File
advertisement

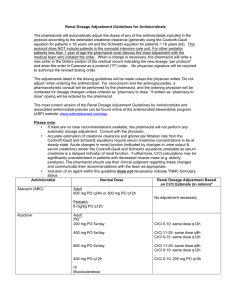
Nayri Hatsakorzian Pharm.D/MPH candidate 2014 Touro University- CA Who should be admitted to ICU? Direct admission to ICU is required for patients with: 1- 2 major criteria - Septic shock requiring vasopressors - Acute respiratory failure requiring intubation and mechanical ventilation 2- at least 3 of the minor criteria - PaO2/FiO2 ratio 250 (arterial oxygen pressure/fraction of inspired oxygen) - Multilobar infiltrates - Leukopenia (WBC <4000) - Thrombocytopenia (PLT <100,000) - Hypothermia (core temp <36C) - Hyponatremia - Hypoglycemia (in non-diabetic patients) - Acute alcoholism/alcoholic withdrawal - Unexplained metabolic acidosis - Elevated lactate levels - Cirrhosis - Asplenia - CURB-65 o Confusion/disorientation o Uremia (BUN ≥ 20) o RR ≥ 30 Diagnostic testing Obtain blood culture, sputum culture, legionella UAT, Pneumococcal UAT - ICU - Pleural effusion - Active alcohol abuse patients Obtain blood and sputum culture - Cavity infiltrates Obtain blood cultures and Pneumococcal UAT - Leukopenia - Chronic severe liver diseases - Asplenia o Blood Pressure o Hypotension requiring aggressive fluid resuscitation Etiologies of CAP: Outpatient: - Streptococcus pneumoniae - Mycoplasma pneumoniae - Haemophilus influenzae - Chlamydophila pneumoniae - Respiratory viruses Inpatient (non-ICU) - Streptococcus pneumoniae - Mycoplasma pneumoniae - Haemophilus influenzae - Chlamydophila pneumoniae - Legionella species - Aspiration - Respiratory viruses Inpatient (ICU) - Streptococcus pneumoniae - Staphylococcus aureus - Legionella species - Gram negative bacilli - Haemophilus influenzae CA-PNA Empiric treatment OUTPATIENT Previously healthy with no ABX tx for the past 3 month PO: 1st line: Macrolides Azithromycin (Zithromax) 500 mg PO day1 then 250mg day 2-5 - Adjust azithromycin when CrCl <10 Clarithromycin (Biaxin) 250mg PO every 12 hours for 7-10 days - Decrease clarithromycin by 50% when CrCl < 30 Alternative to macrolides is Doxycycline - (Vibramycin, Doryx) 100 mg PO twice daily - No renal adjustment is needed - Macrolides active against most common pathogens including atypicals - Erythromycin is not used d/t major GI side effects and losing efficacy against H. influenzae OUTPATIENT Presence of comorbidities (COPD, CHD, liver, renal diseases, DM, alcoholism, malignancies, asplenia, immunosuppressing conditions or use of immunosuppressing drugs). Or ABX tx the past 3 months (use different ABX: If patient received FQ then use macrolide and V.V) Respiratory FQ Levofloxacin (Levaquin) 750mg PO daily for 5 days o Adjust frequency when CrCl < 50 Moxifloxacin (Avelox) 400 mg PO daily for 7-10 days o No renal or hepatic dose adjustment is necessary Gemifloaxacin PO 320mg daily for 7 days Or: B-lactam + macrolides Amoxicillin 1g three times daily o Adjust dose renally when CrCl < 30 Augmentin (Amoxicillin-Clavulanate) 2g twice daily for 7-10 days o Adjust dose renally when CrCl < 30 o Hepatic adjustment is necessary Ceftriaxone (Rocephin) 1g daily for 7-10 days o No adjustments necessary Cefpodoxime (Vantin) 200mg PO twice daily for 14 days o Decrease frequency to every 24 hours when CrCl < 30 Cefuroxime (Ceftin) 750 mg every 8 hours o Decrease frequency to every 24 hours when CrCl < 10 NON-ICU PATIENTS: Respiratory FQ Levaquin 750 mg IV daily Moxifloxacin IV Gemifloaxacin (Available PO only) Or: B-lactams + macrolides Ceftriaxone 1-2g IV (IM) daily Cefotaxime (Claforan) 1-2g IV (IM) every 8 or 12 hours depending on severity of infection o Decrease dose by 50% when CrCl < 20 Ertapenem (Invanz) 1g IV (IM) daily for 10-14 days o Decrease Ertapenem by 50% when CrCl < 30 o Ertapenem has activity against S. pneumoniae and similar coverage to CTX and cefotaxime, but is inactive against atypicals and Pseudomonas aeruginosa. ICU PATIENTS: Pathophysiology PNA is an acute infection that inflames the pulmonary parenchyma. PNA is associated with a constellation of features such as cough, sputum production, fever, chills, difficulty breathing, and acute infiltrates that is demonstrable on chest x-ray. Some terminology from CXR impressions. Pulmonary edema: build up of fluid in the alveoli leading to SOB. Pulmonary edema is mainly caused by CHF. When blood is not pumped efficiently from heart, the returning blood can back up into the veins and lungs. The pressure and the fluid build up the normal oxygen/carbon dioxide exchange leading to SOB and the feeling of drowning. Pneumothorax: is a collapsed lung due to collection of air in the space around the lungs. The air build up exerts pressure on the lungs causing it not to expand as much during breathing Pericardial effusion: pericardium is a double layered, sac like structure that surrounds the heart and maintains its normal function. This double layered sac usually has fluid within, but when the fluid exceeds the limits due to blood build up, inflammation or infection, it exerts pressure on the heart causing SOB, heart failure and, if left untreated, death. Duration - 5 days - Afebrile for 48-72h and - No more than 1 CAP signs of clinical instability - Longer duration of therapy may be needed if initial therapy was not active against the identified pathogen or was complicated with extrapulmonary infections such as meningitis or endocarditis. Switching from IV to PO and discharge Hemodynamically stable and clinically improving Able to ingest medications Normally functioning GI Discharge patients as soon as: They are clinically stable with no other active medical problems o Temperature 37.8C o HR 100 beats/min o RR 24 breath/min o SBP ≥ 90 o Arterial O2 saturation ≥ 90% or pO2 ≥60 on room air o Able to maintain oral intake o Normal mental status Have safe environment for continuous care Prevention: Influenza vaccine B-lactams + macrolides or FQ Cefotaxime Ceftriaxone Ampicillin/sulbactam (Unasyn) 1500-3000 mg every 6 hours o Decrease frequency to every 12 hours when CrCl <30 PLUS azithromycin or respiratory FQ If PCN allergy then FQ + aztreonam recommended Aztreonam (Azactam) 1-2 g IV (IM) every 6,8 or 12 hours depending on the severity of infection o Decrease dose by 50% when CrCl < 30 but keep same interval - PPSV Smoking cessation Cases of public health concern should be reported to state or local health department Hygiene and patient education Follow up evaluation If pseudomonas DOUBLE coverage Antipneumococcal, antipseudomonal b-lactams: Zosyn (piperacillin/tazobactam) 3.375g - 4.5 g IV every 6 hours for 7-14 days Cefepime (Maxipime) 1-2g IV every 12 hours for 10 days o Decrease frequency to every 24 hours when CrCl <60 rather than change dose Antipseudomonal carbapenems: Imipenem (Primaxin) 500mg IV every 6 hours or 1 g every 8 hours o See Lexicomp for dosing adjustment based on weight and CrCl Meropenem (Merrem) > 50kg 1g IV every 8 hours (< 50kg: 20-40 mg/kg q8hrs) o CrCl <26 decrease frequency to every 12 hours o CrCl < 10 decrease dose by 50% every 12 hours PLUS Ciprofloxacin (Cipro) 400mg every 8 hours o Adjust Cipro when CrCl < 30 Levofloxacin 750mg In Case of Allergies If FQ allergy then b-lactams + aminoglycoside and azithromycin If b-lactam allergy then aztreonam should be substituted Aztreonam + FQ + aminoglycoside If CA- MRSA then add vanco or Linezolid Reference: Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of CommunityAcquired Pneumonia in Adults. Clinical Infectious Diseases 2007; 44: S27-72 Guidelines for the Management of Adults with Hospital-acquired, Ventilator-associated, and Healthcare-associated Pneumonia Definitions: HAP: Defined as pneumonia that occurs 48 hours or more after admission, which was not incubating at the time of admission. If patients require intubation in case of severe HAP, then they should be manage similar to patients with VAP. VAP: pneumonia that arises more than 48-72 hours after endotracheal intubation. HCAP: Cover MDR pathogens - Any patient who was hospitalized in an acute care hospital for two or more days within 90 days of the infection - Resides in a nursing home or long term care facility - Received recent IV ABX tx, chemotherapy, or wound care within the past 30 days of the current infection - Attended a hospital or hemodialysis clinic - Family member with MDR pathogens - Immunocompramised patients Consider MDR pathogens when: - Antimicrobial therapy in the preceding 90 days - Current hospitalization of 5 days or more - High frequency of antibiotic resistance in the community or in the specific hospital unit - Presence of risk factors for HCAP Empiric Antibiotic Therapy for HAP HAP, VAP or HCAP Suspected Late onset (>5days) or risk factors for MDR pathogens Yes-See table 2 No- See table 1 Table 1: Initial empiric therapy for HAP/VAP/HCAP in patients with no known risk factors for MDR pathogens, early onset, and any disease severity Potential Pathogens Treatments (one of the following options only) Streptococcus pneumoniae Ceftriaxone Haemophilus influenzae Levofloxacin Methicillin-sensitive Staphylococcus aureus Moxifloxacin Antibiotic-sensitive enteric gram negative bacilli Ciprofloxacin Escherichia coli Unasyn Klebsiella pneumoniae Ertapenem Enterobacter species Proteus species Serratia marcescens Table 2: Initial empiric therapy for HAP/VAP/HCAP in patients with late onset disease or risk factors for MDR pathogens and all disease severity Potential Pathogens Treatments Streptococcus pneumoniae Antipseudomonal cephalosporin (OR) Haemophilus influenzae Cefepime 1-2g q8-12h Methicillin-sensitive Staphylococcus aureus Ceftazidime 2g q8h Antibiotic-sensitive enteric gram negative bacilli Antipseudomonal carbapenem (OR) Escherichia coli Imipenem 500mg q6h or 1g q8h Klebsiella pneumoniae Meropenem 1g q8h Enterobacter species B-lactam/B-lactamase inhibitor Proteus species Zosyn 4.5g q 6h Serratia marcescens PLUS MDR pathogens include: Antipseudomonal FQ (OR) Pseudomonas aeruginosa Ciprofloxacin 400mg q8h Klebsiella pneumoniae (ESBL) Levofloxacin 750mg daily Acinetobacter species Aminoglycoside Legionella pneumohila Amikacin 20mg/kg daily (Tr goal < 4-5 mcg/ml) Gentamycin 7mg/kg daily (Tr goal < 1 mcg/ml) Tobramycin 7mg/kg daily (Tr goal <1 mcg/ml) Methicillin Resistant Staphylococcus aureus ADD Linezolid 600mg q12h or Vancomycin 15mg/kg q12h (Tr goal should be 15-20 mcg/ml) Common & Possible Side Effects for Common Antibiotics Penicillin Unasyn, amoxicillin Cephalosporins Ceftriaxone Cefepime Fluoroquinolone Levaquin Avelox Cipro Macrolides Azithromycin Rash, urticaria, diarrhea, ALT/AST elevation, pseudomembraneous colitis, bronchospasm, and hypotension. Rash, diarrhea, BUN elevation (~1%), alk phos elevation, hemolytic anemia, aplastic anemia, allergic dermatitis, edema, angioedema, and creatinine elevations. Fever, HA, rash, pruritis, N/V/D, elevation of alk phos, BUN, creatinine, and bilirubin. Hyperkalemia, hyperphosphotemia, and hypercalcemia HA, insomnia, dizziness, rash, pruritis, abdominal pain, dyspepsia, diarrhea-can be C.diff associated, constipation, arrhythmias, QT prolongation, TdP, and psychosis. Above mentioned plus AST/ALT, alk phos, BUN, and creatinine elevation, hypokalemia, hyperglycemia, hyperlipidemia, triglycerides and uric acid increase PT/INR prolongation - All FQ have category C interactions with Warfarin QTc prolongation- have category C interaction with Warfarin Combination with Amiodarone should be avoided