here. - The Massage Therapist Development Centre
advertisement

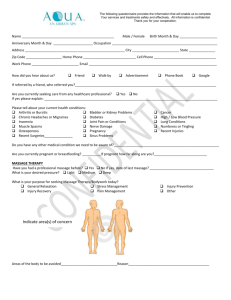
Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities: A case study Chelsea L. Frenkel Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities Acknowledgements I would like to express my gratitude to Matthew Fleet, RMT for his amazing guidance as my advisor throughout this study. I would also like to thank the supervisors and staff at WCCMT Victoria who took the time to offer detailed suggestions, encouragement, and interest. Finally, many thanks to the subject and parent guardian of this study, without dedication and willingness to follow through with treatment this study would not have had such clear results and this excellent learning opportunity would not have been available to me. 2 Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 3 Table of Contents Abstract……………………………………………………………………………4 Introduction………………………………………………………………………..6 Methods……………………………………………………………………………9 Client profile………………………………………………………………9 Assessment protocol.……………………………………………….……12 Treatment Protocol………………………………………………………16 Results……………………………………………………………………………22 Discussion………………………………………………………………………..28 References………………………………………………………………………..32 Appendix…………………………………………………………………………33 Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 4 Abstract Objective: To determine if the effectiveness of massage therapy could improve focus, behavior and motor function in children with developmental disabilities. Case participant: The patient is a nine year old male with a diagnosis of Pervasive Development Delay (PDD), moderate intellectual disability, asthma, seizure disorder, and an educational designation of physical disability or chronic health impairment (PDCVH). The patient also experiences challenges with focus, aggression, and functional movements as a part of his diagnosis. Methods: This case study was performed over the course of three months and was broken into fifteen treatments, seventy minutes in duration, which were divided into three phases (phase 1- introduction to touch and massage, phase 2behavior and focus, and phase 3- motor function). Treatments consisted of manual modalities to the lower extremities and back such as: deep pressure general Swedish techniques, myofascial release techniques, joint mobilizations and vibration techniques. Measurement tools included; postural assessment, gait analysis, orthopedic tests, and Range of motion (ROM) for the motor function aspect of the study as well as focus tests and qualitative feedback from the patients’ guardian for the focus and behavior aspect. Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities Results: the results from the case study concluded that the patients focus and behavior had improved, the patient had become more social with other children, less aggressive with others at times of frustration, less anxiety, and the client’s balance, motor function, gait, and posture had improved. Conclusion: During this case study, massage therapy had proven to significantly improve the patient’s focus, behavior, and motor function therefore improving quality of life. Key words: Pervasive Development delay, children, behavior, motor function, massage therapy 5 Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 6 Introduction Developmental disabilities are common in children and occur in all racial and socioeconomic groups. Such developmental disabilities may include Attention Deficit Disorder (ADD), Autism Spectrum Disorder, Cerebral Palsy, Downs Syndrome, intellectual disorders, hearing loss, vision impairment, learning disabilities, and other development delay. One in six or fifteen percent of children in the United States of America from ages three to seventeen have these developmental disabilities according to the Center for Disease Control and Prevention. In that fifteen percent, Autism spectrum disorder and or Pervasive Development Delay (PDD) are very common and come with varying ranges of qualitative impairments. Children with Autism or PDD may experience impairments in some or all of the following: in social interaction, communication, speech and language, general physical development, behavior, learning, and cognitive skills. Massage therapy has been proven useful in helping these children with their associated qualitative impairments and has been shown beneficial in improving sleep, behavior and focus impairment. According to the Journal of Early Child Development and Care, authors Hernandez‐Reif, M., Field, T., Largie, S., Mora, D., Bornstein, J., & Waldman, R. (2006), children with Downs Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 7 Syndrome who received massage therapy revealed gains in fine and gross motor functioning and less severe limb hypotonicity. The treatments were spanned over eight weeks , were thirty minutes in duration, and consisted of whole body general Swedish massage and non Swedish massage techniques. A study by Escalona, A., Field, T., Singer-Strunck, R., Cullen, C., & Hartshorn, K. (2001), found massage therapy for children aged three to six with Autism Spectrum Disorder, resulted in less stereotypic behaviour and the children demonstrating more on-task and social relatedness behaviour at school. They also experienced fewer sleep problems. Treatments were performed fifteen minutes before bed, on a daily basis for one month. Both studies used slow, general Swedish massage techniques in their studies and according to Rattray and Ludwig (2000) Swedish massage techniques applied in a slow, rhythmical and repetitive manor will result in a response of relaxation and decrease sympathetic nervous system firing. These results can be complimented with the use to hot hydrotherapy and other non Swedish massage techniques to achieve physiological and psychological effects to treat the clients’ condition. The purpose of this study is to evaluate the effects of therapeutic massage, which included the modalities of General Swedish Massage (GSM) and non Swedish massage (muscle approximation, golgi tendon organ release (GTO release), myofascial release (MFR), vibrations, rocking, neutral warmth Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 8 hydrotherapy, and joint mobilizations) to improve motor function, focus and behaviour in a patient with diagnosed pervasive development delay (PDD) and seizure disorder. Swedish massage was used in this study as it has proven to be beneficial in previous studies and also as explained in Rattray and Ludwig, could have great effects for the client. The non Swedish massage techniques that were chosen to decrease muscle tone in spastic muscles included muscle approximation, GTO release, and high frequency vibrations due to the neurological affects to decrease hyper tonicity. According to Rattray and Ludwig (2000), the technique of muscle approximation uses the reflex effect of muscle spindles to reduce tone or spasm in a muscle. This technique is done by approximating, or bringing the ends of muscle closer together, which results in decreasing the stretch on the muscle spindles. This decreases gamma firing and reduces muscle tone and firing”. Also according to Rattray and Ludwig (2000), the GTO release technique can also be used to decrease spasm and tone within a muscle. Its primary effect is on the Golgi Tendon Organ, which is part of a protective reflex to prevent the muscle injury by relaxing the muscle. This reflex is stimulated when excessive load is placed on the tendon. This technique involves placing direct compression to the musculotendinous junction to decrease tone within the muscle. Vibrations were used as they can play a part in both decreasing muscle tone and, in the case of the client taking part in the study, as a sensory stimulation and central nervous system distraction technique. MFR was Can massage therapy improve focus, behavior, and motor function in children with developmental disabilities 9 used to help decrease restrictions that caused hyper tonicity. Joint mobilization techniques were applied on the ankle to increase dorsi flexion (posterior glide) during phase three of the case study. According to Rattray and Ludwig (2000) this technique assesses joint dysfunction, increase range of motion, stretch tight capsules, reduce adhesions, pain and spasm, and encourage the proper action of the joint. The primary objectives of treatment interventions were to determine if massage therapy could decrease adverse behaviour such as hitting or scratching when frustrated, and full body rocking behaviour when anxious, improve focus and learning ability, and improve motor function by decreasing hyper toned muscles, and increasing strength and firing of hypo toned muscles and encouraging proper movement within the joints, which could result in improved ambulation and balance. Methods Client Profile: The client participating in this case study is a nine-year-old male who is diagnosed with Pervasive Development Disorder (PDD), Physical Disability or Chronic Health Impairment (PDCVH), asthma, and seizure disorder. He has full time support from his parent guardian and two education assistants in his living skills program at school. The client also receives Occupational Therapy, Can massage therapy improve focus, behavior, and motor function in children 10 with developmental disabilities Physiotherapy, Speech therapy, and visits a sensory room twice weekly. The patient has a significant medical history of which includes atypical and long in duration seizures as an infant, globally and developmentally delayed yet verbal until a significant seizure in 2010 which caused a loss of verbal ability, and a grand mal seizure in November, 2013. Currently the patient is undergoing assessment by the Complex Developmental Behavioural Condition Clinic (CDBC) to explore a possible diagnosis of Autism Spectrum Disorder. As for Physical assistance, the patient also has been fitted for and wears custom orthotics to support pes planus. The patient takes the following medications: 600 mg of Trileptal two times daily plus 75 mg of Topomax twice daily which help treat his seizure disorder. These medications were increased in April 2014. After the medication increase, the patient had not experienced any seizure activity until September 2014, when he experienced a grand mal seizure. The client also takes Ativan as needed for anxiety and Provent and Ventalin as needed for asthma. With the patients’ diagnosis in PDD, he does experience some impairment in his emotional and behavioural status and is non-verbal. At times of frustration, the client often exhibits aggressive behaviours such as grabbing, hitting, scratching, and biting. Due to this behaviour, he had been denied massage therapy by registered massage therapists. When the participant experiences anxiety, he will elicit a rocking behaviour where he sits with his legs firmly crossed, ankles firmly in dorsi flexion, and toes firmly flexed as he rocks back and forth. These Can massage therapy improve focus, behavior, and motor function in children 11 with developmental disabilities behaviours often happen at times where the clients doesn’t receive enough sensory input or at times of frustration. The client also appears to not be very social with other children his age and prefers the company of adults. As for the clients’ focus and learning abilities, the client appears to attend mostly to sensory experiences and is easily distracted. He has a limited attention for unfamiliar, directed, or non- preferred activities. He also has emerging understanding of cause and effect. The patient is also impaired in many activities of daily living such as using the toilet, dressing himself, ambulation, balance, and properly going up and down stairs. When it comes to using the facilities, the clients learning and attention impairments distract him from learning this life skill. As for ambulation and balance, the client has both hypertoned and spastic muscles which include biceps femoris (long and short head), gastrocnemius, soleus, flexor halluces longus, flexor digitorum longus, and tibialis posterior (all of which present bilateral) and hypotoned muscles of which include gluteus maximus, gluteus medius, gluteus minimus, and tibialis anterior (all of which present bilateral) which cause the client to present with a sluggish gait. As for going up and down stairs, the client tends to lead with his left foot and goes one-step at a time. As part of the clients’ occupational therapy (OT) assessment, it was suggested that the client had a very strong threshold for sensory input and would benefit from extensive sensory stimulation such as auditory stimulation, visual stimulation, and tactile stimulation. The client reacts well with deep pressure and Can massage therapy improve focus, behavior, and motor function in children 12 with developmental disabilities vibration, which were taken into account towards his treatment plan. It was also mentioned that with receiving enough sensory input, the client would react positively. The clients’ physiotherapist (PT) also recommended that massage be indicated for the client’s presentation of impairments. As per the client’s parent guardian, some main goals of treatment included that he become more body aware, less anxious, more comfortable with touch, and more focused. The client had never received massage before, therefore phase one-introduction to touch was established as a key point of the case study to allow the goals of the clients support team, and the therapist, to be successful. Once phase one was completed, treatment strategies would become more specific as the client could tolerate the modalities. Phase two was concentrated on improving the focus and learning ability of the client while decreasing sympathetic nervous system firing and phase three would focus mostly on motor function and postural impairments while still maintaining relaxation goals. Assessment Protocol: Due to the clients’ physical and mental status the following assessment tools that were chosen best fit the clients’ ability to focus and participate. The majority of assessment in this case study mostly focused on a qualitative interview each treatment to determine the clients’ physical and mental status. Qualitative questions were asked every treatment visit. Such questions evolved around the clients’ sleep patterns, behaviour, focus, weekly routines, Can massage therapy improve focus, behavior, and motor function in children 13 with developmental disabilities mental or physical changes post treatment, learning activities, physical activity, routine changes, and other therapy. Along with the interview questions every treatment, therapist observations were also made. Observations included things such as emotional state, physical presentation, ability to focus and respond to direction, and gait when walking from reception to treatment room. Observations were also noted during treatment. During phase one especially, time length of remaining still was noted along with ability to relax, be calm, times of body awareness, and specific treatment modalities that had a positive affect. Observational changes will be noted in the results section. As for physical examination and assessment, upon the initial treatment, a postural scan was completed. Due to the lack of focus and mental awareness, a plum line was not used, as the client could not stand still and in line with the plum line however, the postural scan revealed a significant pes planus, genu valgum and internally rotated hips. It also revealed head forward posture. A postural scan was also preformed on the last treatment and revealed slight positive change. Results from this assessment will be revealed in results section. To further assess the postural impairments within the hips, knees and ankles, palpation was preformed to decipher the muscle tone and restrictions. This was preformed each treatment, however during the initial treatment, hypertonicity was found bilaterally in the: rectus femoris, biceps femoris long and short head, semimembranosus, semitendinosus, adductor group, triceps surae, peronials, Can massage therapy improve focus, behavior, and motor function in children 14 with developmental disabilities tibialis posterior, flexor halluces longus and brevis, and flexor digitorum longus and brevis. Hypotonicity was discovered bilaterally in the following: the gluteus maximus, medius, and minimus along with tibialis anterior, extensor digitorum lonus, extensor digitorum brevis, extensor digitorum longus and brevis. Results from palpation will be found in the results section. To further assess the lower extremity, range of motion (ROM) was bilaterally preformed passively (PROM) to the hips, knees and ankles. For the hips; flexion, extension, abduction, adduction, external rotation, and internal rotation was preformed. As for the knee, flexion and extension was preformed. For the ankle; plantar flexion, dorsi flexion, inversion, and eversion where preformed. These ranges of motion took part over the first four treatments; hip and knee PROM during the first three treatments, and ankle during the forth treatment. Hip range of motion showed full range of motion however internal and external rotation showed to be hypermobile. Knee range of motion showed full range of motion, and ankle as well however dorsi flexion was very limited. Range of motion of the ankle was then assessed again during phase three- motor function in treatment 11- where range of motion would be addressed further in treatment. PROM results are addressed further in table A of the results section. Upon discovery of hypotonicity with the hip abductors and excessive internal ROM, the Trendelenburg test was preformed from the second treatment onward. As explained in ‘Orthopedic Physical Assessment’, D.Magee(2008) Can massage therapy improve focus, behavior, and motor function in children 15 with developmental disabilities explains “this test assesses the stability of the hip and the ability of the hip abductors to stabilize the pelvis on the femur. The patient is asked to stand on one lower limb. Normally, the pelvis on the opposite side should rise; this finding indicates a negative test. If the pelvis on the opposite side (non stance side) drops when the patient stands on the affected leg, a positive test is indicated”. This test was chosen to determine if the client had weak hip stabilization due to the hypotonicity within the gluteals. Modifications were made to this test however, due to the lack of language understanding from the clients’ perspective. The modified test preformed was conducted in the following matter; the client was told to lift his leg and balance on the other while the guardian attempted to put his shoes on. While this took place, the client was observed to see if there was any hip drop on the opposite side of the stance leg and he was timed to determine how long he could stand on one leg for. Results from this test will be found in table B of the results section. To further investigate the hyper tonicity within the hip flexors, the Elys test was preformed. As outlined in “orthopedic Physical Assessment”, Magee (2008),”The patient lies prone, and the examiner passively flexes the knee. On flexion of the knee, the patient’s hip on the same side spontaneously flexes, indicating that the rectus femoris muscle is tight on that side and that the test is positive”. This test was preformed from the second treatment onward until the test Can massage therapy improve focus, behavior, and motor function in children 16 with developmental disabilities showed a negative result and the impairment was corrected. Results of this test will be presented in the results section. To test whether each treatment helped to decrease the patients sympathetic nervous system and to see whether the treatments has a relaxing effect on the client, heart rate was measured by taking the clients pulse via the radial artery. It was taken before and after each treatment. Results will be further presented in table C of the results section. As for testing the focus of the client, each treatment a finger flexion test was preformed. This was done pre and post treatment. The test was preformed to test how many fingers the client could focus on before becoming distracted with something else. It was created to be similar to a game. The therapist would make eye contact with the client then touch each finger one by one and ask the clients to apply pressure in the motion of flexion into their index finger. The test measured each hand separately. Results of this focus test will be shown in table D in the results section. Treatment Protocol: Each treatment was preformed clothed in shorts and undraped as the client moved a lot and seemed to prefer being on top of the sheets. The client was pillowed under the head and knees while in supine and prone. When work to the back was completed, the client was typically in three quarters prone as for his comfort. From treatment 4 onwards, a thermaphore was warmed up and placed on Can massage therapy improve focus, behavior, and motor function in children 17 with developmental disabilities the clients back while in prone, and abdomen while in supine. It was not kept on as it would get to hot; however the temperature was carefully monitored to remain warm but not hot throughout the treatments. The treatment room was also kept warm, as the client was not draped and was only clothed in shorts. The parent guardian also remained in the room during each treatment and would assist with emotional support when needed by the client, however, during treatment 14, the client’s education assistant took place of the parent guardian. As for focus and learning, following each treatment, the client was allowed to turn the light of the treatment room on and off as a reward to listening and participating. This was preformed after he got dressed and was completely done his treatment. As for a learning aspect, it helped teach a lesson of being rewarded after doing something asked of him and it also helped teach a skill of properly turning the light off and on. Results of this will further be discussed in the results section. As for actual treatment modalities, they were divided into three sections; phase oneintroduction to touch and massage, phase two- focus and behaviour, and phase three- motor function. Although there were results of improvements in focus, behaviour and motor function in all three phases, each phase best resulted in what the purpose of that phase was for. Each treatment through out the case study kept the same routine however modalities and assessment tools did change slightly throughout each phase. The routine began with client pickup in the reception area. The client Can massage therapy improve focus, behavior, and motor function in children 18 with developmental disabilities would be seated on the floor and be looking through books. The client would then be taken into the treatment room where he would sit on the floor and continue to look through his book while the interview took place between the therapist and parent guardian. Once the interview was completed, additional notes were taken by the therapist on the client’s behaviour, mood, etc. While notes were taken, the parent guardian assisted the client with getting changed. Assessment then took place and following that treatment began. Hands on treatment took about fifty minutes. Once that was completed, tests (pulse and finger focus test) were reassessed. The guardian then dressed the client and then the client was able to turn the light on and off. The clients was then instructed on how to open the door and then walked out to the lobby where he was instructed to put his book back on the shelf. Once the book was put away, the treatment session was complete. Phase One: treatments 1-3 The treatment modalities and goals for phase one- Introduction to touch, included the following goals of introducing the clients to massage modalities, increase body awareness of the client, assist the therapist in finding which modalities best suited the client, and introduce the client to touch. Phase one of treatment occurred during the first three treatments of the case study. During this time, sensory devices were a part of treatment. These devices consisted of a book to look through, shoe laces to play with, and a light up turtle that played music. The treatments modalities are as followed: Can massage therapy improve focus, behavior, and motor function in children 19 with developmental disabilities Assessment tests included PROM of hips, knees and ankles, postural scan, pulse (pre and post treatment), Elys test, Trendelenburg test, and palpation. The client was first started in supine and the therapist preformed full body compressions followed by gentle rocking. PROM to the hip, knee, and ankle followed by vibrations and shaking to the lower extremity was preformed to lower extremity. General Swedish massage (GSM) (Rattray, 2000) techniques: longitudinal palmar stroking, forearm stroking, fingertip kneading, c-scooping, and wringing to the quadriceps group. In between each technique, vibration and shaking was applied briefly to help decrease the movement of the client’s leg. Finished with a full anterior leg longitudinal flushing strokes. This routine was applied over vastus medialis muscle, vastus intermedius muscle, vastus lateralis muscle, and rectus femoris muscle, also known as the quadriceps femoris group (quads) and adductors group, sartorius and gracilis muscles, tibialis anterior, extensor digitorum longus, extensor halluces longus, and peronials. This routine was completed bilaterally. The client was then turned over to prone where the same techniques were applied as the anterior leg, however muscle approximation and isolytic release was to gastrocnemius, soleus, and the hamstrings group; and GTO release was applied to the Achilles tendon. GSM flushing techniques were then applied over the whole posterior leg followed by compressions over the gluteals, posterior leg, and foot. Treatment then continued onto the back where GSM techniques were applied to the back including longitudinal palmar stroking, Can massage therapy improve focus, behavior, and motor function in children 20 with developmental disabilities forearm stroking, fingertip kneading, c-scooping, and wringing. MFR to the thoracolumbar fascia was also applied. The treatment finished with a bilateral legpull. Phase two: Treatments 6-10 Treatment goals for phase two- improvement of focus and behaviour were to increase focus and behaviour of the client during and after treatment, decrease the amount of sensory stimuli needed during treatment, and to decrease sympathetic nervous system firing which would decrease the amount of muscle spasticity and movement of the lower extremity. During this phase, the client was still allotted a book before treatment started during the assessment but then was taken away during the treatment. A thermaphore became part of the treatment as a sensory tool as weight and heat can create a relaxing effect to sensory seeking children according to Chasnoff (2011). It was applied throughout the treatment and placed on the abdomen with a warm temperature during anterior leg work, placed on the back during posterior leg work, and placed of the posterior legs during back treatment. The use of the thermaphore had an instant calming effect on the client when it was applied. The treatment room was made dark during treatment and the light up turtle was still used. Treatment modalities continued with the same sequence as phase one, however some new techniques were added as the client was able to remain still for longer. Can massage therapy improve focus, behavior, and motor function in children 21 with developmental disabilities Assessment included pulse (pre and post treatment), finger focus test, trendelenburg test, elys test and palpation. Modalities were as followed: The treatments remained with the same sequence as in phase one however, tapotement to tibialis anterior was added to increase muscle firing, isolytic release to the adductor group was added to decrease muscle hypertonicity, and light joint play to the hips and ankles was also added. Phase three: Treatment goals for phase three- improvement of motor function were to decrease impairments in gait by increasing dorsi flexion and to continue with improving previous goals. As for the treatments, sensory stimuli was decreased to just the thermaphore and the room remained darkened during treatments. Assessment included pulse (pre and post treatment), finger focus test, trendelenburg test, ankle PROM, and palpation. Modalities for treatment were still continued the same as previously, however joint mobilizations of the ankle to increase dorsi flexion were included and light joint play to the lumbar spine. Homecare: Homecare throughout the duration of the treatment plan included going on a trampoline for 20-30 minutes, four days a week or as much as possible, going for a walk one time a day as long as tolerated, and balancing on tip toes each night Can massage therapy improve focus, behavior, and motor function in children 22 with developmental disabilities for 5 minutes. Light massage by the parent before bed was also given as homecare. Results The greatest outcomes of this case study included the client’s improvements in both behaviour and focus. The qualitative section of this case study showed very positive results. During phase one, results concluded in: more affection, less grabbing, less scratching, less pinching, and an increase in time of being still during treatment. The first break though in stillness occurred during treatment three with a twelve minute time period of remaining still. This eventually evolved into full treatment focus in phase two and even the ability to fall asleep during the tenth treatment in phase three. Phase one showed an increase in trust and comfort with touch, and beginning changes in behaviour. In the beginning of phase two, the qualitative changes included an increased focus in school, more easily redirected, and more relaxed at home. At this point, changes in routine did affect the client and an example being, when the client went on a weekend trip, poor behaviour increased but only lasted until the next treatment. By treatment five, a significant decrease in rocking behaviour was noticed and had stopped completely by treatment seven. By treatment eight, the Can massage therapy improve focus, behavior, and motor function in children 23 with developmental disabilities rocking behaviour had started again, however, the client had missed a treatment and did not receive massage for twelve days. After the ninth treatment, rocking behaviour had decreased and then stopped completely by treatment ten. Support from the parent guardian was also stopped by treatment six and the patient was able to lie on the table alone for the duration of the treatment. Muscle spasticity had also deceased significantly during phase two. The client began sitting much less rigidly and would sit in a relaxed, cross-legged position while he looked through his books. During phase two, it was also noticed by the speech pathologist that there was an increase in productive vocalizations and an increase in learning ability was recognized by his support group. At this point the client was able to learn how to turn the light switch on and off in a slow, controlled manner and as well, open a door. Education assistants observed an increased interaction with other children at this point. During phase three, qualitative results included the learned ability of using the toilet for the first time without encouragement from a guardian. He was also able to last the duration of treatment at this point without sensory distractions. A weekend trip showed no negative changes in behaviour. Transitions during treatment from one area of the body to another did not affect relaxation. During this phase of treatment, the client also began a new behaviour of tapping lightly with his palms to gain attention rather than hitting or scratching. Can massage therapy improve focus, behavior, and motor function in children 24 with developmental disabilities Other qualitative changes noted during the three months of treatment included learning new skills at home such as: opening cupboards, walking up and down stairs without using the left foot; he would go up and down stairs one foot after the other. There were also no reports of any seizure activity during the whole time period of treatment. As for motor function changes, results were seen throughout all three phases. The postural scan showed slight improvements in head forward posture as the client was less sluggish when standing. Knees were slightly less in genu valgum and hips less coxa valgus due to an increase in hip stability. Pes planus remained the same. The hypertonicity found bilaterally in rectus femoris, biceps femoris long and short head, semimembranosus, semitendinosus, adductor group, triceps surae, peronials, tibialis posterior, flexor halluces longus and brevis, and flexor digitorum longus and brevis had decreased significantly due to the decrease in the rocking behaviour and spasticity. The hypotonicity bilaterally in the gluteus maximus, medius, and minimus along with tibialis anterior, extensor digitorum lonus, extensor digitorum brevis, extensor digitorum longus and brevis, had improved causing an increase in balance and motor function. Range of motion also showed improvements in ankle ROM. Hip and knee ROM were not reassessed as they had full mobility. Refer to table A below for results. Can massage therapy improve focus, behavior, and motor function in children 25 with developmental disabilities Table A-1: Ankle passive ROM ACTION Treatment 4 Treatment 15: pre and post 8 12 60 degrees Treatment 11: pre and post 5 8 degrees 5 8 degrees 60 Dorsi flexion (L) 2 degrees Dorsi flexion (R) 2 degrees Plantar flexion (L) Plantar flexion (R) Inversion (L) Inversion (R) Eversion (L) Eversion (R) 50 degrees 60 60 60 degrees 60 degrees 30 degrees 30 degrees 60 60 30 30 60 60 30 30 8 12 60 The trendelenburg test also showed improvements throughout the course of the study. Refer to table B below for results summary. Can massage therapy improve focus, behavior, and motor function in children 26 with developmental disabilities Table B: Trendelenburg results summary Result Time of Balance Treatment 1 (+) Left (+) Right 0 Treatment 2 (+) Left (+) Right 0 Treatment 3 (+) Left (+) Right 0 Treatment 4 (+) Left (+) Right 0 Treatment 5 (-) Left (-) Right 0 Treatment 6 (-) Left (-) Right 20 sec. (L+R) Treatment 7 (-) Left (-) Right 20 sec.(L) 25 sec (R) Treatment 8 (-) Left (-) Right 12 sec (L) 15 sec (R) Treatment 9 (-) 10 sec (L) 15 sec (R) Treatment 10 (-) 15 sec (L) 12 sec (R) Treatment 11 (-) 15 sec (L) 12 sec (R) Treatment 12 (-) 15 sec (L) 14 sec (R) Treatment 13 (-) 15 sec (L) 12 sec (R) Treatment 14 (-) No results Treatment 15 (-) 23 sec (L) 25 sec (R) (L)=left (R)=right Can massage therapy improve focus, behavior, and motor function in children 27 with developmental disabilities The Elys test provided positive results from treatment. The test was initially found positive however after eight treatments, the test was found negative showing a decrease in hypertonicity of the hip flexors. The results for heart rate before and after treatment also shows a decrease in sympathetic nervous system firing and shows the relaxation that the client was able to achieve. Refer to table C below for summary. Table C- heart rate results Treatment 1 Treatment 2 Treatment 3 Treatment 4 Treatment 5 Treatment 6 Treatment 7 Treatment 8 Treatment 9 Treatment 10 Treatment 11 Treatment 12 Treatment 13 Treatment 14 Treatment 15 Before treatment: beats per minute 90 84 90 78 84 72 78 84 78 78 84 72 72 78 78 After treatment: beats per minute 78 72 72 72 72 66 72 72 72 72 72 66 66 60 78 The finger focus test also showed positive results for the client’s ability to focus. Throughout the treatment schedule the client was able to increasingly focus on the task. The results are summarized below in table D. Can massage therapy improve focus, behavior, and motor function in children 28 with developmental disabilities Table D: Finger Focus test results Treatment 4 Treatment 5 Treatment 6 Treatment 7 Treatment 8 Treatment 9 Treatment 10 Treatment 11 Treatment 12 Treatment 13 Treatment 14 Treatment 15 (L)=left (R)= right Before treatment 2(L) 1(R) 1(L) 2(R) 3(L) 4(R) 4(L) 0(R) 2(L) 1(R) 2(L) 1(R) 2(L) 3(R) 2(L) 3(R) 3(L) 2(R) 2(L) 5(R) 5(L) 5(R) 5(L) 5(R) After treatment 3(L) 4(R) 3(L) 4(R) 5(L) 5(R) 5(L) 5(R) 5(L) 5(R) 5(L) 5(R) 4(L) 5(R) 4(L) 4(R) 5(L) 5(R) 5(L) 5(R) 5(L) 5(R) 5(L) 5(R) Discussion and Conclusion The goals of creating a case study to explore the benefits of massage therapy for children with developmental disabilities to benefit them both physically and mentally were achieved. This case study successfully demonstrates Can massage therapy improve focus, behavior, and motor function in children 29 with developmental disabilities that the benefits of massage therapy were able to increase focus, good behaviour and motor function of a child with Pervasive Development Delay. Throughout the course of the study, the client was able to learn new life skills such as using the toilet, turning a light on and off, opening doors, and even began making more progressive vocalizations. He also became more interactive with other children his age, more affectionate, calmer, demonstrated less aggressive behaviour, and completely stopped his rocking behaviour (which was thought to be a behaviour of anxiety). The client also became less affected by changes to routine. By the end of the study, the client was able to go on a weekend trip without having negative affects to behaviour or focus. He was even able to have his education assistant assist him during a treatment instead of his parent guardian. Relaxation also showed to improve in the treatment room. In the initial treatment, the client could barely remain still throughout the entire session and by treatment thirteen, the client remained completely still and even fell asleep during last thirty minutes. As for the major health concerns of seizure activity, there were none to report since massage therapy began, however, the clients medications were increased five months previous to treatment so that could be a major component to the lack of seizure activity. The client demonstrated positive motor function changes in gait, posture, ability to go up and down stairs, balance, and general muscle tone. Although it was challenging to perform a lot of tests properly due to the mental status of the Can massage therapy improve focus, behavior, and motor function in children 30 with developmental disabilities client, the tests that were performed did show improvements. Gait appeared much less sluggish as well as posture, balance increased, muscle spasticity decreased, and weak muscles became stronger (hip abductors in trendelenburg test). By the end of the study, the client was able to walk up and down stairs without using the left foot as the lead; he was able to go up and down properly. The client’s parent guardian expressed the changes noticed since the study began, “Any changes I have noticed in behavior, focus, energy level, postural differences, and differences in spacticity: - Overall, my son is much more calm and focused (observation by me, EAs, and after-school support worker). He is not fidgeting as much, and is more likely to engage in activity when his fidget (i.e., shoelaces) are not readily accessible. He is going more frequently without his shoelaces, and has not had any escalations associated with this change. - He pays much more attention to what the other kids are doing in the playground, and initiates contact (e.g., approaches them, wants to touch them). - He is taking stairs – going from left foot to right to left, etc rather than using same foot to go up stairs). - More communicative, vocalizing. - Seldom rocking or crossing legs in rigid pose any more. Was doing that several times per day prior to massage. Before, when we would uncross his Can massage therapy improve focus, behavior, and motor function in children 31 with developmental disabilities legs, he would move them back to that rigid pose; now when he does this and we move his legs, he does not cross them again. - He appears a lot less aggressive. - Requests music; copies movements to songs (both hand gestures – tapping or clapping – and awkward dance moves). - Loves to twirl around now. His balance appears to have improved. He can lift both legs much higher than he used to, and hold them above the ground for a longer time.” The client’s education assisstent would note another insight to the changes experienced. She mentioned, “I believe that he is more calm and focused after massage. In the sensory room, we have been doing lots of sighing and I must say that he is sustaining joint attention during action songs for a longer time (this is a perceptual observation as I never time his attention time)”. Due to the small body of research on manual therapies such as massage for children with PDD and autism spectrum disorders, as well and the complexity and wide spectrum of how they can present, it is challenging to draw a solid conclusion that the results of this case study can be transferred to other developing children with these disorders. Due to the profound results in this particular case study, it would be of great benefit to continue research on how massage therapy can benefit these children. Can massage therapy improve focus, behavior, and motor function in children 32 with developmental disabilities References Baird, G., Charman, T., Cox, A., Baron-Cohen, S., Swettenham, J., Wheelwright, S., & Drew, A. (2001). Screening and surveillance for autism and pervasive developmental disorders. Archives of Disease in Childhood, 84(6), 468-475. Centers for disease control and prevention. N.p., 26 Dec. 2013. Web. 17 Dec. 2014. http://www.cdc.gov/ncbddd/developmentaldisabilities/facts.html Chasnoff, Ira J. "To sleep.a parent's dream." Psychology Today (2011). Web. 28 Dec. 2014. http://www.psychologytoday.com/blog/aristotles-child/201107/sleepaparents-dream Escalona, A., Field, T., Singer-Strunck, R., Cullen, C., & Hartshorn, K. (2001). Brief report: improvements in the behavior of children with autism following massage therapy. Journal of autism and developmental disorders, 31(5), 513-516 Hernandez‐Reif, M., Field, T., Largie, S., Mora, D., Bornstein, J., & Waldman, R. (2006). Children with Down syndrome improved in motor functioning and muscle tone following massage therapy. Early child development and care,176(3-4), 395410. Ludwig, L. & Rattray, F. (2000). Clinical massage therapy: Understanding assessing and treating over 70 conditions. Elora, Ont.: Talus Incorporated. Magee, D.J. (2008). Orthopedic physical assessment (5th ed.). St. Louis, MO: Saunders . Can massage therapy improve focus, behavior, and motor function in children 33 with developmental disabilities Appendix Appendix A- health history form Can massage therapy improve focus, behavior, and motor function in children 34 with developmental disabilities Appendix B: treatment forms