BIO 208 - Microbiology - Unit 4 - Diseases of Skin, Nervous System
advertisement

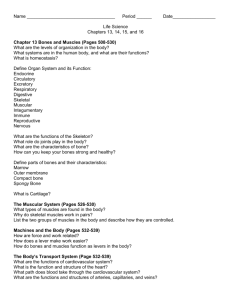
BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems This outline is intended to facilitate your preparation for lecture. This web outline will NOT substitute for regular lecture attendance. For the rest of Unit 4 we will discuss: Significant or Interesting Human Diseases Key to Understanding Infectious Diseases: • • • • • Microbes are as old as the planet Humans evolved under the selective pressure of microbes Microbes see our bodies as just another habitat In all the vast diversity of microbial life, only the smallest fraction of microbes are capable of causing illness For any infection with a potential pathogen, there are a wide variety of possible outcomes A. Diseases of the skin General background Main pathogens of the skin Staphylococcus aureus GPC, cat + Streptococcus pyogenes GPC, cat - Skin diseases caused by S. pyogenes Group A Strep (GAS) 1. impetigo 2. erysipelas – infection of dermal layer of skin 3. invasive GAS - 10,000-15,000 cases/yr; 2,000 deaths/yr a. streptococcal toxic shock syndrome (TSS) 2,000-3,000/yr; 60% fatal 1 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems The class vote -Disease - necrotizing fasciitis (a.k.a. flesh-eating strep) Agent – phage-infected strain of group A Streptococcus pyogenes (bacterium, GPC, cat-) frequently initiates the infection, but infection often becomes “polymicrobial” with aerobic and anaerobic pathogens, including Bacteroides, Clostridium, Peptostreptococcus, Enterobacteriaceae, coliforms, Proteus, Pseudomonas, and Klebsiella. Similar clinical course may be seen with Clostridium perfringens and some strains of S. aureus (e.g., MRSA). Virulence factors (what factors does this strain have that other strains do not, that makes this one capable of causing disease) Only strains of. S. pyogenes that are parasitized by lysogenic bacteriophages are virulent – lysogenized strains produce a phage-encoded streptococcal pyrogenic exotoxin (SPE) that is responsible for tissue destruction. A second toxin called exotoxin A interferes with a coordinated immune response. Transmission - direct contact through some minor wound (community-acquired) or through a surgical incision (hospital-acquired) Medical description of disease - “a progressive, rapidly-spreading, inflammatory infection located in the deep fascia, with secondary necrosis of the subcutaneous tissues”. Clinical picture – very rapid progression from trivial wound to gangrene and shock. Take a few notes off the powerpoint Treatment – must be aggressive – life support, IV antibiotics, surgical debridement and amputation. Frequency – More rare. - Since 2004, increasing number of cases due to MRSA. Mortality – overall 70-80%; lowered to 20% with aggressive treatment. Prevention - wash hands, keep wounds clean and watch them. 2 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems B. Diseases of the nervous system General background Nerves Brain Encephalitis - inflammation of the encephalon (the brain itself) Encephalitis is usually caused by viruses or, in rare cases, by protozoa. Always serious, often fatal. The class vote – Disease - Rabies Agent – Lyssavirus (Family Rhabdoviridae; ss RNA virus, enveloped) Virulence factors – evades immune detection in the nervous system. Spreads cell to cell in brain,, causes dysfunction in infected cells. Transmission – direct contact with saliva of an infected animal Clinical Picture –Take a few notes off the powerpoint Treatment – within 14 days of bite (the sooner the better) - post-exposure prophylaxis. Once clinical signs begin, there is no treatment. Frequency – very rare in humans in the U.S. Mortality – 100% (due to paralysis of respiratory/cardiac systems) Prevention – vaccinate people at high risk (veterinarians, animal control, etc) 3 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems C. Diseases of the cardiovascular and lymphatic systems General background The class vote – Disease – plague Ancient – described in Old Testament 3 great historical plague pandemics Justinian’s plague – 6th century – lasted 60 years, killed 100 million Black Death – 14th century – killed 25 million in Europe alone (add in Asia, etc, unknown #) Modern Pandemic – 1896-1930 Agent – bacterium Yersinia pestis (GNR, ox-; an Enterobacteriaceae (as is E. coli). Virulence factors Very complex 3 different plasmids carrying multiple virulence genes, the products of which are used for invading host tissue, evading host immune responses, and producing toxins Transmission Natural disease of rodents; rats are classic primary reservoir; in US it is wild rodents. Humans are accidental hosts and are not critical for maintenance of disease. Rat fleas are intermediate hosts and vectors, carrying bacteria from one mammalian host to another while feeding. Flea-borne, from infected rodents to humans Direct contact with infected tissues or fluids from handling sick or dead animals Respiratory droplets from cats and humans with pneumonic form of plague 4 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems Clinical picture 1. Bubonic plague - a very painful, usually swollen, and often hot-to-the touch lymph node, called a “bubo”. 2. Pneumonic plague - characterized by development of an overwhelming pneumonia with high fever, cough, bloody sputum, and chills. 3. Septicemic plague – characterized by bacterial spread in the bloodstream and necrosis of the tissues (“Black death”) Treatment – antibiotics (streptomycin or tetracycline) if early. Frequency – In US, last urban outbreak was Los Angeles, 1924-25. Now about 18 cases/year. Mortality – Mortality 50-90% if untreated; 15% when diagnosed and treated. Prevention – surveillance of infected animals, vectors, and human contacts. Destruction of plague-infested animal populations. 5 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems FYI 1 (additional nervous system disease) Disease - Epidemic bacterial meningitis Agent - Neisseria meningitidis (bacterium, GNC, ox+) Virulence factors - 3 1. capsule - evade phagocytosis by host immune cells 2. lipopolysaccharide (lps) – induces inflammation 3. fimbriae – allows for attachment to meninges Transmission Humans are only host 5-20% of population are asymptomatic carriers – higher end on college campuses Transmitted through the air by respiratory droplets resulting from sneezing and coughing and from direct contact, such as kissing or sharing items with an infected person. College students may have an increased risk of meningitis related to features in campus life. These include active and passive smoking, going to bars, consuming alcohol, and living in close quarters (residence halls). Freshmen living in dormitories are at the greatest risk -- more than 7 times higher than undergraduates in general. Clinical Picture – very rapid progression from flu-like to death (within hours) – can kill more rapidly than any other infectious disease. Take a few notes off the powerpoint Treatment – must be aggressive – IV antibiotics, life-support Frequency - The disease strikes nearly 3,000 Americans each year, and results in 300 deaths annually (100-125 college students are infected yearly, resulting in 5-15 deaths). Of those who survive, one in five suffers a permanent disability due to amputation, brain damage, hearing loss, and seizures. Mortality - The mortality rate is approximately 5% in children and 5-10% in adults; however, meningococcemia associated with DIC (disseminated intravascular coagulation) has a mortality rate of greater than 90%. Prevention – Vaccine for some strains 6 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems FYI 2 (additional cardiovascular disease) Viral Hemorrhagic Fever Syndrome widespread vascular damage, leaky small RNA viruses, lipid envelope zoonotic persist in nature most infectious via aerosol 4 families – All are RNA viruses! Arenaviridae - Machupo, Lassa Bunyviridae – hantavirus (same as in our epidemiology mystery case), Rift Valley Flaviviridae - dengue, yellow fever Filoviridae - Marburg, Ebola Disease – Ebola hemorrhagic fever Agent – Ebola virus Two main human infectious strains: Ebola Zaire Ebola Sudan Virulence factors – still under investigation ? ability to evade host interferon? (a chemical produced by infected host cells that interferes with viral replication) ? ability to evade immune defenses that are normally activated early against viral infections Transmission – blood, aerosol (candidate biowarfare agent) History of the Emergence of Ebola Clinical Picture Incubation Early Later 5-7 days 7-16 days needle transmitted 5-7 days; person-person transmission 6-12 days sudden onset fever, severe headache, severe muscle/body aches – resembles bad case of Influenza at this stage nausea, abdominal pain, vomiting, diarrhea focal necrosis of vascular endothelium leading to hemorrhaging death due to shock (severe drop in blood volume) Treatment – No specific treatment for the virus (i.e., no anti-viral drugs) – supportive care only (fluids, electrolytes, comfort care) Frequency – 4 outbreaks of Ebola Sudan (1976-2004); 11 outbreaks of Ebola Zaire (1976-2004) Mortality – 65%-89% 7 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems Prevention – Interruption of person-person spread *Interesting note - Semen from men recovering from Ebola infection has been shown to contain infectious virus, and Ebola has been transmitted by sexual intercourse involving recovering men and their sex partners. 8 BIO 208 Microbiology. Unit 4. Diseases of skin, nervous and cardiovascular systems FYI 3 (additional disease that can target skin, nervous, and/or cardiovascular system) Disease - Lyme Disease – emerged in 1975 Agent - Borrelia burgdorferi – bacterium, GN spirochete Transmission - Transmitted to humans through bite of infected deer tick Clinical Picture - 3 phases 1. 7-10 days post bite - local reaction -expanding ring-shaped lesion (bull’s eye rash), flu-like symptoms 2. Weeks - months later – disseminated, spreads throughout the body - neurological abnormalities, heart inflammation, arthritis 3. Years later - late stage – nervous system degeneration = neuroborreliosis – why?? Perhaps triggers and autoimmune response that attacks the nervous system? Treatment - Antibiotics early in illness Frequency - Most common tickborne disease in U.S. 10,000+ cases/yr Natural hosts - deer and field mice Prevention 1. Highest transmission May-July 2. Light colored pants with pant legs tucked into socks 3. Insecticide for ticks 4. Examine your body for ticks, shower w/ lots of soap 5. Prompt removal of ticks 9