Laura
advertisement

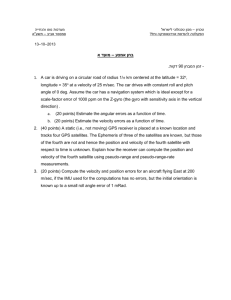
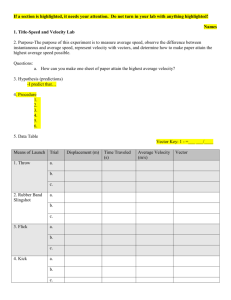
AN UNUSUAL CASE OF FOREIGN BODY PULMONARY EMBOLUS: CASE REPORT AND REVIEW OF PENETRATING TRAUMA AT A PEDIATRIC TRAUMA CENTER Laura A. Boomer, MD*, Daniel J. Watkins, MD, Julie O’Donovan, MD, Brian D. Kenney, MD, Andrew R. Yates, MD, Gail E. Besner, MD Nationwide Children’s Hospital Departments of Pediatric Surgery, Radiology and Cardiology 700 Children’s Place, Columbus, OH 43206 Background: Penetrating thoracic trauma is relatively rare in the pediatric population, accounting for only 10-20% of all pediatric thoracic trauma. Embolization of foreign bodies from penetrating trauma is very uncommon. We present a case of a 6 year old boy with a penetrating foreign body from a projectile thrown from a lawn-mower with embolization to a pulmonary artery branch. Objective: The purpose of this study was to describe a rare case of foreign body pulmonary embolus and to review the pediatric patients presenting with penetrating thoracic trauma at a large pediatric trauma and tertiary care center. Methods: We reviewed the penetrating thoracic trauma patients in our trauma registry between 1/1/03 and 12/31/12, including the details of the specific case presented in more detail. Data collected included demographic data, procedures performed, complications and outcome. Patients with low velocity wounds (i.e., knife stab wounds) were compared to those with high velocity wounds (i.e., gunshot wounds). Results: A 6 year old male presented to the trauma center after sustaining a penetrating injury to his chest from a projectile thrown from the underside of a lawn-mower. The patient presented with pericardial tamponade requiring pericardial tube drainage. Imaging demonstrated a foreign body that embolized to the left pulmonary artery. Seventy patients were initially identified in the trauma database, 65 of whom were included for review after confirming the presence of penetrating trauma to the chest. Fourteen of the patients (21.5%) had low velocity penetrating trauma and 51 (78.5%) had high velocity injuries from gunshot wounds. Seven fatalities occurred, all of which were from high velocity wounds (p=0.331). Patients with high velocity injuries were more likely to be older (12.9 vs. 9.5 years old; p=0.018) and less likely to be Caucasian (p=0.002). There were no statistically significant differences between patients with low velocity injuries and those with high velocity injuries regarding injury severity score (ISS), combined total abbreviated injury score (AIS), Glasgow Coma Scale (GCS) at initial presentation, length of stay (LOS), intensive care unit (ICU) LOS, or days requiring mechanical ventilation. There were no statistically significant differences in procedures required between patients with low velocity wounds versus those with high velocity wounds. This review demonstrates that penetrating trauma with foreign body embolization may be able to be treated non-operatively. Laura Boomer Nationwide Children’s Hospital, Department of Pediatric Surgery 700 Children’s Place, Columbus, OH 43205 Ph: 614-722-3879 Fax: 614-722-3903 laura.boomer@nationwidechildrens.org Figure 1. A.) Chest radiograph demonstrating a linear, metallic density at the level of the right hilum. This radiograph was performed at 23:35 on the day of admission. B.) Repeat chest X-ray performed 30 minutes later demonstrating the foreign body overlying the left cardiac silhouette, concerning for possible intracardiac migration. C.) Maximum intensity projection (MIP) coronal image (10 mm thickness) from CT scan performed 8 hours after initial presentation, demonstrating the foreign body lodged in the distal left pulmonary artery (arrow). The other density visualized is a naso-gastric tube. A. B. C. Table 1. Demographics of patients with penetrating chest trauma. High velocity wounds were from firearms whereas low velocity wounds included all other penetrating wounds. All values represented as number (%) except for age which is shown in years. P-values compare low velocity vs. high velocity values. Number of Patients Age, mean (range) Sex Male Female Race White Black Asian/PI 2 or more other Insurance Private Medicaid None All Patients 65 Low Velocity 14 (21.5%) High Velocity 51 (78.5%) p-value 12.16 (1.33-20) 9.53 (2.42-16) 12.89 (1.33-20) p=0.018* 53 (81.5%) 12 (18.5%) 10 (71.4%) 4 (26.6%) 43 (84.3%) 8 (15.7%) p=0.271 27 (41.5%) 28 (43.1%) 6 (9.2%) 2 (3.1%) 2 (3.1%) 12 (85.7%) 1 (7.1%) 0 (0%) 0 (0%) 1 (7.1%) 15 (29.4%) 27 (52.9%) 6 (11.8%) 2 (3.9%) 1 (2.0%) 20 (30.8%) 25 (38.5%) 20 (30.8%) 5 (35.7%) 5 (35.7%) 4 (28.6%) 15 (29.4%) 20 (39.2%) 16 (31.4%) p=0.002* p=0.903 Laura Boomer Nationwide Children’s Hospital, Department of Pediatric Surgery 700 Children’s Place, Columbus, OH 43205 Ph: 614-722-3879 Fax: 614-722-3903 laura.boomer@nationwidechildrens.org Table 2. Severity of Injury. All data represent mean standard deviation (range). ISS = injury severity score; AIS = abbreviated injury score; GCS = Glasgow Coma Score; LOS = length of stay; ICU = intensive care unit ISS Total AIS Initial GCS LOS ICU LOS Ventilator Days All Patients 17 + 14 (1-75) 10 + 7 (1-36) 13 + 4 (3-15) 6.3 + 9.0 (1-45) 1.4 + 4.5 (0-36) 0.5 + 1.6 (0-12) Low Velocity 12 + 7 (1-26) 7 + 5 (1-17) 14 + 3 (3-15) 3.6 + 2.2 (1-9) 0.6 + 0.7(0-2) 0.1 + 0.4 (0-1) Laura Boomer Nationwide Children’s Hospital, Department of Pediatric Surgery 700 Children’s Place, Columbus, OH 43205 Ph: 614-722-3879 Fax: 614-722-3903 laura.boomer@nationwidechildrens.org High Velocity 18 + 16 (1-75) 11 + 7 (1-36) 13 + 4 (3-15) 7.1 + 9.9 (0-45) 1.6 + 5.1 (0-36) 0.6 + 1.8 (0-12) p-value p=0.331 p=0.090 p=0.637 p=0.640 p=0.356 p=0.152