use of dexmedetomidine for icu sedation in pediatric and
advertisement

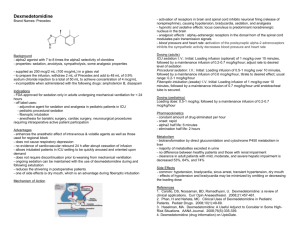
REVIEW ARTICLE USE OF DEXMEDETOMIDINE FOR ICU SEDATION IN PEDIATRIC AND ADULT PATIENTS Sahana K.S1, Sunil B.V2 HOW TO CITE THIS ARTICLE: Sahana K.S, Sunil B.V.“Use of Dexmedetomidine for ICU sedation in Pediatric and Adult Patients”. Journal of Evolution of Medical and Dental Sciences 2013; Vol. 2, Issue 51, December 23; Page: 9876-9889. ABSTRACT:All Critically ill patients either pediatric or adult are routinely provided analgesia and sedation to prevent pain and anxiety, permit invasive procedures, reduce stress and oxygen consumption, and improve synchrony with mechanical ventilation.Dexmedetomidine (DEX), a highly selective α2-adrenergic receptor agonist, is the newest agent introduced for sedation in intensive care unit (ICU) and perioperative care. We analysed Medline and Science Citation Index, articles of last 13 years involving DEX in ICU and sedation for pediatric and adult patients. α 2-Adrenoceptor agonists have several beneficial actions during the perioperative period. They decrease sympathetic tone, with attenuation of the neuroendocrine and hemodynamic responses to anesthesia and surgery; reduce anesthetic and opioid requirements; and cause sedation and analgesia. They allow psychomotoric function to be preserved while letting the patient rest comfortable. The sedation strategy for critically ill patients has stressed light sedation with daily awakening and assessment for neurologic, cognitive, and respiratory functions. Sedation with dexmedetomidine differs from sedation with other commonly used sedatives such as propofol or midazolam. Sedation induced by DEX, mimics Non rapid eye movement sleep, which can be easily arousable without respiratory depression. Because α2-agonists provide analgesia and sedationwhich mimics natural sleep without respiratory depression, they represent an interesting alternative to GABA agonists. Over sedation, however, occurs commonly and is associated with worse clinical outcomes, including longer time on mechanical ventilation, prolonged stay in the intensive care unit, and increased brain dysfunction (delirium and coma).DEX has many advantages like characteristic feature of sedation, together with a concomitant opioid sparing effect, may decrease the length of time spent on a ventilator, length of stay in ICU, and prevalence and duration of delirium, as the evidence shown from several comparative studies. Use of DEX is increasing in pediatric ICUs, but the availability of literature is limited in that group.In addition, DEX has an excellent safety profile. The primary objective of this study was to capture data on the safety and advantages of dexmedetomidine (specifically, adverse events) in critically ill children and adult.In conclusion, DEX is considered as a promising agent optimized for sedation in ICU for both peadiatric and adult population. KEYWORDS:Dexmedetomidine, Delirium, ICU, Sedation. INTRODUCTION: The ideal sedative agent for use in critically ill children should be effective and short-acting, has a rapid onset of action, lacks active metabolites, does not accumulate in patients with renal or hepatic dysfunction, has minimal to no cardiovascular or respiratory adverse effects, and has few drug interactions. In critically ill patients, pain and anxiety contribute to an already prominent sympathetic stress response that includes increased endogenous catecholamine activity, increased oxygen consumption, tachycardia, hypercoagulability, hypermetabolism, and immunosuppression1. Sedation is frequently required for critically ill infants and children as adults for comfort and to prevent self-extubation or removal of IV catheters. ICU stay may also contribute Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9876 REVIEW ARTICLE to significant physical and psychological stress during the acute event and in the future, long-term consequences such as posttraumatic stress disorder (PTSD) may develop.2 Analgesia and sedation, therefore, are administered to provide patient comfort and ensure patient safety while decreasing the stress response. However oversedation occurs frequently and is associated with longer time on mechanical ventilation and in the intensive care unit (ICU), greater need for radiological evaluations of mental status and higher probability of developing brain dysfunction.3-5 (delirium and coma). A wide discrepancy exists in the approach and administration of these medications due to patient and provider variability, bias, and regional preference.1 Analysis of sleep spindles shows that dexmedetomidine produces a state closely resembling physiologicalsleep in humans, which gives further support to earlier experimental evidence for activation of normal non-rapid eye movement sleep-promoting pathways by this sedative agent. Because α2-agonists provide analgesia and sedation without respiratory depression, they represent an interesting alternative to GABA agonists.6 Despite profound sedative properties, dexmedetomidine is associated with only limited respiratory effects, even when dosed to plasma levels up to 15 times those normally achieved during therapy, leading to a wide safety margin.7 However, GABA-mimetic sedatives have significant limitations including delirium, respiratory depression, dependence and withdrawal. Traditional agents (Benzodiazepine [BDZ], Propofol) which act on the GABA receptor whereas DEX acts on subtypes of α2-adrenergic receptor, which include α2A, α2B, α2C; DEX seems to produce its therapeutic effects primarily through the α 2A receptor.8, 9 In 1990s dexmedetomidine a highly selective alpha 2 agonist with a 1600:1 ratio of alpha2:alpha1 receptor binding (8 -10 fold stronger binding then clonidine) was introduced as a short term intravenous sedation in intensive care. Adult patients receiving long-term dexmedetomidine infusion had similar rates in terms of mortality rate at one month, hospital and ICU LOS[length of stay],rate of re intubation when compared with the short-term infusion group. Moreover patients in both groups had similar days on mechanical ventilation.10 A number of studies have been undertaken to evaluate the efficacy and availability of DEX in various clinical fields including sedation for critically ill patients, adjuvant for general and regional anesthesia, monitored anesthesia care for some invasive procedures, postoperative analgesia, stabilization of heart in cardiac surgery or procedures and pediatric/adult ICU since its approval by the FDA in 1999.11.Among these, especially in the area of sedation in ICU, DEX is expected to play a role in relation to its unique features of action. Now DEX is increasingly used in peadiatric ICUs for sedation but the existing literature is limited.The sedative strategy for critically ill patients has emphasized light sedation with daily awakening and assessment for neurologic, cognitive, and respiratory functions, since SCCM guidelines were presented in 2002 and concerns on adverse effects associated with oversedation emerged.12 Thus, there are growing interests on DEX as a possible alternative. The primary site of action in the brain for DEX is the locus ceruleus (LC).13 LC plays a key role in regulation of arousal and autonomic activity through numerous projections to multiple sites, including the sleep promoting nucleus and autonomic nucleuses.14Inhibition of norepinephrine (NE) release from LC by DEX depresses alertness and sympathetic activity, which present sedation, hypotension, bradycardia, decreased cardiac output.13 The alpha 2 adrenergic agonist acts by binding to pre synapyic C fibre and post synaptic dorsal horn neurons. Intrathecal alpha 2 Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9877 REVIEW ARTICLE adrenergic agonist produce analgesia by depressing the realease of C fibretransmission by hyperpolarization of post synaptic dorsal horn neurons..15 Dexmedetomidine Use in Pediatric Intensive Care: Based on its efficacy in adults, dexmedetomidine is now being explored as an alternative or adjunct to benzodiazepines and opioids in the pediatric intensive care setting. This review describes the studies evaluating the safety and efficacy dexmedetomidine in infants and children and provides recommendations on dosing and monitoring. In several papers, dexmedetomidine use resulted in a reduction in the dose or discontinuation of other sedative agents.Dexmedetomidine offers an additional choice for the sedation of children receiving mechanical ventilation in the intensive care setting or requiring procedural sedation. While dexmedetomidine is well tolerated when used at recommended doses , it has the potential to cause hypotension and bradycardia and requires close monitoring. However, data on the use of dexmedetomidine in critically ill children for periods exceeding 48 h are lacking. The pharmacokinetic profile of dexmedetomidine in children has been assessed in several studies.16-20In 2006, a two-center study evaluated the pharmacokinetics and pharmacodynamics of dexmedetomidine in children undergoing surgery.16Thirty-six children between 2 and 12 years of age were assigned to receive dexmedetomidine infusions of 2, 4, or 6 mcg/kg/hr for 10 minutes or placebo. Plasma protein binding of dexmedetomidine was 92.6 ± 0.7%. The estimated central volume of distribution was 0.81 L/kg, with a peripheral volume of distribution of 1 L/kg. The estimated systemic clearance rate was 0.013 L/kg/min, with a terminal half-life of 1.8 hours. In a second pharmacokinetic study, 10 children ranging in age from 4 months to 7.9 years who received dexmedetomidine during postoperative mechanical ventilation were assessed.17They were given an IV loading dose of 1 mcg/kg, followed by an infusion of 0.2 to 0.7 mcg/kg/hr. Treatment continued for an average duration of 18.8 hours (range 8–24 hours). The average volume of distribution at steady state was 2.53 ± 0.37 L/kg, with an average clearance of 0.57 ± 0.14 L/hr/kg and a terminal elimination half-life of 2.65 ± 0.88 hours. The authors of both of these studies concludedthat dexmedetomidine pharmacokinetic parameters in children were similar to those of adults. The following year, a third dexmedetomidine study evaluated the effects of age on pharmacokinetic parameters.18Eight children between 28 days to 23 months of age and another eight between 2 and 11 years of age were studied after receiving a single 1 mcg/kg IV dose of dexmedetomidine for procedural sedation. Clearance was not significantly different between the groups, 17.4 mL/kg/min in the younger children and 17.3 mL/kg/min in the older children, but the median volume of distribution at steady state was significantly larger in the younger children (3.8 L/kg versus 2.2 L/kg, p<0.05). Elimination half-life was also significantly longer in the younger children, with a median of 139 minutes compared to 96 minutes in the older subjects (p<0.05). An additional study, a population pharmacokinetic analysis using nonlinear mixed effects modeling, was published in 2008.19One hundred forty-eight observations were obtained from 45 children, 4 days to 14 years of age, who received dexmedetomidine after cardiac surgery. A two-compartment model with first order elimination was chosen based on the best fit of these data. Clearance was estimated at 39.2 L/hr per 70 kg (CV 30.36%) and central volume of distribution at 36.9 L per 70 kg (CV 69.49%). The authors estimated that clearance rates in neonates were approximately one-third of adult values, but reached 87% of adult values by 1 year of life. The differences in the results of these four studies may be partially explained by the age distribution of the samples. The minimum age in Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9878 REVIEW ARTICLE the first study was 2 years and only three patients less than 1 year of age were included in the second study, which may have prevented the authors from detecting the slower clearance in younger children observed in two subsequent papers. A recent pooled analysis of the data from all four pediatric dexmedetomidine pharmacokinetic studies confirms this observation.20 ADVERSE EFFECTS: The most significant adverse reactions associated with dexmedetomidine are hypotension and bradycardia, resulting from its sympatholytic activity. Both hypotension and bradycardia have been reported in several pediatric studies, although rarely have the changes been clinically significant or required intervention to correct. However, dexmedetomidine should be used with caution in patients already at risk for arrhythmias or hemodynamic instability. In a study of 12 children undergoing ablation of supraventricular accessory pathways, administration of dexmedetomidine (1 mcg/kg IV loading dose followed by an infusion of 0.7 mcg/kg/hr) resulted in a significant decrease in heart rate and transient hypertension.21Dexmedetomidine-induced hypotension or bradycardia resolves with dose reduction and administration of IV fluid boluses. Large-dose dexmedetomidine has been used by some clinicians to increase the rate of successful procedural sedation, but this regimen has resulted in increased numbers of patients with adverse hemodynamic effects.22 A recent retrospective study of 747 children evaluated the safety and efficacy of large-dose therapy, with IV loading doses of 2–3 mcg/kg followed by infusions of 1–2 mcg/kg/hr. While the authors achieved adequate sedation in 97% of their patients, there was a 16% incidence of bradycardia. The rate of bradycardia was no different in patients who received additional pentobarbital when compared to those given dexmedetomidine alone. None of the patients with bradycardia required intervention.23 Clinically significant hypertension has been reported in isolated pediatric cases, 24 but has not been common in larger case series.25 Transient hypertension has been reported with the administration of the loading dose due to initial vasoconstriction caused by stimulation of peripheral postsynaptic alpha2B-adrenergic receptors. The ability of dexmedetomidine to produce hypotension or bradycardia may be magnified by administration with other drugs capable of producing those effects. In a study comparing midazolam and dexmedetomidine, the authors observed a case of bradycardia in a 5-week-old infant receiving both dexmedetomidine and digoxin.26 Use during Mechanical Ventilation in peadiatrics: In 2004, a prospective randomized open-label trial comparing midazolam and dexmedetomidine in children requiring mechanical ventilation.27 Thirty children were randomized to either midazolam, with a 0.1 mg/kg IV loading dose followed by 0.1 mg/kg/hr, or dexmedetomidine small-dose (0.25 mcg/kg IV followed by an infusion of 0.25 mcg/kg/hr) or large-dose (0.5 mcg/kg IV followed by an infusion of 0.5 mcg/kg/hr). Three sedation scoring tools, the Ramsay score, a pediatric intensive care unit (PICU) sedation score, and a score assessing response to tracheal suctioning, were used to evaluate the patients, as well as Bispectral Index Monitor (BIS). The BIS score represents a processed electroencephalogram (EEG) measurement ranging from 0 (isoelectric EEG) to 100 (fully awake). No differences were noted in sedation scores or BIS scores among the groups. Mean BIS numbers were 57 ± 8 for the midazolam group, 51 ± 12 for the small-dose dexmedetomidine group, and 60 ± 10 for the largedose dexmedetomidine group. The children in the large-dose dexmedetomidine group required significantly fewer supplemental morphine doses than the children given midazolam and had a Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9879 REVIEW ARTICLE lower total morphine dose. The number of inadequately sedated children was also lower in the two dexmedetomidine groups than in the midazolam group. Based on their results, the authors suggest that dexmedetomidine at a dose of 0.25 mcg/kg/hr was approximately equivalent to midazolam given at a rate of 0.22 mg/kg/hr, and that a higher infusion rate (0.5 mcg/kg/hr) may be more effective. Another early retrospective study described the use of dexmedetomidine in 65 pediatric patients (mean age 5 years) with burns.28 The infusion was initiated at 0.2 mcg/kg/hr and titrated to an average dose of 0.5 mcg/kg/hr. Twenty-six patients received an IV loading dose of 1 mcg/kg. All patients were considered adequately sedated, based on clinical impression, even those who had previously failed treatment with opioids and benzodiazepines. Similar efficacy rates were reported from a retrospective study of 38 children given dexmedetomidine after cardiac or thoracic surgery.29After an initial dose of 0.32 ± 0.15 mcg/kg/hr, patients were titrated to a mean dose of 0.3 ± 0.05 mcg/kg/hr. There was a trend towards larger dose requirements in patients less than 1 year of age, with a mean of 0.4 ± 0.13 mcg/kg/hr compared to 0.29 ± 0.17 mcg/kg/hr in older children (p=0.06). The desired level of sedation was achieved in 93% of patients; analgesia was adequate in 83%. Six patients (15%) had hypotension; three patients responded to dose reduction and three cases resolved with discontinuation. One patient developed bradycardia. These early studies prompted many institutions to consider a role for dexmedetomidine in their pediatric patients requiring mechanical ventilation. Dexmedetomidine may have a unique role in the sedation of children with neurologic impairment who require mechanical ventilation. It is often difficult to achieve adequate sedation in these patients, and the use of large-dose therapies may increase the risk of adverse effects. Benzodiazepines, among the most common sedatives used in pediatric patients, may produce paradoxical agitation or hypotension. The benefits of dexmedetomidine in these patients has been suggested in several papers, beginning with a case series of 5 children with trisomy 21 published in 2007.30 The patients ranged from 2 months to 3 years of age, and all were receiving mechanical ventilation after cardiac surgery. Dexmedetomidine, administered at infusion rates of 0.2 to 2.5 mcg/kg/hr,provided adequate sedation even after discontinuation of fentanyl and midazolam. Therapy was generally well tolerated, with only one patient experiencing transient hypotension and bradycardia with an infusion rate of 0.7 mcg/kg/hr. None of the patients experienced paradoxical agitation and all were successfully extubated on therapy. In 2008, a prospective observational study described dexmedetomidine use in 17 infants and children (ages 1 month to 17 years) requiring mechanical ventilation, including ten children with neurologic impairment. 25Twenty treatment courses were evaluated. In 15 cases, dexmedetomidine was initiated to minimize the use of midazolam prior to extubation. In the remaining cases, it was chosen as an alternative sedative in patients unable to tolerate midazolam. The average dose at initiation was 0.2 ± 0.2 mcg/kg/hr; no loading doses were given. The maximum dose was 0.5 ± 0.2 mcg/kg/hr, with an average duration of therapy of 32 hours.. Mean arterial pressures and heart rate were not significantly different before and 1 hour after starting therapy. These values were also assessed at discontinuation and 12 hours later to assess for withdrawal or rebound hypertension, but no differences were observed. One patient developed transient hypotension during the study. None of the patients, including those with neurologic impairments, developed paradoxical agitation. There were no cases of withdrawal. The authors concluded that careful patient selection and a Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9880 REVIEW ARTICLE conservative approach to dosing resulted in successful introduction of dexmedetomidine into their PICU. Three additional retrospective studies were published in 2009.31-33 The first compared dexmedetomidine to standard analgesic/sedative combinations in 14 children after Fontan surgery.31 The patients, all between 14 months and 11 years, received either dexmedetomidine (0.1– 1 mcg/kg/hr) or standard therapy with a combination of midazolam, propofol, buprenorphine, and/or pentazocine. Doses were adjusted to maintain target pediatric sedation scores. The five children who received standard therapy developed respiratory depression, while the nine patients given dexmedetomidine had no evidence of respiratory depression (defined as a PaCO2> 42 mm Hg). All of the patients had cardiac pacing wires in place throughout the study, set to activate at a heart rate less than 90 bpm. Six of the nine children given dexmedetomidine developed bradycardia and were paced, compared to none in the standard treatment group. Duration of mechanical ventilation and length of stay were not significantly different between the groups. No withdrawal or rebound was observed in the dexmedetomidine group. The authors concluded that the lack of respiratory depression with dexmedetomidine may decrease the risk for elevated pulmonary vascular resistance and improve cardiac function, making it a useful option for sedation after Fontan surgery. In the largest retrospective study to date, the records of 121 children (2 months to 21 years) who received dexmedetomidine while undergoing mechanical ventilation were evaluated.32 The average effective dose was 0.55 mcg/kg/hr, with a range of 0.15 to 0.7 mcg/kg/hr. Therapy was adjusted based on COMFORT scores, a system incorporating signs and symptoms of both pain and agitation. Dexmedetomidine was the sole sedative in 18 patients. The remaining patients received combination therapy with opiates and/or benzodiazepines. The addition of dexmedetomidine resulted in a dose reduction of 42% and 36% in the patients treated with benzodiazepines and opiates, respectively. The average length of therapy was 25.8 hours, with a range of 20 minutes to 60 hours. Hypotension and/or bradycardia requiring intervention occurred in 27% of patients. In 10%, adverse effects led to the discontinuation of the drug. The authors concluded that the use of dexmedetomidine allowed reductions in the doses of opiates and benzodiazepines for most patients, but that close hemodynamic monitoring was necessary to identify adverse effects. In a retrospective study of patients who received dexmedetomidine for sedation in the pediatric intensive care unit, adverse events were assessed with the Naranjo scale to determine the likelihood of association with dexmedetomidine. 33One hundred and forty-four patients (median age 34 months, range 0 – 17.7 years) who underwent a total of 153 treatment courses were included. The mean infusion rate of dexmedetomidine was 0.42 μg/kg per hour (standard deviation 0.17 μg/kg per hour, range 0.05–2 μg/kg per hour). The median duration of therapy was 20.50 h (range 0.75–854.75 h), and 70 infusions (46%) lasted more than 24 h. At least one adverse event was observed in 115 (75%) of the treatment courses. Hypotension (81 [53%]) and bradycardia (38 [25%]) were the most common adverse events and were deemed “probably” attributable to dexmedetomidine in 17 (11%) and 9 (6%) of the treatment courses, respectively.33 But as with all other sedative/analgesic agents, close monitoring is vital to minimize adverse effects. DOSING AND ADMINISTRATION: Based on the reports available to date, the recommended adult dosage range of 0.2 to 0.7 mcg/kg/hr may also be used in children.25Dexmedetomidine may be initiated with a loading dose of 1 mcg/kg given over 10 minutes, but some pediatric centers reduce Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9881 REVIEW ARTICLE or omit the loading dose in an effort to avoid bradycardia and hypotension. The infusion should be titrated to patient response, with a suggested maximum dose of 2 mcg/kg/hr. WITHDRAWAL: Although not well studied, abrupt cessation of dexmedetomidine may produce withdrawal symptoms similar to those seen with clonidine withdrawal, including agitation, irritability, headache, and rebound hypertension. In clinical practice, infusions have often been continued for longer than 24 hours without adverse effects.³³ Additional experience comes from the series of 65 children given dexmedetomidine during mechanical ventilation after burn injury.28There were no reports of withdrawal or rebound, despite an average duration of 11 days and a range of 2 to 50 days. Conversely, a case report from 2007 describes tachycardia, hypertension, and emesis after abrupt discontinuation of a dexmedetomidine infusion in a 2-year-old boy.34 He had been treated for 6 days following a Glenn procedure, with dexmedetomidine doses ranging from 0.3 to 0.8 mcg/kg/hr. Reinstitution of therapy, with subsequent weaning by 0.1 mcg/kg/hr every 8 hours, resulted in resolution of all symptoms Dexmedetomidine Use in adult Intensive Care: Benzodiazepines, propofol are commonly used for sedation in ICU, along with the newly introduced DEX. Many studies have compared themwith DEX for sedation, length of stay in ICU, time for extubation, additive analgesia anddelirium. Comparision with Midazolam: In eclampsia patients DEX significantly reduced LOS in ICU (45.5 hours vs. 83 hours), duration from stop of drug to discharge from ICU (21 hours vs. 52 hours), and requirement of antihypertensive drug (less than 50%) with decreased heart rate and mean arterial pressure in 24 hours, when compared to midazolam.35 Dexmedetomidine patients in the SEDCOM studyhad decreased duration of mechanical ventilation and less tachycardia and hypertension.17The Safety and Efficacy of Dexmedetomidine Compared with Midazolam (SEDCOM) study presents that DEX was associated with shorter median time to extubation by 1.9 days (3.7 days vs. 5.6 days; P = 0.01) compared to midazolam, but LOS in ICU (5.9 days vs. 7.6 days; P = 0.24) and time within target Richmond Agitation-Sedation Scale [RASS] score range (77.3% vs. 75.1%; P = 0.18) was similar between 2 drugs.36 Comparision with Lorazepam: In mechanically ventilated ICU patients managed with individualized targeted sedation, use of a dexmedetomidine infusion resulted in more days alive without delirium or coma and more time at the targeted level of sedation than with a lorazepam infusion.37The Maximizing Efficacy of Targeted Sedation and Reducing Neurological Dysfunction (MENDS) study resulted in better sedative efficacy (RASS within 1 point of goal 80% vs. 67%; P = 0.04) with less likelihood of oversedation (15% vs. 33%) in the DEX group than in the lorazepam group. Benzodiazepines have been used for sedation for many years within the ICU setting with midazolam, lorazepam, and diazepam being the most commonly utilized agents. They are GABA agonists metabolized in the liver to active metabolites (lorazepam being the exception with no active metabolite). These metabolites can lead to prolongation of their sedative effects, especially in the presence of renal failure. The use of lorazepam is limited by the fact it is dissolved in propylene glycol, which can accumulate to produce metabolic acidosis and renal dysfunction.38 Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9882 REVIEW ARTICLE Comparision with Propofol: In a recently published study, dexmedetomidine was compared to midazolam (MIDEX) and propofol (PRODEX) for light to moderate sedation in patients requiring mechanical ventilation for greater than 24 hours.39 Time at target arousal level was equivalent between dexmedetomidine and the control groups; however, more patients in the dexmedetomidine group required rescue drug than in the propofol group, and discontinuation due to lack of efficacy occurred more often in patients sedated with dexmedetomidine than in patients sedated with midazolam or propofol. Arousability, communication, and patient cooperation were improved with dexmedetomidine sedation. Dexmedetomidine reduced duration of mechanical ventilation compared with midazolam, and time to extubation was faster in the dexmedetomidine groups than either the midazolam or propofol groups. Overall, length of ICU and hospital stay and mortality were similar between groups. In a study that evaluated sedative efficacy of DEX compared to standard therapy with propofol or midazolam, both drugs showed similar adequacy to light to moderate sedation (RASS 0 to -3). However, sedation by DEX was unreliable when deeper sedation (RASS score of -4 or less) is targeted (time at target RASS 42% vs. 62%; P = 0.06).40 Dexmedetomidine provided safe and effective sedation for post-CABG surgical patients and significantly reduced the use of analgesics, beta-blockers, antiemetics, epinephrine, and diuretics. Mean sedation levels were within target ranges in both groups. Mean times to weaning and extubation were similar, although fewer dexmedetomidine patients remained on the ventilator beyond 8 hours. Morphine use was significantly reduced in the dexmedetomidine group41A study comparing dexmedetomidine and propofol sedation in post-surgical patients showed similar efficacy at target sedation, but patients sedated with dexmedetomidine required less supplemental analgesia.42For ICU patient sedation, dexmedetomidine may offer advantages over propofol in terms of decrease in the length of ICU stay and the risk of delirium.43DEX provided adequate sedation comparable to propofol for postoperative ventilator care of patients with extensive cervical spinal operation.44 Collectively, though data are not identical with each other, DEX produces better or at least, similar sedative adequacy compared to traditional agents and has potential to decrease the duration of ventilatory care and LOS in ICU. However, in the case of a required deep level of sedation around a RASS score -4, DEX might be an inappropriate option, so other agents or use with additive drugs should be considered. Withdrawal: Most of studies reported no withdrawal symptoms even following abrupt discontinuation of DEX, but still there was a small possibility of developing agitation, headache, hyperhidrosis, hypertension, tremor, nausea, vomiting in minor population, so a progressive tapering is considered safe.36 Delirium in ICU: Delirium is characterized by a disturbance of consciousness with accompanying change in cognition. Delirium is an acute neuropsychiatric syndrome of attentional deficit, disorganized thought, cognitive dysfunction with fluctuating course and it is reported to affect up to 80% of patients in ICU.12 Delirium is extremely common in the intensive care unit (ICU) especially amongst mechanically ventilated patients. Delirium is now designated for the strongest independent Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9883 REVIEW ARTICLE predictor of mortality, duration of ventilatory care, LOS in ICU, and total duration of hospital admission.36, 45, 46 The causes that develop or precipitate delirium include sedative agents used in ICU.46The GABAergic agents cause cognitive impairment through direct effect on memory formation and modulation, or indirect sleep disturbance.47The normal process of memory involves both slow wave sleep (stage 3, 4 of NREM sleep) and REM sleep.BDZ alters sleep architecture and depresses slow wave sleep. On the contrary, DEX has little effect on direct memory impairment, and preserves slow wave sleep.6Thus,it has less influence on cognitive dysfunction. This character is accompanied by arousability, facilitates cooperative assessment for delirium and would be advantageous to prevention and diagnosis of delirium. There is the clinical evidence for DEX's effect on prevention of delirium. SEDCOM study showed lower prevalence of delirium in the DEX group than in the midazolam group (54% vs. 76.6%; P < 0.001).36 MENDS study measured the number of days alive without delirium or coma, presenting a higher value in the DEX group (7.0 days vs. 3.0 days; P = 0.01) and lower prevalence of coma as well (63% vs. 92%; P < 0.001) than in the lorazepam group.[37] These results show that DEX is superior to BDZ in prevention of delirium or coma. However, the effect of DEX on delirium, in spite of its favorable pharmacologic distinction with clinical evidence, has not been proven to be significantly different from traditional sedatives in a meta-analysis that included 2, 419 patients that participated in 24 trials48 This does not mean that DEX has no benefit, considering limitations of significant heterogeneity and inconsistent measurement of delirium between the pooled studies. DEX seems to have a therapeutic potential on delirium, as well as on prevention. There is an interesting preliminary trial, though it is limited by small sample size, in which 20 patients who could not be weaned from a ventilator because of agitated delirium were treated with DEX or haloperidol.49 Results showed that the DEX group had a markedly shorter time to extubation (19.9 hours vs. 42.5 hours; P = 0.016) and ICU LOS (1.5 days vs. 6.5 days; P = 0.004) as well. Because the duration of ventilatory support and ICU stay are definitely related to a reduction in delirium, particularly in this trial, results reflect the influence of DEX on delirium directly. Pharmacodynamics, Pharmacokinetics, adverse effects and safety: Dexmedetomidine, an imidazole compound, is the pharmacologically active dextroisomer of medetomidine that displays specific and selective α2-adrenoceptor agonism. The mechanism of action is unique and differs from those of currently used sedative agents, including clonidine. Activation of the receptors in the brain and spinal cord inhibits neuronal firing, causing hypotension, bradycardia, sedation, and analgesia. The responses to activation of the receptors in other areas include decreased salivation, decreased secretion, and decreased bowel motility in the gastrointestinal tract; contraction of vascular and other smooth muscle; inhibition of renin release, increased glomerular filtration, and increased secretion of sodium and water in the kidney; decreased intraocular pressure; and decreased insulin release from the pancreas 50 The administration of a bolus of 1 μg/kg dexmedetomidine initially results in a transient increase of the blood pressure and a reflex decrease in heart rate, especially in younger, healthy patients.51The initial reaction can be explained by the peripheral α2B-adrenoceptor stimulation of vascular smooth muscle and can be attenuated by a slow infusion over 10 or more minutes. Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9884 REVIEW ARTICLE Dexmedetomidine could result in cardiovascular depression, i.e., bradycardia and hypotension. The incidence of postoperative bradycardia has been reported as high as 40% in healthy surgical patients who received dexmedetomidine, especially high doses.52Usually, these temporary effects were successfully treated with atropine or ephedrine and volume infusions. There are, of course, clinical situations in which the sympatholytic or bradycardic actions of α 2adrenoceptor agonists may be deleterious (e.g., in hypovolemic patients or patients with fixed stroke volume). Most studies consistently pointed out bradycardia as the only adverse effect of DEX. Actually, DEX does not increase the risk of bradycardia in general, butfound only in cases in which both a loading dose and high maintenance dose (> 0.7 µg/kg/h) are administrated, and furthermore, it does not seem to be associated with increased risk of significant hypotension requiring treatment.48 Even if bradycardia has developed, it is reversed with relatively simple intervention, such as by decreasing the dose.36 Dexmedetomidine has no significant effect on adrenocorticotropic hormone (ACTH) secretion at therapeutic doses, cortisol's response to ACTH may be reduced after prolonged use or high doses of dexmedetomidine.53coadministration of dexmedetomidine with anesthetic agents, sedatives, hypnotics, or opioids is likely to cause additive effects.54 The recommended dose for sedation in ICU,is a loading dose of 1 µg/kg over 10 minutes followed by continuous infusion of 0.2-0.7 µg/kg/h (< 24 h). However, several trials have used a higher dose up to 1.5 µg/kg/h over 24 hours, without clinically significant problems.36, 37.49, 55However, there still is a long way to go to extend all the benefits of DEX to the general population of critically ill patients. Several studies have limitations of that exclude many disease groups neurologic disease, acute MI, heart block, trauma, burn injury, serious CNS pathology, severe liver disease, pregnancy - from clinical trials or small sample size or being unblended.55 Dexmedetomidine undergoes almost complete biotransformation through direct glucuronidation and cytochrome P450 metabolism (hydroxylation, mediated by CYP2A6), all hepatic processes, with very little excretion of unchanged molecules in the urine or feces. Although dexmedetomidine is dosed to effect, it may be necessary to decrease the typical dose in patients with hepatic failure, since they will have lower rates of metabolism of the active drug. Metabolites of biotransformation are excreted in the urine (about 95%) and in the feces (4%). It is unknown whether they possess intrinsic activity. The elimination half-life is approximately 2 hours.56 DEX has an onset of action approximately in 15 minutes after intravenous injection, and reaches its peak concentration after 1 hour of continuous infusion. Dexmedetomidine exhibits linear kinetics when infused in the recommended dose range of 0.2 to 0.7 μg/kg/hr for no more than 24 hours. The steady-state volume of distribution is 118 L, and the distribution phase is rapid, with a half-life of distribution of approximately 6 minutes.56 The average protein binding of dexmedetomidine is 94%, with negligible protein binding displacement by fentanyl, ketorolac, theophylline, digoxin, and lidocaine, all drugs commonly used during anesthesia and in the ICU.56 There have been no significant sexor age based differences in the pharmocokinetic profile, even in elderly patients, and pharmacokinetics of the active dexmedetomidine molecule do not change in patients with renal failure.56 CONCLUSION: Conscious sedation combined with analgesic property of DEX make it a unique drug of choice for adult ICU sedation. DEX preserves a natural sleep pattern and induces cooperative Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9885 REVIEW ARTICLE sedation in which patients are easily arousable, leads to less impairment in cognitive function, and has an opioid sparing effect as well. DEX decreases duration of ventilatory care, ICU stay, prevalence, and duration of delirium with better adequacy of sedation, and therefore improvement in outcomes. DEX appears to be an alternative to benzodiazepines and propofol for adult patients. Dexmedetomidine offers an additional choice for the sedation of children receiving mechanical ventilation in the intensive care setting. Its benefits include limited effects on respiratory drive, a relatively short half-life, no significant drug interactions, and a generally mild adverse effect profile. It may be particularly useful in children with underlying neurologic disorders, who often develop agitation or adverse hemodynamic and respiratory effects with opioids or benzodiazepines. additional studies are needed to define the role of dexmedetomidine in pediatric intensive care. REFERENCES: 1. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30(1):119–41. 2. Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry. 2004;161(1):45–52. 3. Kollef MH, Levy NT, Ahrens TS, Schaiff R, Prentice D, Sherman G. The use of continuous i.v. sedation is associated with prolongation of mechanical ventilation. Chest. 1998;114(2):541– 48. 4. Pandharipande P, Shintani A, Peterson J, Pun BT, Wilkinson GR, Dittus RS, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006;104(1):21–26. 5. Watson PL, Shintani AK, Tyson R, Pandharipande PP, Pun BT, Ely EW. Presence of electroencephalogram burst suppression in sedated, critically ill patients is associated with increased mortality.). Crit Care Med. 2008;36(12):3171-7. 6. Huupponen E, Maksimow A, Lapinlampi P, Särkelä M, Saastamoinen A, Snapir A et al. ActaAnaesthesiol Scand. Electroencephalogram spindle activity during dexmedetomidinesedation and physiological sleep 2008;52(2):289-94. Epub 2007 Nov14. 7. Venn RM, Hell J, Grounds RM. Respiratory effects of dexmedetomidine in the surgical patient requiring intensive care. Crit Care. 2000;14:302–308. doi: 10.1186/cc712. 8. Berkowitz DE, Price DT, Bello EA, Page SO, Schwinn DA. Localization of messenger RNA for three distinct alpha 2-adrenergic receptor subtypes in human tissues. Evidence for species heterogeneity and implications for human pharmacology. Anesthesiology. 1994;81:1235–44. 9. Panzer O, Moitra V, Sladen RN. Pharmacology of sedative-analgesic agents: dexmedetomidine, remifentanil, ketamine, volatile anesthetics, and the role of peripheral Mu antagonists. AnesthesiolClin. 2011;29:587–605. 10. Abuhasna S, Al Jundi A, Abdelatty W, Urrahman M. Evaluation of long-term infusion of dexmedetomidine in critically ill patients: A retrospective analysis. Int J CritIllnInj Sci. 2012;2(2):70-4. doi: 10.4103/2229-5151.97270. 11. Mantz J, Josserand J, Hamada S. Dexmedetomidine: new insights. Eur J Anaesthesiol. 2011;28:3–6. Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9886 REVIEW ARTICLE 12. Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119–41. 13. Correa-Sales C, Rabin BC, Maze M. A hypnotic response to dexmedetomidine, an alpha 2 agonist, is mediated in the locus coeruleus in rats. Anesthesiology. 1992;76:948–52. 14. Samuels ER, Szabadi E. Functional neuroanatomy of the noradrenergic locus coeruleus: its roles in the regulation of arousal and autonomic function part I: principles of functional organisation. CurrNeuropharmacol. 2008;6:235–53 15. Fairbanks CA, Wilcox GL. Spinal antinociceptive synergism between morphine and clonidine persist in mice made acutly or chronically tolerant to morphine. J PharmacolExpTher 1999;288:1107-16. 16. Petroz GC, Sikich N, James M. Van Dyk H Shafer SL, Schily M. etal.A phase I, two-center study of the pharmacokinetics and pharmacodynamics of dexmedetomidine in children. Anesthesiology. 2006;105:1098–110. 17. Diaz SM, Rodarte A, Foley J. CapparelliEV.Pharmacokinetics of dexmedetomidine in postsurgical pediatric intensive care unit patients: preliminary study. PediatrCrit Care Med. 2007;8:419–24. 18. Vilo S, Rautiainen P, Kaisti K.Aantaa R, Scheinin M, Manner T, et al Pharmacokinetics of intravenous dexmedetomidine in children under 11 years of age. Br J Anaesth. 2008;100:697– 00. 19. Potts AL, Warman GR, Anderson BJ. Dexmedetomidine disposition in children: a population analysis. PaediatrAnaesth. 2008;18:722–30. 20. Potts AL, Anderson BJ, Warman GR. Lerman J, Diaz SM, Vilo S. Dexmedetomidine pharmacokinetics in pediatric intensive care - a pooled analysis. PaediatrAnaesth. 2009;19:1119–29. 21. Hammer GB, Drover DR, Cao H. Jackson E, Williams GD, Ramamoorthy C. etalThe effects of dexmedetomidine on cardiac electrophysiology in children. AnesthAnalg. 2008;106:79–83. 22. Mason KP, Zurakowski D, Zgleszewski SE Robson CD, Carrier M, Hickey PR, et al. High dose dexmedetomidine as the sole sedative for pediatric MRI. PaediatrAnaesth. 2008;18:403–11. 23. Mason KP, Zgleszewski S, Forman RE. An exaggerated hypertensive response to glycopyrrolate therapy for bradycardia associated with high-dose dexmedetomidine. AnesthAnalg. 2009;108:906–08. 24. Erkonen G, Lamb F, Tobias JD. Stark C, DiNardo JA. High-dose dexmedetomidine-induced hypertension in a child with traumatic brain injury. Neurocrit Care. 2008;9:366–369. 25. Buck ML, Willson DF. Use of dexmedetomidine in the pediatric intensive care unit. Pharmacotherapy. 2008;28:51–57. 26. Berkenbosch JW, Tobias JD. Development of bradycardia during sedation with dexmedetomidine in an infant concurrently receiving digoxin. PediatrCrit Care Med. 2003;4:203–05. 27. Tobias JD, Berkenbosch JW. Sedation during mechanical ventilation in infants and children: dexmedetomidine versus midazolam. South Med J. 2004;97:451–55. 28. Walker J, MacCallum M, Fischer C, Kopcha R, Saylors R, McCall J.Sedation using dexmedetomidine in pediatric burn patients. J Burn Care Res. 2006;27:206–10. Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9887 REVIEW ARTICLE 29. Chrysostomou C, Di Filippo S, Manrique A. Schmitt CG, Orr RA, Casta A.et al Use of dexmedetomidine in children after cardiac and thoracic surgery. PediatrCrit Care Med. 2006;7:126–31. 30. Kalyanaraman M, Costello JL, Starr JP. Use of dexmedetomidine in patients with trisomy 21 after cardiac surgery. PediatrCardiol. 2007;28:396–99. 31. Tokuhira N, Atagi K, Shimaoka H, Ujiro A, Otsuka Y, Ramsay M.Dexmedetomidine sedation for pediatric post-Fontan procedure patients. PediatrCrit Care Med. 2009;10:207–12. 32. Czaja AS, Zimmerman JJ. The use of dexmedetomidine in critically ill children. PediatrCrit Care Med. 2009;10:381–86. 33. Carney L, Kendrick J, Carr R. safety and effectiveness of dexmedetomidine in paediatric intensive care unit (SAD-PICU) Can J hospparm 2013;66(1)21-27. 34. Weber MD, Thammasitboon S, Rosen DA. Acute discontinuation syndrome from dexmedetomidine after protracted use in a pediatric patient. PaediatrAnaesth. 2007;18:87–88. 35. Esmaoglu A, Ulgey A, Akin A, Boyaci A. Comparison between dexmedetomidine and midazolam for sedation of eclampsia patients in the intensive care unit. J Crit Care. 2009;24:551–55. 36. Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidinevs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301:489–99. 37. Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidinevslorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007;298:2644–53. 38. Yahwak JA, Riker RR, Fraser GL, Subak-Sharpe S. Determination of a lorazepam dose threshold for using the osmol gap to monitor for propylene glycol toxicity. Pharmacotherapy. 2008;28(8):984–91. 39. Jakob SM, Rukonen E, Grounds R, Sarapohja T, Garratt C, Pocock SJet al..Dexmedetomidinevs midazolam or propofol for sedation during prolonged mechanical ventilation;two randomized controlled trails.JAMA 2012;307(11)1151-60. 40. Ruokonen E, Parviainen I, Jakob SM, Nunes S, Kaukonen M, Shepherd ST, et al. Dexmedetomidine versus propofol/midazolam for long-term sedation during mechanical ventilation. Intensive Care Med. 2009;35:282–90. 41. Herr DL, Sum-Ping ST, England M. ICU sedation after coronary artery bypass graft surgery: dexmedetomidine-based versus propofol-based sedation regimens.jcardiothoracVascAnesth. 2003;17(5):576-84. 42. Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth. 2001;87(5):684–90. 43. Xia ZQ, Chen SQ, Yao X, Xie CB, Wen SH, Liu KX Clinical benefits of dexmedetomidine versus propofol in adult intensive care unit patients: a meta-analysis of randomized clinical trials. J Surg Res. 2013; Jul 24. pii: S0022-4804(13)00685-9. doi: 10.1016/j.jss.2013.06.062. [Epub ahead of print]. 44. Terao Y, Ichinomiya T, Higashijima U, Tanise T, Miura K, Fukusaki M, et al. Comparison between propofol and dexmedetomidine in postoperative sedation after extensive cervical spine surgery. J Anesth. 2012;26:179–86. Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9888 REVIEW ARTICLE 45. Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–62. 46. Frontera JA. Delirium and sedation in the ICU. Neurocrit Care. 2011;14:463–74. 47. Sanders RD, Maze M. Contribution of sedative-hypnotic agents to delirium via modulation of the sleep pathway. Can J Anaesth. 2011;58:149–56. 48. Tan JA, Ho KM. Use of dexmedetomidine as a sedative and analgesic agent in critically ill adult patients: a meta-analysis. Intensive Care Med. 2010;36:926–39. 49. Reade MC, O'Sullivan K, Bates S, Goldsmith D, Ainslie WR, Bellomo R. Dexmedetomidine vs. haloperidol in delirious, agitated, intubated patients: a randomised open-label trial. Crit Care. 2009;13(3):R75. 50. Metz SA, Halter JB, Robertson RP. Induction of defective insulin secretion and impaired glucose tolerance by clonidine. Selective stimulation of metabolic alpha-adrenergic pathways. Diabetes. 1978;27:554–62. 51. Bloor BC, Ward DS, Belleville JP, Maze M. Effects of intravenous dexmedetomidine in humans. II. Hemodynamic changes. Anesthesiology. 1992;77:1134–42. 52. Aho M, Erkola O, Kallio A, Scheinin H, Korttila K. Comparison of dexmedetomidine and midazolam sedation and antagonism of dexmedetomidine with atipamezole. J ClinAnesth. 1993;5:194–203. 53. Maze M, Virtanen R, Daunt D, Banks SJ, Stover EP, Feldman D. Effects of dexmedetomidine, a novel imidazole sedative-anesthetic agent, on adrenal steroidogenesis: in vivo and in vitro studies. AnesthAnalg. 1991;73:204–08. 54. Aantaa R, Kanto J, Scheinin M, Kallio A, Scheinin H. Dexmedetomidine, an alpha 2-adrenoceptor agonist, reduces anesthetic requirements for patients undergoing minor gynecologic surgery. Anesthesiology. 1990;73:230–35. 55. Guinter JR, Kristeller JL. Prolonged infusions of dexmedetomidine in critically ill patients. Am J Health Syst Pharm. 2010;67:1246–53. 56. Gertler R, Brown HC, Mitchell DH, Silvius EN.Dexmedetomidine: a novel sedative-analgesic agent.Proc (BaylUniv Med Cent). 2001; 14(1): 13–21. AUTHORS: 1. Sahana K.S. 2. Sunil B.V. PARTICULARS OF CONTRIBUTORS: 1. Assistant Professor, Department of Paediatrics, Srinivas Institue of Medical Sciences and Research Center, Mukka, Surathkal, India. 2. Associate Professor, Department of Anaesthesia, Srinivas Institue of Medical Sciences and Research Center, Mukka, Surathkal, India. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr.Sahana K.S., C/O. SatishRao, #12, 2A Cross, Basavasamithi Layout, Vidyaranyapura, Bangalore – 97. Email-dr.sahana2003@yahoo.co.in Date of Submission: 02/12/2013. Date of Peer Review: 03/12/2013. Date of Acceptance: 13/12/2013. Date of Publishing: 17/12/2013 Journal of Evolution of Medical and Dental Sciences/Volume 2/Issue 51/ December 23, 2013 Page 9889