link-c-diff - St. Mary`s Hospital
advertisement

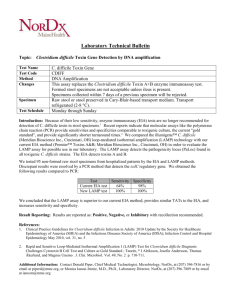
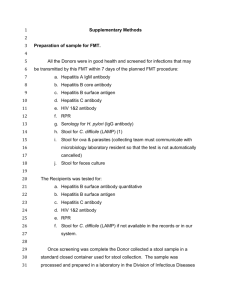
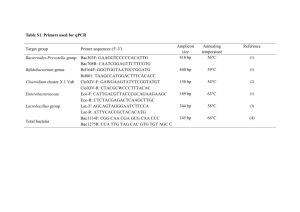
Antibiotic Stewardship by Geri Naymick (PharmD) * Dr. James Levin (infectious disease) * Dick Dern (microbiology) C. Difficile Lab Testing What is the difference between the lab testing for C. Difficile infections (CDI) at Dean Clinics versus St. Mary’s Hospital? Test Comment Lab Site Turnaround Time Sensitivity Specificity Toxin A/B EIA Moderate sensitivity Dean clinic 2 hrs 53-77 % 95-100 % High sensitivity & negative predictive value St. Mary’s Hospital Submit specimen by 9am -> results available 1pm 77-100 % 93-100 % Enzyme immunoassay Toxin B gene PCR Nucleic acid amplification Although the EIA provides results in a short time period, there is an issue of false negatives due to its decreased sensitivity. Use of PCR (polymerase chain reaction) testing is becoming the accepted standard because of its high sensitivity and negative predictive value. Due to the complexity and expense of testing, “batch” sample testing is done. What if the PCR test result is negative? A negative PCR test excludes C. Difficile infection. What about repeat testing? Serial testing of 3 or more stool samples has been associated with the EIA method. This practice is based on early literature that suggested the negative predictive value of EIA test may increase by up to 10% by testing three specimens. However, the unintended consequence of repeat testing is an increase in false positive results.1 Multiple studies have demonstrated that repeat PCR testing confirms a negative result2,3,4. Researchers at Stanford and Mayo found that no useful information was provided if repeated within 7 days (0.5% and 2.9%, respectively, changed to positive)2,3. In patients who remain symptomatic and have ongoing risk factors for CDI (continuing antibiotic use, prolonged hospitalization), repeat testing between 7-14 days of an initial negative test increases the potential for a positive test (1.7% and 4.8%, respectively, convert to positive)2,3 . For more detail, click on this literature review chart. Should I order a repeat test prior to patient discharge to a nursing home or assisted living facility? A “test of cure” is not recommended5. Clinical response of the patient (formed stools, normalization of white count) is the target outcome. A positive test may represent asymptomatic colonization or false positive due to PCR sensitivity. What if therapy is initiated prior to obtaining the stool sample? It is best to obtain the stool sample prior to treatment if possible. There is a potential for false negative due to conversion (for PCR, 14%, 35%, and 45% after 1, 2, and 3 days of treatment, respectively)6. How does Epic support C. Difficile diagnostic testing and treatment? There is a C. Difficile order set. A drug therapy algorithm is available as an icon in left hand corner of order set. References: 1 Laboratory 2 Is tests for the diagnosis of clostridium difficile infections. Clin Microbiol Newsletter 2012;34(19):151-157 repeat PCR testing needed for diagnosis of C difficile infection? J Clin Microbiol 2010;10:3738-3741 3 An evaluation of repeat stool testing for C difficile infection by PCR. J Clin Gastroenterol 2012;46:846-849 4 Nonutility of repeat lab testing for detection of C difficile by use of PCR or EIA. J Clin Microbiol 2008;46:3795-3797 5 APIC guide to preventing Clostridium difficile infections: 2013 www.apic.org/implementationguides 6 Does empirical clostridium difficile infection (CDI) therapy result in false-negative CDI diagnostic test results? Clin Inf Dis2013;57(4):494-500