SEA Audit Report - NIPACS - Business Services Organisation
advertisement

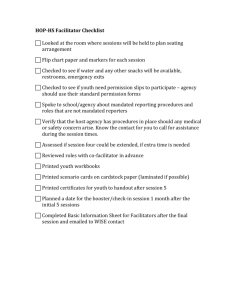
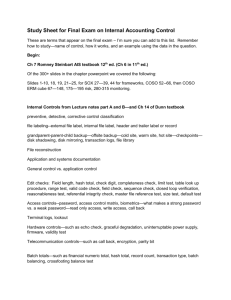
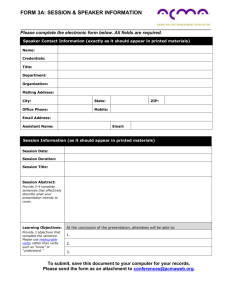
Paper BSO 16/2015 To: BSO Board From: Director of HR&CS Subject: Significant Event Audit Report Status: For Noting Date of Meeting: 29 January 2015 As part of the Serious Adverse Incident process BSO has been required to undertake a Serious Event Audit about a case identified on 02 October, 2014 which is described in the attached papers. This report is being submitted to the Board as part of the on-going formalisation of the reporting adverse incidents as required by a recent Audit report into Information Governance. The Board is asked to note the content of the report which has been forwarded to the HSCB. Enc Paper BSO 16/2015 LEVEL ONE – SIGNIFICANT EVENT AUDIT REPORT TITLE: DATE OF SIGNIFICANT EVENT: DATE OF SIGNIFICANT EVENT MEETING: NIPACS unprinted paper reports 2/10/14 Date issue was discovered 3/10/14 David Bryce, Hugh Fullerton and Nicky Harvey 6/10/14 David Bryce, Karen Bailey, Carolyn Harper and Nicky Harvey 15/10/14 David Bryce, Hugh Fullerton, Nicky Harvey with Sectra UK and Sweden integration and RIS specialists including Sectra MD and NIPACS Account Manager Daily conference calls between Sectra, Nicky Harvey SEA FACILITATOR/ LEAD OFFICER: TEAM MEMBERS PRESENT: WHAT HAPPENED? The NIPACS managed service is a regional diagnostic imaging service which is used by Radiology departments and clinicians across HSC. This incident relates to a failure to print out examination reports after they have been authorized by a Radiologist. The Radiology Pathway is as below: Patient is referred to the Radiology Department either via electronic or paper request Patient is either x-rayed at the time or an appointment sent out via post. This workflow is all managed through the RIS (Radiology Information System) Patient attends and Imaging is undertaken, the images are stored in the PACS The radiologist then reports these images on the RIS and when content with the report they authorise it. This then sends the report electronically to the PACS, to IUVO for GP clinical systems and ECR and to Sectra Connections (NIPACS Electronic referral system) The report is then printed via batch print function in the RIS for most departments with exception of GP’s and a few clinicians or wards who have opted out The paper report is then posted via internal mail and delivered to the referring consultant, who is responsible for reviewing and actioning Although NIPACS provides a completely electronic service, the current workflow used by most HSC referrals (with the exception of GP referrals) is that the paper report is printed and manually transported to the referrer. If this does not happen for any reason, then the risk is that the examination result is not followed up by the referrer. This risk exists outside the NIPACS service but in this incident a number of reports which should have been printed after authorization were not printed. It should be clear that all reports were available electronically and no reports have been lost. The incident relates to the failure to print out some reports on paper at the stage when they have been authorised. NIPACS does have a facility for electronic acknowledgement of results but this is not being used by clinicians. Using an electronic results signoff facility either within NIPACS or elsewhere (NIECR is being piloted) would remove the dependence on paper reports. In response to an issue with printing on the 10/09/14. The NIPACS service manager asked Sectra for an analysis of all authorized reports which had no record of being printed in the period since the system went live in 2009. Paper BSO 16/2015 This analysis identified three batches of reports which met these criteria. The total number of reports was 8147. During this period the total number of reports excluding GPs was 4 426 367 . The first batch of reports occurred after June 2011 when a change to how reports were extracted was implemented (a NIPACS system change) and a second batch occurred before June 2011 and a third batch were identified to have occurred between March 2010 to October 2014 All of these reports were checked to ensure appropriate follow up occurred based on report findings. Out of 8147 reports , the 5 instances below still await confirmation that the reports below have been followed up. The referring clinicians have been contacted and we are still awaiting a response on these individual cases 1. 2. 3. 4. 5. Testicular orchitis (inflammation) - June 10 Possible elbow fracture - April 10 Abnormal brachial pressure index - Feb 11 Recommended sigmoidoscopy if clinically relevant – March 12 Delayed cancer diagnosis May 10, see below for more detail In Instance No 5, this has been raised as a separate SAI by the Southern Trust. In this instance, a Portuguese non English speaking patient attended Craigavon A&E on 10th May 2010 with abdominal pain. A&E requested two x-rays, one of his chest and one of his abdomen. He was admitted and underwent further investigation due to his original complaint which was identified as pancreatitis and was discharged after a few days. The PACS audit log functionality at that time did not identify the individuals who looked at the patient’s chest x-ray; this type of audit has been possible since 2012. The chest x-ray taken on the 10 May 2010 in A&E was not reported until 31st August 2010, over 3 months later. A suspicious finding was noted in the report and it recommended further investigation and that additional views of the chest should be undertaken. The report was printed on the morning of the 31st August 2010, before it was authorized. It is speculated that this was so it could be highlighted to referring department, A&E, as an urgent report but this information is not recorded in the RIS. This information would not be recorded even if the report had then been printed again via batch print list subsequent to authorization. Since 2011 a journal entry within the RIS is created highlighting who was informed of any urgent, critical or unexpected finding and when this occurred and who provided this information. This functionality was not available at this point in time. It would appear that the printed report was then not actioned or followed up. The report was then authorised on 1st September 2010 but was not reprinted via the batch print list which would have been sent to A&E with all other reports for this department. The Patient was referred by his GP for a further chest x-ray on 1st June 2011 which showed a mass in his lung. The fact that there was an earlier report relating to this appears not to have raised as a SAI by the Southern Trust at that time. The Patient underwent further tests, had both chemotherapy and radiotherapy treatment but died on 2nd January 2014. Paper BSO 16/2015 WHY DID IT HAPPEN? BSO have worked with Sectra to identify and rectify the three technical causes of the issues which are a mixture of implementation, configuration, design issues and software bugs in the NIPACS software over the 5 year period. These are described below. 1. Printing reports before they are authorised provides a paper report at that time but prevents the report from being printed again via batch print list once authorized. The batch printing process was configured to print out all of those authorized reports which were not electronically sent back to the referrer. In order to do this Sectra ran a number of overnight batch jobs to change the status of each report. If the request was edited between the overnight batch job running and the report being printed then the status was modified so the report did not come out on the batch print. If the configuration of referral source masterfile entry was set up incorrectly this could prevent a report being available on the batch print list. Administrators manually set up all referral sources in the masterfile and define whether they are included in batch print list. Some referral sources were found to be incorrectly configured. 3. Batch printing Configuration was incorrectly set up at Southern and Western NIPACS shortly after go live in 2010 with the impact that some reports were not printed at that time. 2. A number of changes have been defined and implemented to rectify the shortcomings identified. Sectra are also developing further reporting mechanisms to clearly identify unprinted reports as a further control mechanism. WHAT HAS BEEN LEARNED? The current batch printing configuration was complicated and prone to failure and has been amended via a patch/ fix for the current RIS software. There are also plans to upgrade the RIS software to a new version. A pilot is running to provide further integration with ECR which would provide electronic results acknowledgement for both Radiology and Laboratory tests. There is a need for constant monitoring to identify and follow any reports which are not printed for any reason and reporting facilities to do this have been enhanced. These actions will not address the broader risks which arise from the continued use of a paper report as the primary mode of feedback on examinations to referrers. Royal College Guidelines specifically advise against this process being the sole feedback channel and advocates the use of electronic results acknowledgement. For example , a Safer practice notice from 2007 states “In the long term, it is proposed that radiological imaging reports should be routinely provided in a comprehensive EPR system and that this should include functionality to acknowledge receipt of the information”. Only electronic results acknowledgment will remove the inherent risk associated with a paper report being required to trigger a patient review. Paper BSO 16/2015 WHAT HAS BEEN CHANGED? Reporting turnaround times in Southern Trust currently meet DRTT guidelines Urgent report RIS workflow is in place (2011) which identifies which referrer was directly contacted, when and by whom PACS audit log now identifies which logged-in user accesses patient images (2012) PACS Managers have been reminded staff that reports should not be printed before they are authorised. However, a fix to the RIS software implemented in September 14 has ensured that this no longer creates same issue. Further configuration and software changes have been applied on 3rd December 2014 which will address the risk of recurrence of all other scenarios which have been identified above. Monitoring has been set up to identify any reports not printed. Worklists have been created within NIPACS that can be managed by Sectra, Trust PACS Mangers and NIPACS Services Manager so any further problems will also be identified in real time. NIECR has sign off functionality and this is being developed into an electronic results acknowledgement system which will cover both radiology and laboratory test. This is currently being piloted. RECOMMENDATIONS FOLLOWING THE LEVEL ONE SEA: It is imperative that the use of paper reports as the primary mode of feedback to a referrer is discontinued. It is recommended that a full electronic results acknowledgement system is implemented and utilised for 100% of activity by all referrers. Electronic results acknowledgement would be more efficient, ensure that reports have been read, allow monitoring of this process and increase the likelihood of follow-up in all cases where it is necessary. The Electronic results acknowledgement functionality within ECR would need further development to ensure that any recommendations in a report were actioned by the referring clinician. Where a Level two or three investigation is recommended please complete the sections below. THE INVESTIGATION TEAM: INVESTIGATION TERMS OF REFERENCE: