them to dry. A pre-scored ampoule can be snapped open using a paper tissue soaked in 70% ethanol. Unscored types must first be scored with a diamond before soaking in 70% ethanol, after which they are opened. Plastic ampoules are opened whilst gripped with a tissue soaked in 70% ethanol. • Using a pipette, transfer the ampoule contents into either a flask or a centrifuge tube containing prewarmed growth medium. A slow transfer is recommended. If it essential to remove the cryoprotectant at this stage, centrifugation should be at the lowest speed necessary to form a cell pellet. For cultures started directly from an ampoule, the first medium change should be at 24 h after transfer unless recommended otherwise. Start-up cell density is of critical importance. The cells must be encouraged to become conditioned to the medium as rapidly as possible and prevent a protracted lag phase. For adherent cells, an initial density of 2-5 x 104 cells /ml is normally appropriate. • Examine the cells daily using an inverted microscope and subculture them as soon as confluency or maximum cell density is reached. This is frequently indicated by a medium colour change to orange or orange-red, i.e. acid pH. Safety considerations During the handling of frozen ampoules, a full-face mask and gloves must be worn. Ampoules containing pathogens should be thawed on an outer sealed container. In order to prevent explosion of the ampoules on their removal from the liquid phase, it is recommended that transfer to the gaseous phase is carried out 24 h prior to thawing. To reduce the risk of injury from exploding ampoules during thawing, it is advisable to place them in a perforated container before they are placed in a water bath. Demonstration / confirmation of the presence of viruses in infected cell cultures Introduction 30 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures When evidence of viral infection is observed in inoculated cell cultures, either by the development of CPE or by a positive haemadsorption test, the affected cultures should be subcultured in order to demonstrate propagation of the effects. If the CPE observed is minimal, one may increase the likelihood of a successful passage if the CPE is allowed to progress. Since some viruses are cell associated one should ensure that cells are transferred as well as fluid when making a passage. Once evidence of the presence of a virus is obtained, an identification procedure can be selected based on the assessment of the most likely viruses to display the effects noted and which appear consistent with the nature of the specimen and the patient’s illness, i.e. one would not look for influenza virus as an isolate from a stool specimen. Although numerous methods of identification have been developed, usually only a few of them are routinely used by any particular laboratory. With the exception of the biophysical characterization, which is used to obtain the taxonomic assignment of a virus that proves difficult to identify, the methods used are mostly immunological. The most commonly used techniques are immunofluorescence and neutralization tests, and ‘reversed’ serology tests, such as the haemagglutination inhibition and complement fixation (the latter in general used anymore). The immunofluorescence test (direct or indirect) is often the most convenient way to determine the identity of many common pathogenic viruses. These techniques are most useful whenever only one or one of a small number of agents is considered most likely to be involved. In the absence of reagents or facilities for performing immunofluorescent identification, perhaps the next most convenient means of viral identification is the use of ‘reverse’ serology. This is where the virus-containing culture is used as an unidentified serologic antigen, which is to be tested for reactivity with a number of specific reference sera. Haemagglutination inhibition is well suited for this type of identification in that the reactivity of the antigen is known before the test is carried out; complement-fixation is more difficult to use, both technically and in that the reactivity of the unknown antigen is not assured before the test is run. Serotyping of viruses can also be accomplished by means of the neutralization test. Handling of specimens for the isolation and identification of viruses Preparation of clinical specimens for viral isolation Most clinical material requires processing before being tested in order to remove extraneous, non-virus matter. In general, it is necessary to prepare a reasonably concentrated, homogeneous suspension of the specimen free from particulate matter which might block hypodermic needles and pipettes or obscure specific effects in tissue cultures and other test systems. Certain types of specimen e.g. swabs, nasal washings, lesion scrapings, and cerebrospinal fluid usually contain little if any solid debris, in which case they may be tested without prior treatment. Nasal washings Centrifuge the nasal washing fluid at 2000 rpm for 15 min at 4°C to remove debris. This procedure may be omitted if no debris is present. Carefully pipette off the supernatant fluid. 31 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Freeze and store the unused supernatant fluid and remainder of the specimen. Depending on the time period of storage material can be stored either at 4°C or at –20°C. Cerebrospinal fluid No processing is generally required. If cellular material is obviously present, transfer the fluid to a centrifuge tube and proceed as for nasal washings. Antibiotics are usually added. The type and concentration of the antibiotics used depends on the laboratory, but in general a broad spectrum antibiotic is used. Urine No processing is generally required. If cellular material is obviously present, transfer the fluid to a centrifuge tube and proceed as for nasal washings. Antibiotics are usually added. Saliva No processing is generally required. Antibiotics are usually added. Biopsy or necropsy tissue and organ specimens for viral isolation Weigh approximately 1 g of the specimen and place it in a Ten-Broeck tissue grinder of suitable size or a pestle and mortar with sterile sand. Add sufficient phosphate-buffered saline containing extra antibiotics to make a 10% w/v suspension, and grind by hand until a uniform homogenate is obtained. The time required for complete homogenization depends on the nature of the tissue. Relatively non-fibrous tissues, such as brain may be adequately suspended within 1 – 2 min, whereas a much longer time is required for tissue, such as muscle. In the latter case, the grinder should be embedded in crushed ice to avoid overheating during the grinding process. Suspensions of tissues of even greater resistance, such as keratinized skin, are best made by grinding the tissue in a mortar containing washed sand and phosphate– buffered saline. When homogenized, transfer the suspension to a centrifuge tube and processed as for nasal washings. Faeces Faeces samples are not normally used for viral isolation in cell culture. Electron microscopy is a rapid and sensitive method to identify many viruses. If cell cultures are used: • One method is to weigh about 1 g of faeces into a screw-capped bottle containing about 5 g coarse beads approximately 5 mm in diameter. Add sufficient phosphate-buffered saline containing a high concentration of antibiotics to make a 10% w/v suspension. Shake vigorously by hand for 30 sec or until the faeces are uniformly dispersed. Centrifuge the resulting suspension at 4000g for 20 min at 4°C. High speed centrifugation is desirable since it removes the majority of bacteria and certain toxic substances from the stool suspension. Carefully remove and save only the upper two-thirds only of the supernatant fluid, discarding the remainder. Freeze and store at approximately –20°C. 32 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures • Faecal samples can also be extracted with chloroform before being used for the isolation of viruses in cell cultures. This method entails: A suspension of the faeces is made using phosphate buffered saline (PBS). Chloroform is then added, and the suspension shaken and centrifuged. The supernatant is used to infect cell cultures. Swabs Procedures used for the preparation of nasal, throat, rectal and vesicle swabs are identical. Macerate the swab well in the transport medium in which it was submitted, to disperse any virus particles. Transfer the resulting suspension to a centrifuge tube, and proceed as for nasal washings. Tissue scrapings of lesions Add coarse glass beads to the transport medium in which the scrapings were transmitted and submitted. Shake vigorously by hand for about 5 min at room temperature in order to disrupt any intact cells. Transfer the resulting suspension to a centrifuge tube and proceed as for nasal washings. Blood Blood in heparin is generally used for viral isolation. The blood is added to the cells, left for an hour and then the cells are washed with medium before adding fresh medium to the cells. In some cases the blood can be toxic to the cells, but in general the cells will flourish. Blood destined for serological investigation is best collected in containers, which can be centrifuged subsequently. Inoculation of cell culture Care must be taken in the preparation of the material suspected to contain the antigen or antigens. The isolation cabinet should be cleaned before using a disinfectant. Do not prepare tissue specimens from more than one animal or more than one antigen at the same time in the cabinet. Viruses are generally isolated from diagnostic samples using cell monolayers in tubes or 25 cm2 flask cultures. Before use the medium in the flask is changed from a growth medium to an equivalent volume of the maintenance medium of choice. The serum content of the maintenance medium is lower than that of the growth medium. This is to prevent the overgrowth of the cultured cells and their consequent rapid degeneration. If normal bovine serum has been used in the growth medium all traces of it must be removed to prevent the presence of antibodies which may interfere with the isolation of certain viruses. If a serum-free maintenance medium is used, the monolayers are first washed free from residual growth medium. This is done by aspirating the fluid and rinsing twice with maintenance medium before finally adding the same volume of maintenance medium as there originally was of growth medium to the flask. 33 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures The cultures are screened before inoculation. Medium changing carried out the day before inoculation will ensure that the pH is not too high and will assist in the screening process. Screening should be carried out microscopically. A volume of 0,2 ml of the prepared material from the clinical specimens are inoculated into each of preferably four tubes/flasks which are incubated immediately. Four tubes/flasks in each batch are kept as uninfected negative controls. In order to reduce the risk of cross-contamination between specimens, only one specimen is inoculated at a time, each specimen container and the inoculated tubes being properly stoppered and labelled before proceeding to the next. Moreover, since inoculation inevitably involves contamination of the tube/flask lip during entry and exit of the inoculating pipette, the tube/flask must be adequately flamed before closing. This requires care, since too rapid heating may result in spluttering of infective fluid. However, it is important that no residual virus remains on the lip. Maintenance of inoculated cultures Once specimens have been inoculated into cell cultures, all further manipulations which may provide opportunities for cross-contamination of the cultures to occur should be avoided. Primarily, this comprises the opening of the tubes for the purpose of changing the medium, or adding buffers to adjust the pH. In addition blind passage should be avoided as far as possible, to reduce the total number of cell cultures required and thus the general workload involved. One approach to these problems is to increase the buffering capacity of the maintenance medium in which the cultures are kept by the addition of synthetic buffers to the medium: the HEPES buffer is widely used for this purpose, but the MOPS buffer is less expensive and works well. A well-buffered maintenance medium containing galactose in the place of glucose reduces the formation of acids by cellular fermentation is an alternative, but very expensive, medium. Inoculated cell cultures are held, with daily to three times a week observations, for two weeks, or as long as a given lot of cell cultures do not undergo spontaneous degeneration – observed in the non-inoculated control cultures. Specimen toxicity, in the form of nonspecific CPE, usually develops within a few hours after inoculation of cell cultures. If non-specific CPE appears in inoculated cell cultures, especially if it occurs shortly after the inoculation, the affected cultures should be used to inoculate fresh cultures (passed), to dilute out potential toxic material in the inoculum. Cytopathic effect An inoculated culture should be examined microscopically every day so that the onset of changes may be observed and their progress followed. In this way, any virus-specific effect (cytopathic effect or CPE) may be differentiated with certainly from any non-specific phenomena. In practice, it is often not possible to undertake daily examinations, especially when large numbers of tubes are involved. With some experience of the rates at which changes induced by different viruses advance but also of the agents likely to be encountered in given clinical materials, the times at which tubes are read may be profitably adjusted. 34 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures It is important, however, that a reading is always made on the first day after inoculation when any non-specific cell changes due to toxicity of the clinical specimen will be disclosed. Toxic changes are variable. Mild toxicity is frequently manifest as a diffusely spread granularity of the cell cytoplasm. In toxicity of a more severe degree, the cells may become pyknotic, or bizarre forms may be apparent. When stool specimens or rectal swabs are inoculated, traces of residual trypsin from the gut may actually digest the cell monolayer from the glass. Non-specific toxic changes of the foregoing kind are readily distinguished from almost all kinds of virusinduced changes which, in any case, are unlikely to appear during the first 24 hours following inoculation. The importance of this first-day reading is that non-specific changes may progress rapidly to total destruction of the culture, which at a later stage is unlikely to be distinguishable from a culture destroyed by specific virus action. Non-specific changes observed on the day after inoculation may often be reversed, or their progress halted, by removing the medium and replacing it with an equal volume of fresh maintenance medium. Since fluids removed 24 h after inoculation may contain large amounts of virus, the changing procedure should be done with the utmost care in order to restrict cross-contamination. It is convenient to adopt a numerical system of scoring when reading tubes for cytopathic changes. The extent of involvement is usually scored on a scale from 0 to 4. At one end of the scale, 0 represents a normal culture without CPE, while at the other extreme; a completely degenerated culture is scored 4+. Varying degrees of involvement are given in between values. Thus, a culture with one or a few foci of infection is scored 1+, while a tube in which approximately 10% of the monolayer is affected is rated 2+. When 50 – 75% of the monolayer is involved, a 3+ rating is given. It is obvious that such a system entails an element of subjective interpretation. However, a single person can achieve a high degree of reproducibility, so that comparisons within and between experiments are valid. The appearance of CPE in certain cell cultures is characteristic for some viruses. Respiratory syncytial and distemper virus induce non-haemadsorbing multinucleated giant cell formation in many cell cultures. Adenovirus infection results in the aggregation of the cells into ‘clusters’. Herpes simplex virus gives rise to ballooning of human embryo cells, and the shrinking and rounding of other cell types. Enteroviruses and rhinoviruses cause rounding of cells and are difficult to distinguish from each other by their CPE. Examination of cultures showing complete CPE by electron microscopy may be helpful in ‘grouping’ the agent, thus possibly minimizing subsequent specific identification procedures. Cultures not showing CPE The majority of cultures inoculated with clinical material almost never develop CPE. This may be because of: • No virus was present in the sample • Most tissue culture systems are far from the ideal for growing non-adapted viruses, and therefore clinical material may not elicit a CPE although incubated for a time adequate for the virus to develop on theoretical grounds – the same virus may produce CPE if given more time. Cultures failing to give CPE can be sub-cultured into further tubes. Cells as well 35 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures as medium are transferred. Prior to sub-culturing the cells are detached from the tube wall by vigorous pipetting of the medium, and 0,2 ml of the suspension is then inoculated into another tube of the same kind and incubated under the same conditions as before. Tubes failing to produce any CPE by the end of the second period are recorded as negative. This is referred to as the blind passaging of cells. • The susceptibility of the type of cells used. Some cell cultures may not be the ideal cell type for a specific virus. This can be very common in Veterinary Clinical Virology because of the large number of different animal species that are dealt with. The clinical signs of the animal as well as the expected virus in the sample must be considered. • Cell cultures, derived from insect cells (mosquitoes, etc.) will, because of their vector capabilities for certain viruses, not produce CPE. Such cell cultures then become persistently infected with the virus and, in a clinical diagnostic situation, one needs to ‘blind passage’ these cultures to a mammalian cell culture in which the virus (if present) in most cases will produce CPE. Inclusion bodies Viral replication proteins and assembled virions often accumulate in specific regions of the nucleus (e.g. inclusion bodies or replication compartments in cells infected with herpesviruses or adenoviruses) or cytoplasm (e.g. the Negri body in rabies-infected cells). The assembly of these new structures in the infected cell often displaces host-cell components from specific regions of the cell and leads to one form of CPE. The inclusion bodies, or areas of altered staining in infected cells, are useful in diagnostic virology because they are found at locations in the cytoplasm or nucleus (or both) which are characteristic of specific groups of viruses. Also, they show characteristic staining properties in that they are basophilic or acidophilic. To clearly see these inclusion bodies, cells are grown on coverslips, fixed and stained. Hematoxylin and eosin is the stain of choice. These structures are used in diagnostic virology and are illustrated by the following examples: Parvovirus forms typical intranuclear inclusions, which can be used as a diagnostic tool. Measles virus The most striking and consistent feature of measles virus infection in vivo as in vitro is the formation of multinucleated giant cells, which results from the fusion of infected cells with their infected and uninfected neighbour cells. In tissue culture, these giant cells contain eosinophilic cytoplasmic inclusion bodies. Reoviruses Cells infected with reovirus develop characteristic cytoplasmic inclusions referred to as ‘viral factories’ or ‘inclusion bodies’. These inclusions initially appear as phase-dense granular material scattered in the cell cytoplasm, which eventually coalesce and move toward the nucleus. Dense perinuclear inclusions subsequently appear and increase in size as infection progresses. Inclusion body formation is delayed when infected cells are maintained at low temperature. Different cell lines vary in temporal sequence of inclusion body formation following 36 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures infection. Viral inclusion bodies have been shown to contain dsRNA, virus-specific polypeptides and both complete and incomplete viral particles. Orbiviruses Virus synthesis and maturation occurs in the cytoplasm of infected cells, where inclusions and crystalline arrays of virions are sometimes found. These virus inclusion bodies apparently represent centres of viral replication or assembly. Accumulations of tubular structures or virusspecific tubules are also seen in infected cells. Fixation and staining of coverslips Cells grown on coverslips are used to identify viruses especially those which induce the formation of inclusion bodies and syncytia. Coverslips are first fixed in a fixative, such as ethanol or Bouins fixative, and then stained with the desired stain. They are then mounted onto microscopic slides for observation. Syncytia The formation of multinucleated giant cells results from the fusion of infected cells with their infected and uninfected neighbour cells. Measles virus, distemper virus and other viruses of the Paramyxoviridae family have this unique characteristic, which can be used for their viral identification. Plaque test Cell monolayers are infected with certain viruses which are allowed time to enable them to settle on and attach to the cells. The latter are then overlaid with a nutrient agar medium to limit the spread of the viruses. As a result, localized, often multiple, areas of cellular destruction and lysis (CPE) called plaques are formed. These may be detected if the monolayers are stained with dyes, such as neutral red or trypan blue, that are used to distinguish living from dead cells. This technique can also be used for the quantification of viruses in a solution or specimen, in which case the titre of the virus sample is then expressed as plaque forming units per volume. Plaque separation - if a mixture of viruses is suspected the same technique can be used to obtain pure cultures of viruses. It is also known as the plaque purification method. Haemadsorption The detection of haemagglutinins either by haemadsorption or haemagglutination is widely used to detect infection by membrane-bound viruses, such as orthomyxoviruses and paramyxoviruses, which obtain their outer envelope by budding through the cell membrane and may cause little or no CPE. Prior to budding, viral coded proteins (haemagglutinins) are incorporated into the cell membrane. Even with strains that produce CPE, haemagglutinins are usually detectable at an earlier stage. Cell cultures which are sensitive to myxoviruses should 37 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures be tested for their presence by haemadsorption 5 – 7 days after inoculation. Un-inoculated control cultures should be tested together along with the inoculated cultures to detect haemadsorbing viral contaminants which are frequently found in primary monkey kidney cultures. The haemadsorption test is a particularly convenient screening test, as one need only add a few drops of dilute erythrocyte suspension to the tubes containing the control cells and to those inoculated with the specimens being tested. The cultures are then refrigerated briefly to allow adsorption to occur and to inhibit the relapse of the adsorbed cells by viral neuraminidases. The cultures are inverted and inspected to determine if erythrocytes are adhering to the infected cells. The culture medium can be removed and monolayers washed in order to facilitate the inspection, but this is not always necessary. If the haemadsorption test gives an ambivalent result it is recommended that the more sensitive haemagglutination test be performed. Haemagglutination Haemagglutination (HA is a property of some viruses. For human viruses, the human ‘O’ group red blood cells (RBC) are normally used for influenza and parainfluenza viruses, and certain enteroviruses and adenoviruses. Chicken RBCs are used for Newcastle disease virus and porcine RBC for parvovirus of dogs. Many viruses have optimal temperature and pH requirements for HA, and these variables along with the need to absorb sera for naturally occurring agglutinins to some species of RBC, make HA tests particularly difficult to reproduce with certain specificity. Binding is accomplished by an interaction of viral proteins (haemagglutinins) located in the outer coat of the virion or virion envelope with receptor sites on the RBC. Agglutination is a result of the bridging effect of one virion binding to two RBCs simultaneously and these in turn being bound to other RBCs by additional virions. The result is a lattice-like aggregate of RBCs. The ability of viruses to agglutinate RBCs is influenced by pH and temperature. Agglutination of RBCs is useful for the concentration and purification of some viruses, and as a rapid presumptive test for the presence of these viruses in fluids from infected cell cultures and chicken embryos. It is especially useful for assaying viral activity of cell cultures infected with haemagglutinating viruses that produce little or no discernible CPE. Clinical specimens such as faeces can also be directly examined for haemagglutinating (HA) activity. For example, a presumptive diagnosis of canine parvovirus can be made by demonstrating HA activity to porcine RBCs in faecal samples. 38 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Figure 1: Schematic presentation of the haemagglutination test Serology Serum viral neutralization test Serum viral neutralization test (SNT) is the most widely used method of detecting and measuring antibodies to viruses of veterinary importance. This test is generally considered to be the most reliable of all serologic tests, being less prone to variation and less subjective in its interpretation. The principle of the test is based on the fact that the demonstrable activity of the virus - whether it is CPE in cell cultures, clinical signs, lesions or death in embryonated chicken eggs and animals - can be inhibited by specific antibody to that virus. SNTs are almost always performing using cell cultures. Stock viruses for use in the tests are previously grown, aliquoted, and stored at ultra-low temperature. These viruses are titrated several times to determine the amount of virus present. Performance of the test entails the dilution of the test serum in microtitre plates, followed by the addition of an equal volume of virus suspension diluted to contain approximately 100-300 infective doses. Following incubation of 1 to 2 h at 37°C, indicator cell cultures at a certain concentration are added. Plates are sealed, incubated at 37°C, and observed daily for development of viral CPE. The presence of specific antibody in the test serum inhibits the production of CPE. The SNT is also used to identify unknown viral isolates in essentially the same manner as described above. The only difference is that different known antibodies must be used and identification of the unknown virus is accomplished by the one which inhibits the development of CPE. Serotyping To determine the serotype of a virus the neutralization tests is normally performed using specific antibodies. This test is carried out using a standard challenge dose of virus, which is determined by preliminary titration of the isolate. Unfortunately, the neutralization tests are time-consuming and expensive due to the need to use large numbers of cultures for the titration 39 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures and neutralization steps, and the need to await virus growth in controls and non-neutralizing serum reactions. Also the subject is complicated by the existence of heterologous neutralization reactions, poorly neutralizing strains (which may be due to aggregated virus) and prime strains, which react in one-way crosses with standard prototype strains used to produce the reference sera for the neutralizations. Haemagglutination inhibition test The haemagglutination inhibition test (HAI) test is used to measure specific antibody, which often corresponds with neutralizing antibody, and to identify virus isolated using specific animal or bird antisera. Test sera often contain non-specific inhibitors of agglutination and may result in false positive antibody tests. These can be removed by the adsorbing of sera with RBC or by the treatment of sera with kaolin and the ‘receptor destroying enzyme’ prior to testing. The HAI test is similar in principle to the SN test except that the viral activity being inhibited is haemagglutination. HI tests are quite sensitive and highly specific, and are particularly useful for measuring antibody to those haemagglutinating viruses that either grow poorly in cell culture or produce little or no discernible CPE. Examples of such viruses are Type A influenza viruses of most animal species, Newcastle disease virus of birds, and porcine parvovirus. HI tests are usually performed in microtitre plates. Dilutions of test sera (25 µl) are made, followed by the addition of an equal volume of virus suspension diluted to contain approximately 4 to 8 HA units. The appropriate RBC suspension is then added (50 µl) and the plates are gently mixed and allowed to incubate for 1 to 2 h at 4°C (for most viruses). If the specific antibody is present in the test serum, agglutination of RBC will be inhibited and the RBCs will settle out in a welldefined “button”. Agglutinated cells, in contrast, will settle out in a thin layer over the entire bottom of the test well, or in a rough, irregularly fringed button. Figure 2: Schematic presentation of the haemagglutination inhibition test 40 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Figure 3: Schematic representation of the haemagglutination inhibition test Electron microscopy A feature of many viral groups, which can be used with advantage for diagnostic purposes, is that they are morphologically distinct. When viewed in electron microscope (EM) herpes, pox, adeno, rota, influenza and wart viruses are readily distinguishable, even to the untrained eye. Widespread use of the EM in diagnostic virology is limited principally by the large number of particles (>106/ml) required before even one of them can be seen on the microscope screen. The diagnostic use of the EM for direct examination of clinical specimens is thus restricted to viruses which are concentrated naturally in the body, e.g. herpes simplex, small pox or chickenpox virus in vesicles, wart or orf virus in skin lesions, rotavirus, astrovirus and others in faeces. Throat swabs and respiratory secretions contain little virus and although viruses have been identified directly by electron microscopy in such specimens, the EM can best be used indirectly to identify virus after it has multiplied to a sufficient level in cell culture. Generally, any cell culture exhibiting complete CPE will contain enough virus for it to be visible in the EM, and examination of such cultures is worthwhile as time and reagents can be saved by the early identification of the virus group to which it belongs. The information provided by the EM is purely morphological, i.e. size, shape and surface detail. Specificity, therefore, is limited to the virus group: although adenoviruses can be distinguished from herpes viruses, adenovirus type 2 is morphologically indistinguishable from adenovirus type 5, and herpes simplex type 1 from herpes simplex type 2. Some differentiation within groups can be achieved by observing whether the virus will react with type-specific antibody as shown by antibody molecules visibly attached to a virus or by clumps or virus particles aggregated by antibody molecules. However, this combination of serology and electron microscopy – immune electron microscopy - is mainly used for identifying viruses of poor morphological differentiation and low titre. It can only be recommended for identifying members within a virus group if high titred, type specific sera are available. 41 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures VIRAL QUANTIFICATION Infectivity assays for viruses Two general types of assays are based on the ability of the virus to infect cells. The first depends on quantification of individual, localized infection in a layer of cells. The plaque assay is an example of this. The second method depends on the detection of virus infection in cell cultures or animals, inoculated with serial dilutions of the virus, is better known as the end-point dilution method. Dose response curve and significance of ID50/TCID50 Figure 4: Dose response curve Examine this graph • of the 50% area of response a very small alteration in the host is reflected by an exaggerated difference in the percentage of the host affected • at high extremes of the curve, a much greater variation in the dose is required to affect the • number of hosts thus the point of maximum sensitivity of the assay system can be established at the 50% level Thus, the unit of measurement become a 50% dose and may be expressed in various ways, e.g. • LD5O – (lethal dose 50), • PD5O (paralytic dose 50) • TCID5O (tissue culture infected dose 50) 42 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures • It is also called the endpoint method - find the endpoint dilution at which 50% of the host cells or organisms are damaged This is only a statistical unit • terms of the conditions, e.g. volume of inoculum, route of infection, host system must be defined. Example of the calculation of the 50% end point by the method of Reed & Muench (1938). Table 3: Calculation of the TCID 50 of a virus suspension DEATH / SURVIVAL Virus dilution Lab record D S (P) (N) P P+N D/S Cumulative % ± 10-1 5/5 5 0 22 0 100 10-2 5/5 5 0 17 0 100 10-3 5/5 5 0 12 0 100 10-4 4/5 4 1 7 1 88 10-5 2/5 2 3 3 4 43 10-6 1/5 1 4 1 8 11 10-7 0/5 0 5 0 13 0 50 % Proportionate distance = = = = % 𝑚𝑜𝑟𝑡𝑎𝑙𝑖𝑡𝑦 > 50−50 % 𝑚𝑜𝑟𝑡𝑎𝑙𝑖𝑡𝑦 > 50− % 𝑚𝑜𝑟𝑡𝑎𝑙𝑖𝑡𝑦 < 50 88−50 88−42 38 45 0,8 (i.e. proportional distance between the 10-4 and 10-5 dilution at which 50 % of the host system is affected) By formula: LD50= log of lower dilution + (prof. distance x log. of dilution factor)= 4 + (0,8 x 1) 43 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures By same calculation the original suspension before dilution must contain 63100 LD 50 (Anti log of 8 = 0,6310) per unit volume. A dilution of 10-4,8 contains 1 LD50. Plaque assay In the plaque assay method, the number of plaques produced is proportional to the concentration of the virus inoculated, that is, the dose-response curve is linear. This proportionally indicates that one virus particle is responsible for the formation of each plaque. It also indicates that one virus particle is sufficient to infect a cell. The endpoint method is still used for certain viruses that do not cause sufficient CPE’s recognized as plaques but whose presence can be detected in cultured cells, or for viruses that do not replicate in tissue culture but do cause disease in embryos or adult animals. The virus is serially diluted, and a constant volume of each dilution is inoculated into a number of similar test units (such as mice, chick embryos or cell cultures). At each dilution the proportion of infected test units (infectivity ratio) is scored e.g. • death or disease of an animal or embryo, • • degeneration of a tissue culture, or recognition of progeny virus in vitro The lower dilutions of the virus infect most the test units, and the highest dilutions infect none. The end-point is the last dilution at which virus can be detected in an inoculated culture or animal and that dilution contains at least one infective unit in the volume inoculated. The transition is not sharp, however, and only by combining the data from several dilutions is it possible to calculate the precise endpoint at which 50% of the test units are infected. At this dilution each sample contains on the average one ID50, i.e., one infectious dose for 50% of the test units. Viral titres obtained by the endpoint method are expressed in various equivalents of the ID 50: LD50 (lethal dose) if the criterion is death, PD50 (paralysis dose) if the criterion is paralysis, TC 50 or TCID50 (tissue culture dose) if the criterion is degeneration of a culture. Statistical methods according to Reed & Muench, and Kaber. The interpolation to obtain the ID50 can be carried out in a variety of ways. The method of Reed and Muench (1938), though not mathematically derived, yields results in fair agreement with more rigorous methods. This method is used in conjunction with a series of progressive dilutions of a virus. If the 50% endpoint lies between two dilutions, the dilution containing one ID50 is obtained by interpolation between the two dilutions that straddle the 50% value of the infectivity ratio. The interpolation assumes that in the proximity of the ID 50 the infectivity ratio varies linearly with the log dilution. The interpolated value is given by: % animals affected at dilution next above 50% - 50% % animals affected at dilution next above 50% - % animals affected at dilution below 50% 44 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures This is multiplied by h, which is the log of the dilution factor employed at each step of the serial dilution of the virus. This method of calculation is only justified if one assumes that the fluctuations observed at each dilution are purely due to variations in host sensitivity to the agent under test and not to the chance presence or absence of discrete material particles. Plaque assay technique and factors which influence infective particle counts The plaque method is the fundamental assay method in virus research, and is of great value in diagnosis for it combines simplicity with accuracy and high reproducibility. It was first used with bacteriophages and these were assayed as follows: A phage-containing sample was mixed with a drop of dense liquid culture of suitable bacteria and a few millilitres of melted soft agar at 44°C. The mixture was poured over the surface of a plate or Petri-dish containing a layer of hard nutrient agar. The soft agar spreads in a thin layer and sets, and the bacteriophages diffuse through it until each meets and infects a bacterium. After 20-30 min the bacterium undergoes lysis, releasing several hundred progeny virions. These, in turn, infect neighbouring bacteria, which again lyse and infect new virus. In the meantime, the uninfected bacteria grow to form a dense, opaque lawn and after a day’s incubation the lysed areas stand out as transparent plaques against the dense background. The soft agar permits diffusion of phage to nearby cells, but prevents convection to other regions of the plate and secondary centres of infection cannot form. With animal viruses, a similar method is possible, the bacteria being replaced by a monolayer of cells growing on a solid support, and the medium is replaced by a solution containing serial dilutions of virus. Within an hour or so, most of the virions attach to cells. Soft nutrient agar or some other gelling mixture is poured over the cell layer to minimize the spread of the virus by dispersion, which would occur in liquid medium. A single virus particle infects a cell, and progeny virus produced by that virus spreads to adjacent cells. This process repeats itself and results in a localized area of infection and cell damage that can be visually identified and counted (plaques) after a period of incubation. Plaques are detected in a variety of ways: • The virus often kills the infected cells and produces the so-called CPE. The plaques are the detected by staining the cell layer with a dye that stains only the live cells (e.g. neutral red) or only the dead cells (trypan blue) • With certain viruses, the cells in the plaques are not killed but acquire the ability to absorb red blood cells. The plaques are revealed by haemadsorption (flooding the cell layer with a suspension of red blood cells and then washing out those not attached to infected cells) • The infected cells may fuse with neighbouring uninfected cells to form polykaryocytes which are microscopically detectable (syncytial plaques) • Often the cells of the plaque contain large amounts of viral antigens, which can be detected by immunofluorescence 45 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Each lesion is caused by a single virus particle, and the titre of the viral preparation can be directly calculated from the number of plaques and the dilution of the sample. The amount of virus quantitated by the plaque assay method is expressed as plaque-forming units (PFU). A variation of the plaque assay that is used for tumour viruses that do not cause cell death is the focus assay. A tumour virus causes cell proliferation and the formation of localized area of transformed, proliferating cells called a focus. The units are expressed as focus-forming units (FFU). Some viruses cause localized lesions on the chorioallantoic membrane of the chick embryo, which are called pocks. Each pock is formed by a single virion. STORAGE OF ANTIGEN Antigens /viruses can be stored as wet antigen or in a freeze-dried form. Buffered lactose peptone (BLP) with antibiotics are generally added to the storage medium. • Short-term (1 week – 6 months) Wet material e.g. brain and organs can be stored in storage medium with 5-10% foetal calf serum (FCS) or 5-10% bovine albumin for a short period. • Medium-term (6 months – 1 or 2 years) Only in the presence of 5-10% FCS or bovine albumin. Generally a virus must be stored at –20°C or –80°C. Some virus can be stored under these temperatures in the short term without FCS or bovine albumin. • Long-term (10 or more years) Freeze dry This is the best way to store any virus. Depending on the virus you can freeze dry it without a protein stabilite although it is better to have one present. With this method one need not use very low freezing temperatures such as –20°C, –80°C, or even – 180°C for storing the freeze-dried virus 4°C is considered adequate. The storing agent used for most viruses: • 5-10% bovine albumin or foetal calf serum in BLP • • 1 ml penicillin + 1 ml streptomycin for each 100 ml of BLP Care must be taken to ensure that the virus material is free of contaminants 46 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures FREQUENTLY ASKED QUESTIONS 1. Can a cell culture laboratory be part of a microbiology laboratory? Yes, but specific rooms separated from other diagnostic laboratories should be dedicated to virology. If the laboratory receives samples from humans or samples containing highly infectious agents, a virology unit with all the necessary safety precautions should be used. 2. Is it possible to prepare your own cell culture medium or should one rather buy from a reliable source? It is always better to buy good quality medium but it is possible to produce your own medium and do the sterility testing. 3. Why is it necessary to quantify viruses? For vaccine production, infection of animals in research projects and serology e.g. the serum neutralization and haemagglutination inhibition tests, it is very important to know the concentration of the virus. 4. Can one use cell culture medium without using bovine serum? Serum-free medium is commercially available but the effectivity of the medium for all types of cells may vary. This is currently not commonly used by virology laboratories. 5. Is serology always used to confirm the presence of a virus in a diagnostic sample? The clinical signs and specific host species are a good indication of the cause of the disease. Electron microscopy is also normally used, if available. 6. Is trypsin the best enzyme to use during splitting of cells? Yes – most virology laboratories are using trypsin. 7. Which type of antimicrobial drug should one uses? A broad spectrum, non-toxic antibiotic e.g. gentamycin. Penicillin and streptomycin are also commonly used. 8. How effective is the preparation and use of primary cell cultures? The preparation depends on the type and age of animal tissues used. Primary cultures are very susceptible to isolate viruses especially from the same host species as the culture. 9. Will all viruses give CPE? Not all viruses produce CPE. Arboviruses do not produce CPE in insect cells and a mammalian cell culture or another method should be used to confirm the presence of the virus. Noncytopathic bovine viral diarrhoea virus also e.g. will not produce CPE. 10. Can all cell types grow in the same culture medium? 47 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures Most cells commonly used in a virology laboratory can grow in one basic medium but there are cell types i.e. insect cells that need a specific formulation. REFERENCES 1. Aula P. and Nichols W.W. 1967. The cytogenetic effects of mycoplasma in human leucocyte cultures. Journal of Cell Physiology 70: 281 – 290. 2. Butler M. and Leach R.H. 1964. A mycoplasma which induces acidity and cytopathic effect in tissue culture. Journal of General Microbiology 34: 285 – 294. 3. Freshney R.I. 1987. Culture of Animal Cells: A Manual of Basic Techniques. A.R. Liss, New York. 4. Freshney R.I. 2006. Basic principles of cell cultures. In: Vunjak-Novakovic Gordana and Freshney R. Ian (eds), Culture of cells for tissue engineering, John Wiley & Sons, Inc. pp 4 – 21. 5. Goldsmith Cynthia S. and Miller Sara E. 2009. Modern uses of electron microscopy for detection of viruses. Clinical Microbiology Reviews. 22: 552 – 563. 6. Gray J.J. and Brenwald N.P. 1991. The use of antibiotics to control bacterial overgrowth of cell cultures used for diagnostic virology. Journal of Virological Methods 32: 163 -170. 7. Griffiths J.B. and Riley P.A. 1985. Cell Biology: Basic Concepts. In: Spier R.E. and Griffiths J.B. (ed). Animal and Cell Biotechnology. Academic Press Inc., Orlando FL. USA Vol. 1 pp 17 - 48. 8. Jacobs J., Magrath D.I., Garrett A.J. and Schild G.C. 1981. Guidelines for the acceptability, management and testing of serially propagated human diploid cells for the production of live virus vaccines for use in man. Journal of Biological Standards 9: 331 – 342.Joklik, W.K., 1980. Principles of Animal Virology. Appleton-Century-Crofts, New York. pp 9-11. 9. Life Technologies: Cell Culture Laboratory Safety. 10. Levine E.M., Thomas L., McGregor D., Hayflick L.V. and Eagle H. 1968. Altered nucleic acid metabolism in human cell cultures infected with mycoplasma. Proceedings of the National Academy of Science of the USA 60: 583 -589. 11. Lovelock J.E. and Bishop M.W.H. 1959. Prevention of freezing damage to living cells. Nature 183: 1394 - 1395. 12. MacPherson I. and Russel W. 1966. Transformants in hamster cells mediated by mycoplasmas. Nature 210: 1343 – 1345. 13. Mazur P. 1970. The freezing of biological systems. Science 168: 939 - 949. 48 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures 14. Mazur P. 1977. The role of intracellular freezing in the death of cells at supraoptimal rates. Cryobiology 14: 251 - 272. 15. McGarrity G.J., Phillips D. and Vaidya A. 1980. Mycoplasmal infection of lymphocyte cultures: infection with M salvarium. In vitro cellular and Developmental Biology 16: 346 – 356. 16. Paul J. 1975 Cell and Tissue Culture, pp 256 - 257, 5th ed., Churchill Livingston, Edinburgh. 17. Polge C., Smith A.U. and Parkes A.S. 1949. Revival of spermatozoa after vitrification and dehydration at low temperatures. Nature 164: 1394. 18. Poole C.A., Reilly H.C. and Flint M.H. 1982. The adverse effects of HEPES, TES, and BES zwitterionic buffers on the ultra-structure of cultured chick embryo epiphyseal chondrocytes. In vitro 18: 755 - 765. 19. Raetz C.R.H. 1990. Biochemistry of endotoxin. Annual Review of Biochemistry, 59: 129 – 170. 20. Reed L J & Muench H 1938. A simple method of estimating fifty per cent (50 %) endpoints. American Journal of Hygiene 27: 493 – 497. 21. Schaeffer W. I. 1990. Terminology associated with cell, tissue and organ culture, molecular biology and molecular genetics. In Vitro Cellular and Developmental Biology 26: 97-101. 22. Schaffner 1979. Animal and plant tissue culture decontamination. In: Maramorosh K & Hirumi H (eds) Practical Tissue Culture Applications, Academic Press Inc.m, New York. pp. 203-214. 23. Shipman C. Jr 1969. Evaluation of 4- (2-hydroxyethyl) - 1 piperazineethane sulfonic acid (HEPES) as a tissue culture buffer. Proceedings of the Society for Experimental Biology and Medicine 130: 305 - 310. 24. Stanbridge E.J., Hayflick L. and Perkins F.T. 1971. Modification of amino acid concentrations induced by mycoplasmas in cell culture medium. Nature 232: 242 – 244. 25. Wiedemann B. and Atkinson B.A. 1991. Susceptibility to antibiotics: species incidence and trends. In: Lorian V (ed) Antibiotics in Laboratory Medicine, pp. 962- 1150. Williams & Wilkins, Baltimore. 26. Wise K.S., Cassel G.H. and Action R.T. 1978. Selective association of murine T lymphoblastoid cell surface alloantigens with Mycoplasma hyorhinis. Proceedings of the National Academy of Sciences of the USA 75: 4479 – 4483. Websites 1. Gibco® Cell culture basics. http://www.lifetechnologies.com/za/en/home/references/gibco-cellculture-basics.html 2. Cell culture Basics. Handbook GIBCO®, Invitrogen. http://www.vanderbilt.edu/viibre/CellCultureBasicsEU.pdf 49 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures 3. http://www.lifetechnologies.com/za/en/home/references/gibco-cell-culture-basics/introduction-tocell-culture.html 4. http://www.lifetechnologies.com/za/en/home/references/gibco-cell-culture-basics/cell-culturelaboratory-safety.html 5. http://www.worthington-biochem.com/tissuedissociation/dissociatingenzymes.html 6. http://www.worthington-biochem.com/tissuedissociation/working.html 7. http://www.worthington-biochem.com/tissuedissociation/trypsinharvesting.html 8. http://www.worthington-biochem.com/tissuedissociation/optimization.html 9. http://www.worthington-biochem.com/tissuedissociation/cellquantitation.html 10. http://www.worthington-biochem.com/tissuedissociation/glossary.html 11. SIGMA-ALDRICH: Fundamental Techniques in Cell Culture Laboratory Handbook http://www.sigmaaldrich.com/life-science/cell-culture/learning-center/ecacc-handbook/cellculture-tech-glossary.html 12. http://www.sigmaaldrich.com/technical-documents/protocols/biology/safety-aspects-of.html 13. http://www.sigmaaldrich.com/technical-documents/protocols/biology/cryopreservation-and.html 14. http://www.sigmaaldrich.com/technical-documents/protocols/biology/cryopreservation-of.html 15. ATCC Animal Cell culture guide; tips and techniques for continuous cell lines. http://www.summitpharma.co.jp/japanese/service/ATCC_Animal_Cell_Culture_Guide_low_res.p df 16. http://www.stanford.edu/dept/EHS/prod/researchlab/bio/docs/types_biosafety_cabinets.pdf 17. https://www.google.co.za/search?q=biosafety+cabinet&rlz=1T4RNQN_enKE485ZA486&tbm=isc h&tbo=u&source=univ&sa=X&ei=LKvXUoLtK8fm7AajYCYBQ&ved=0CE0QsAQ&biw=1366&bih=533 18. http://www.bakerco.com/intro-to-biological-safety-cabinets.html 19. http://virology-online.com/general/Safety5.htm 20. http://virology-online.com/general/Safety9.htm 21. http://www.who.int/vaccines/en/poliolab/webhelp/Chapter_04/4_1_Working_in_the_cell_culture_l aboratory.htm 22. http://www.millipore.com/lab_water/clw4/cell_culture 23. http://www.abcam.com/ps/pdf/protocols/cell_culture.pdf 50 | P a g e Applied Veterinary Virology: The isolation and identification of viruses using cell cultures 24. http://www.bioind.com/page_13875 25. Ryan J. CORNING Technical Bullettin http://www.level.com.tw/html/ezcatfiles/vipweb20/img/img/20297/contamination-COR.pdf 26. http://www.microbelibrary.org/component/resource/laboratory-test/2875-cytopathic-effects-ofviruses-protocols 27. Albrecht Thomas, Fons Michael, Boldogh Istvan and Rabson Alan S 1996. Effects on cells. In: Medical Microbiology, The University of Texas Medical Branch at Galveston. http://www.ncbi.nlm.nih.gov/books/NBK7979/ 28. http://www.mansfield.ohio-state.edu/~sabedon/biol2065.htm 29. http://web.uct.ac.za/depts/mmi/stannard/cpeherps.html 30. http://www.biolcell.org/boc/100/0491/1000491.pdf 51 | P a g e