Medication Reconstitution Guide for Pharmacy Technicians
advertisement
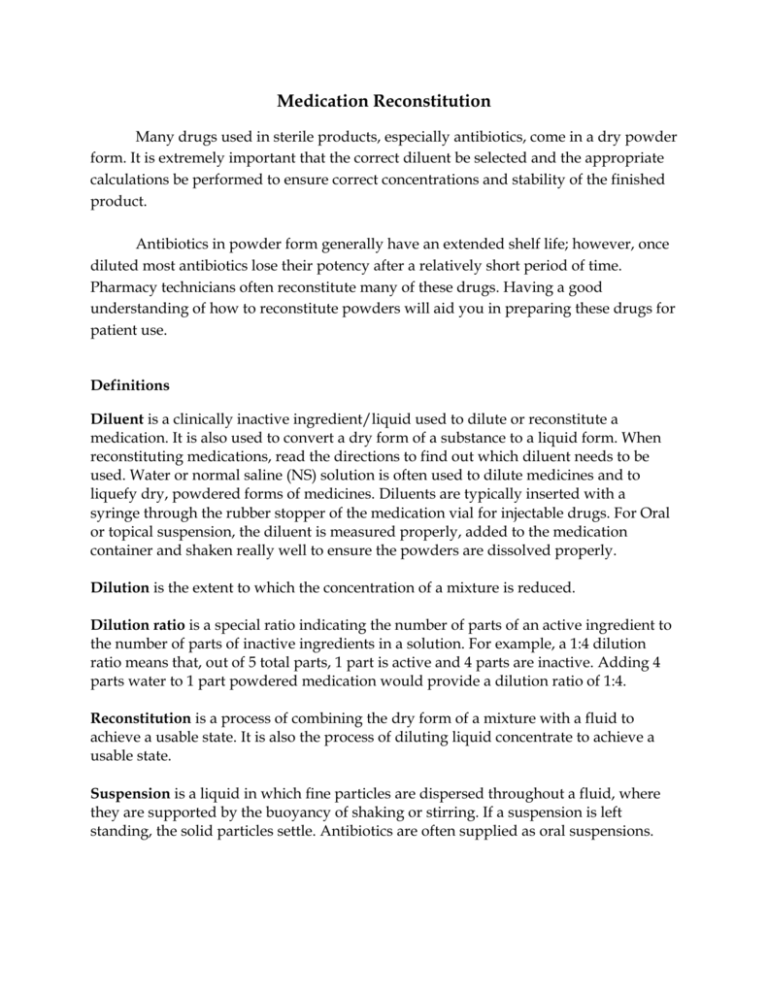
Medication Reconstitution Many drugs used in sterile products, especially antibiotics, come in a dry powder form. It is extremely important that the correct diluent be selected and the appropriate calculations be performed to ensure correct concentrations and stability of the finished product. Antibiotics in powder form generally have an extended shelf life; however, once diluted most antibiotics lose their potency after a relatively short period of time. Pharmacy technicians often reconstitute many of these drugs. Having a good understanding of how to reconstitute powders will aid you in preparing these drugs for patient use. Definitions Diluent is a clinically inactive ingredient/liquid used to dilute or reconstitute a medication. It is also used to convert a dry form of a substance to a liquid form. When reconstituting medications, read the directions to find out which diluent needs to be used. Water or normal saline (NS) solution is often used to dilute medicines and to liquefy dry, powdered forms of medicines. Diluents are typically inserted with a syringe through the rubber stopper of the medication vial for injectable drugs. For Oral or topical suspension, the diluent is measured properly, added to the medication container and shaken really well to ensure the powders are dissolved properly. Dilution is the extent to which the concentration of a mixture is reduced. Dilution ratio is a special ratio indicating the number of parts of an active ingredient to the number of parts of inactive ingredients in a solution. For example, a 1:4 dilution ratio means that, out of 5 total parts, 1 part is active and 4 parts are inactive. Adding 4 parts water to 1 part powdered medication would provide a dilution ratio of 1:4. Reconstitution is a process of combining the dry form of a mixture with a fluid to achieve a usable state. It is also the process of diluting liquid concentrate to achieve a usable state. Suspension is a liquid in which fine particles are dispersed throughout a fluid, where they are supported by the buoyancy of shaking or stirring. If a suspension is left standing, the solid particles settle. Antibiotics are often supplied as oral suspensions. Unstable means that the pharmaceutical formula is easily broken down to a state of diminished effectiveness. Breakdown can occur rapidly with reconstituted solutions. Foods, solutions, and certain medications that are unstable, such as reconstituted medications, have a short shelf life. They must be discarded if they are not used in a timely manner. Sterile Container – the contents of the medication container is free of biologic contaminants (example: bacterial or viral). Diluent Identification Some medications are very unstable in liquid form. Therefore, they are supplied in a dry form to which an inactive diluent is added just before use. The information about the specific type and amount of diluent to be added to achieve specific concentrations is provided on the product label. Selecting the correct diluents (liquid or solution) is important in reconstituting a medication. Incorrect diluents used can affect the medication’s stability, efficacy and safety. Use of the incorrect diluent may result in loss of potency of the medication, an unwanted chemical interaction, or a shorter period of stability of the reconstituted medication. The information regarding the correct diluent to be used is clearly written on the product label. To ensure that the ingredients are compatible or incompatible with the diluent, the pharmacist or pharmacy technician should check the reference books available in the pharmacy or may consult the product information leaflet. Common Diluents for injectable drugs Normal saline is a term commonly used interchangeably with 0.9% sodium chloride (NaCl) injection and is the concentration of sodium chloride within the human blood stream. For reconstituting powder for oral suspension, Sterile water is commonly used as diluent to dissolve the powder. Standard Name Dextrose 5% in Water Lactated Ringers Normal Saline Sterile Water for Injection Bacteriostatic Water Alternate Name Common Abbreviation 5% Dextrose Injection D5W Ringers Lactate LR 0.9% Sodium Chloride Injection NS SWFI BW Measuring device / equipment used to measure diluents/liquids for reconstitution 1. Graduated Cylinder 2. Calibrated Medication cup 3. Syringe 4. Beaker Reconstituting Medications 1. Interpreting Prescription Orders and Reading Labels for Reconstituted Medications Sample A. Examine the directions on the following label for an oral suspension to be reconstituted: Rx: Amoxicillin 200mg/5ml suspension The order includes the form, oral suspension, but does not mention that the drug requires reconstitution or describe how to prepare it. The pharmacist or pharmacy technician must read the medication label and / or product information to determine how to prepare the medication. Reading Labels Directions on the label state the precise amount and type of liquid diluent to add in order to achieve specific dilutions or concentrations of the drug per milliliter. The directions always state conditions and time limits for storage after reconstitution to liquid form. Some products must be discarded immediately, while others may be refrigerated for several hours to several days so that they can be used for additional doses. Examine and interpret the medication label: 1. The route is oral. This is important to note because there are injectable antibiotics and other drugs with similar names made specifically for intramuscular or intravenous routes. Diluents for oral preparation do not necessarily need to be sterile whereas the sterility of the diluent is very important for injectable medications. 2. The type of diluent is water. Most oral suspension diluents use tap water unless otherwise specified. Pediatric patients and immunocompromised patients may need Sterile water to ensure bacterial content of the diluent is avoided. 3. The total amount of diluent to be added is 57 mL, can be added in two parts: 30 mL for the first mix and add the remaining 27 mL for the second in order to avoid lumping of the suspension. 4. After reconstitution, the drug concentration will yield 200 mg/ 5 mL water. The total amount of medication is 75 mL, although only 57 mL of water was added. This discrepancy is due to displacement of liquid by the powder. Both ingredients occupy space. 5. Discard after 14 days. Refrigeration after reconstitution is preferable to ensure stability of the medication. It is important to educate the patient on the storage condition once the powder is reconstituted. Sample B. Read and interpret the prescription label and indicate the required information below (checklist): 1. Form and route of medication: Oral Suspension 2. Type of diluent to be used: Water 3. Amount of diluent to add to bottle: 47.6 ml 4. Mixing directions: Add 47.6ml of water gradually and shake well. 5. Unit dose concentration after reconstitution: 25mg per 5 ml 6. Total volume in container after reconstitution: 60ml 7. Number of unit doses in container after reconstitution: 12 unit doses of 5 mls 8. Storage location and condition in dry form: room temperature at 30°C 9. Storage location after reconstituted: room temperature 10. Expiration, or discard, time after reconstitution: 14 days 11. Additional instruction to patient: Shake well before using Sample C. Calculating, reconstituting and measuring doses and interpreting the prescription order Rx order: Erythromycin susp. 300mg tid x 7 days 1. Form and route of administration: Oral Suspension 2. Amount and type of diluent to be added: 77 mls of water 4. Mixing directions: Add 77mls of water gradually and shake well. 5. Unit dose concentration after reconstitution: 200 mg per 5 ml 6. Total volume in container after reconstitution: 100 ml 7. Storage location and condition in dry form: room temperature at 30°C 9. Storage location and condition after reconstituted: refrigerate, do not freeze 10. Expiration, or discard, time after reconstitution: 10 days 11. Additional instruction to patient: Shake well before using; medication may be taken with or without food Prescription interpretation: Rx: Erythromycin 300mg tid x 7 days Interpretation: Take 300mg three times a day for seven days. Calculation: Once reconstituted, the suspension will yield 200mg per 5 mls. The prescription order requires the patient to take 300mg per dose. Calculate the equivalent volume in mls of the reconstituted suspension to yield 300mg per dose. 1. Use ratio and proportion: 200mg : 5ml:: 300mg: X X = 300mg x 5 ml 200mg X = 7.5 ml per dose equivalent of 300mg Erythromycin 2. Calculate the amount of medication needed to be dispensed: = 7.5 mls (amount per dose) x 3 (three times a day-frequency of administration) x 7 days (duration of treatment) Answer: 157.5 mls 3. Round up the quantity. The bottle will yield 100 mls of reconstituted suspension, since we cannot break the bottle, 2 x 100mls Erythromycin 200mg/5ml suspension will be dispensed to the patient to be consumed for the treatment duration indicated (7 days). Special instruction to “discard the remainder” of the suspension should be given to the patient during patient counseling. 4. Prescription Labeling: Dawood Khan National Military Hospital Pharmacy Department Dr. Omar Abdullah Date: 20 April 2013 Patient: Ali Karimi Father: Abdul Karimi Medication: Erythromycin 200mg/5ml susp Quantity: 200 mls Directions: Take 7.5 mls (300mg) three times daily for 7 days. *Keep in the refrigerator. Discard the remainder *May be taken with or without food *Shake well before using Reconstituting Injectable Medications Before you can produce a reconstituted product, you need to read the package insert or drug label to identify the proper diluent when reconstituting a powder for IM or IV injection. Diluents are used to prepare powdered medications for transfer to IV solutions. Not all diluents are suitable to reconstitute injectable medications. Calculate amounts of reconstituted solutions: 1. Use the provided resources, especially the label and package insert. 2. Double check units in all calculations. 3. Ensure your answers make sense by working the problem in reverse or solving for a different factor. Determine the correct diluent: 1. Always use your reference materials. 2. Determine if you need bacteriostatic or sterile agents. 3. Ensure the information on a diluent label or product label matches what is in the reference material.