RTC 101 Student Learning Outcomes (SLO) Assessment
advertisement
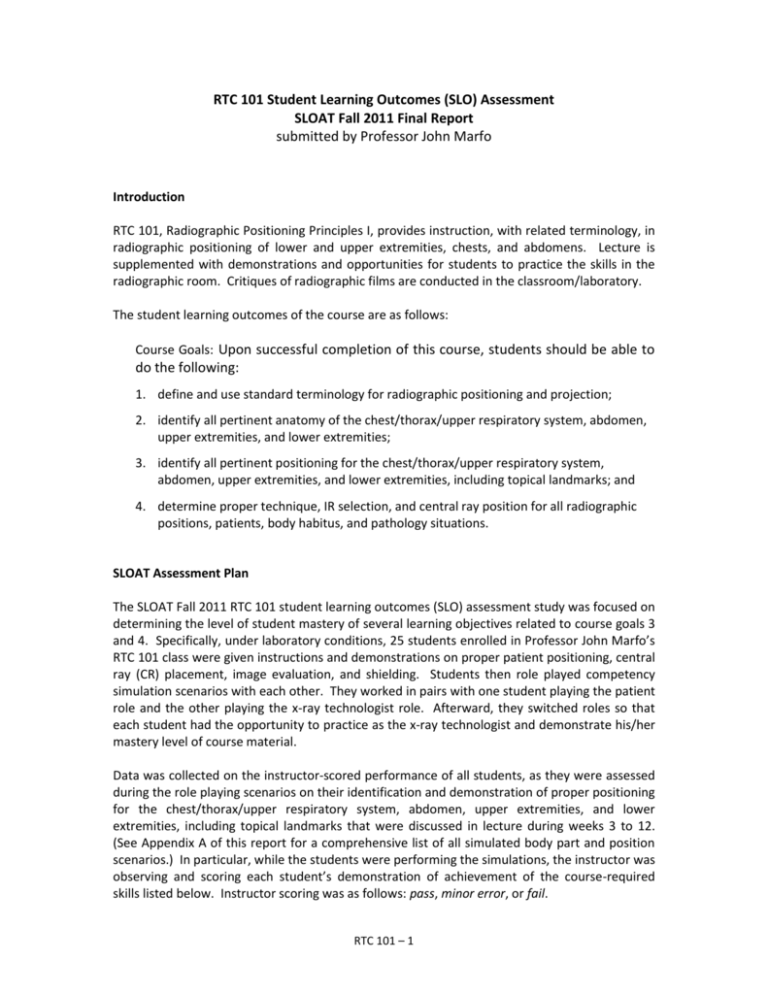
RTC 101 Student Learning Outcomes (SLO) Assessment SLOAT Fall 2011 Final Report submitted by Professor John Marfo Introduction RTC 101, Radiographic Positioning Principles I, provides instruction, with related terminology, in radiographic positioning of lower and upper extremities, chests, and abdomens. Lecture is supplemented with demonstrations and opportunities for students to practice the skills in the radiographic room. Critiques of radiographic films are conducted in the classroom/laboratory. The student learning outcomes of the course are as follows: Course Goals: Upon successful completion of this course, students should be able to do the following: 1. define and use standard terminology for radiographic positioning and projection; 2. identify all pertinent anatomy of the chest/thorax/upper respiratory system, abdomen, upper extremities, and lower extremities; 3. identify all pertinent positioning for the chest/thorax/upper respiratory system, abdomen, upper extremities, and lower extremities, including topical landmarks; and 4. determine proper technique, IR selection, and central ray position for all radiographic positions, patients, body habitus, and pathology situations. SLOAT Assessment Plan The SLOAT Fall 2011 RTC 101 student learning outcomes (SLO) assessment study was focused on determining the level of student mastery of several learning objectives related to course goals 3 and 4. Specifically, under laboratory conditions, 25 students enrolled in Professor John Marfo’s RTC 101 class were given instructions and demonstrations on proper patient positioning, central ray (CR) placement, image evaluation, and shielding. Students then role played competency simulation scenarios with each other. They worked in pairs with one student playing the patient role and the other playing the x-ray technologist role. Afterward, they switched roles so that each student had the opportunity to practice as the x-ray technologist and demonstrate his/her mastery level of course material. Data was collected on the instructor-scored performance of all students, as they were assessed during the role playing scenarios on their identification and demonstration of proper positioning for the chest/thorax/upper respiratory system, abdomen, upper extremities, and lower extremities, including topical landmarks that were discussed in lecture during weeks 3 to 12. (See Appendix A of this report for a comprehensive list of all simulated body part and position scenarios.) In particular, while the students were performing the simulations, the instructor was observing and scoring each student’s demonstration of achievement of the course-required skills listed below. Instructor scoring was as follows: pass, minor error, or fail. RTC 101 – 1 Preparation of the patient for the specific simulated procedure Collection of the patient’s history information Proper positioning of the patient for the specific simulated procedure Proper shielding of the patient for the specific simulated procedure Correct central ray (CR) placement (i.e., axial, vertical & horizontal) for the specific simulated procedure Identification of the correct topical landmarks for accurate CR placement for the specific simulated procedure Communication/demonstration of correct breathing instructions (if any) to the patient Assessment Study Findings & Recommendations During these simulation exercises, it was a very positive side effect to see that students who were not actively role playing, initiated discussions with their classmates pertaining to patient positioning, CR placement, shielding, and patient preparation. Therefore, all students in the class were actively engaged throughout the assessment activity. The instructor-scored results of student performance on the simulation exercises are presented in the table and depicted in the graph below. Simulation Exercise Assessment Activity SLO Rubric pass % minor error % fail % 24 96% 1 4% 0 0% 22 88% 3 12% 0 0% 23 92% 1 4% 1 4% 23 92% 2 8% 0 0% 23 92% 1 4% 1 4% Identification of the correct topical landmarks for accurate CR placement for the specific simulated procedure 23 92% 1 4% 1 4% Communication/demonstration of correct breathing instructions (if any) to the patient 25 100% 0 0% 0 0% Preparation of the patient for the specific simulated procedure Collection of the patient’s history information Proper positioning of the patient for the specific simulated procedure Proper shielding of the patient for the specific simulated procedure Correct central ray (CR) placement (i.e., axial, vertical & horizontal) for the specific simulated procedure RTC 101 – 2 100% 90% 80% 70% Pass 60% 50% Minor Error 40% Fail 30% 20% 10% 0% As can be seen from reviewing the table or graph above, the assessed RTC 101 students performed very well on this simulation exercise, which means they mastered many of the course learning objectives. Furthermore, it appears that the greatest challenge for the assessed students was collecting the patient’s history. This is most likely due to the fact that students were not very familiar with indication for radiographic procedure of specific body parts. Recommendations to improve student learning and teaching in RTC 101 are as follows: Encourage students to thoroughly determine patient history information before each radiographic examination. Emphasize the importance of becoming familiar with indication for radiographic procedures of various body parts. Perform more in-class demonstrations for students to observe and practice positioning, correct central ray (CR) placement (i.e., axial, vertical & horizontal), and identification of the relevant topical landmarks for accurate CR placement. RTC 101 – 3 Appendix A – RTC 101 Required Laboratory Competencies BODY PART Chest POSITION/S REQUIRED Routine (PA/LAT) Lordotic: Lindbloom and CR angle Stretcher and wheelchair AP and left lateral R & L decubitus and both obliques Pediatric Chest Abdomen Pediatric Abdomen Pediatric Soft Tissue Neck Wrist Radius and Ulna (Forearm) Elbow AP/ LAT supine and erect AP (KUB) and erect Dorsal decubitis and lateral decubitis AP supine, AP erect, and lateral Supine AP and left lateral PA, oblique, left lateral, ulna deviation, and carpal canal (Stecher view) AP and lateral Scapula AC Joint AP, lateral, and both obliques AP partial flexion (when elbow cannot be extended) Trauma axial lateral (Coyle view) AP and lateral Erect or recumbant AP neutral Transthoracic lateral AP, AP 15 – 30 degree cephalic, and PA 15 – 30 degree caudal AP internal, external, and neutral Posterior oblique (Grashey) and axial (Lawrence) AP neutral Transthoracic lateral Scapular Y-view AP and AP or PA lateral oblique Bilateral AP w/ & w/o weight bearing Pediatric Upper Extremity AP and lateral entire infant arm Toes AP entire foot 10 – 15* angle towards calcaneus, oblique, and lateral (no angle) Elbow Trauma Humerus Humerus Trauma Clavicle Shoulder Shoulder Trauma Foot Ankle Calcaneus Tibia/Fibula (Lower Leg) AP (10* angle), oblique, and lateral AP, oblique, left lateral, and mortise AP plantodorsal axial and lateral-mediolateral AP and lateral RTC 101 – Appendix A – 1 CONTINUED BODY PART Knee Patella POSITION/S REQUIRED AP, lateral, and both obliques Intercondylar Fossa Holmblad (kneeling position, 60* - 70* flexion),Camp Coventry (prone 40* - 50* flexion), and Beclere Method (AP axial 40* flexion, 40* CR angle) Merchant view (supine, flexion 40*), Settegast (prone, flexion 90*), and Hughston view (prone, flexion 55*) Femur AP and lateral Trauma lower extremity AP and lateral ankle with body part in 45* rotation Pediatric Lower Extremity AP and lateral entire infant leg RTC 101 – Appendix A – 2