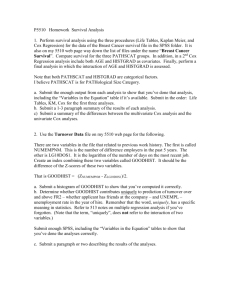
Technical Appendix Statistical method As described in the main text
advertisement

Technical Appendix Statistical method As described in the main text, we used a three-step approach to estimate the effect of CR on survival, while controlling for potential confounders. In this appendix, we describe each of these steps in further detail. In the first step, we fitted a penalized Cox proportionalhazards regression model, estimating days of survival conditional on treatment status (CR / no CR) and confounders. We used the lasso1, an automated variable selection method to shrink the full set of variables in category f (i.e., variables without a specific a priori expectation on their status as a confounder) to a much smaller set with maximal predictive power with respect to the outcome of interest (survival). The lasso can be understood as a regression model, in which the sum of the absolute values of the regression coefficients is less than a constant. Its aim is similar to traditional automated variable selection methods, such as subset selection (e.g., forward stepwise), but improves on these methods by yielding more stable models, and greater predictive accuracy1. The constraint on the absolute values of the regression coefficients is a tuning factor, which regulates the amount of shrinkage, with lower values leading to more parsimonious models, i.e. models in which many coefficients are zero. In our analysis, we fitted the lasso regression model 1000 times, over a range of increasing values of this constraint. We used (10-fold) cross-validation, to choose the optimal constraint based on a cross-validated partial-likelihood criterion, as proposed by Van Houwelingen et al.2 and implemented in the glmnet package3 4 of the R statistical software version 2.15.25. This step ensured that confounders included in our final model were indeed independently related to the outcome (rather than being only related to treatment), which has been shown of importance to minimize bias in the treatment effect6 7.In the second step we estimated the propensity score, i.e. the probability of receiving CR as a function of all confounders selected in the first step, using generalised boosted regression8 9. We subsequently estimated the average treatment effect on the treated (ATT) by weighting all observations for patients who did not receive CR, by the inverse of the propensity score. After propensity score weighting, it was checked whether all confounders were equally distributed across both groups. In the third step, we estimated the effect of CR on survival using a traditional Cox proportional hazards model in this weighted cohort, including the treatment indicator and all covariates (commonly referred to as a "doubly-robust" approach10 11 12. We tested the assumption of proportional hazards over time, and report estimates for three different followup times (12, 24 and 48 months after study inclusion). Results We used a total of 919 potential confounders. Besides the 26 confounders listed in Table 1 of the main text, for which we had an a priori expectation of their association with survival, we identified an additional set of 892 other characteristics that were associated with survival in our dataset. These included diagnoses related to a hospital visit or discharge (160 variables), hospital treatments (82), outpatient prescriptions at 5-digit ATC chemical subgroup level (154) and other medical services and products (496), all measured during the 12 month period before study inclusion. Because we included all confounders both as 0/1 indicators, as actual quantities (e.g. the volume of a prescription), and as aggregated variables (e.g. prescriptions at the 3-digit therapeutic subgroup level), the total number of variables was 2718. From this initial set of variables, 99 remained after applying Cox proportional hazards regression to predict survival, using the lasso and 10-fold cross-validation. 1 Tibshirani R. Regression Shrinkage and Selection via the Lasso." Journal of the Royal Statistical Society B; 1996(58): 267-288.. 2 van Houwelingen HC, Bruinsma T, Hart AAM, van't Veer LJ, Wessels LFA. Cross- Validated Cox Regression on Microarray Gene Expression Data. Statistics in Medicine, 2006 Sep 30;25(18):3201-16.. 3 Friedman J, Hastie T, Tibshirani R. Regularization Paths for Generalized Linear Models via Coordinate Descent. Journal of Statistical Software 2010; 33(1): 4 Simon N, Friedman JH, Hastie T, Tibshirani R. Regularization Paths for Cox's Proportional Hazards Model via Coordinate Descent. Journal of Statistical Software 2011; 39(5) 5 R Core Team. R: A language and environment for statistical computing. http://www.R- project.org/. Vienna, Austria: R Foundation for Statistical Computing; 2012. 6 Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Sturmer T. Variable selection for propensity score models. Am J Epidemiol 2006; 163(12):1149-1156. 7 Patrick AR, Schneeweiss S, Brookhart MA, Glynn RJ, Rothman KJ, Avorn J et al. The implications of propensity score variable selection strategies in pharmacoepidemiology: an empirical illustration. Pharmacoepidemiol Drug Saf 2011; 20(6):551-559. 8 Friedman JH. Greedy function approximation: A gradient boosting machine. Annals of Statistics 2001; 29(5):1189-1232. 9 Friedman JH. Stochastic gradient boosting. Computational Statistics and Data Analysis 2002; 38(4):367-378. 10 Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med 2004; 23(19):29372960. 11 Austin PC. The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Stat Med 2010; 29(20):2137-2148. 12 Funk MJ, Westreich D, Wiesen C, Sturmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol 2011; 173(7):761-767.