Methods of reducing the waiting list for renal transplants in Scotland
advertisement

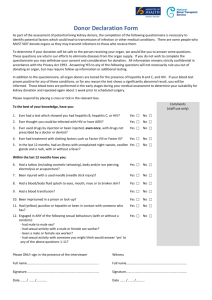
Methods of reducing the waiting list for renal transplants in Scotland and the UK Aims To consider: The assessment criteria of kidneys from deceased donors and whether this criteria should be broadened to maximise the use of donated kidneys. Methods of matching donor kidney quality with patient predicted survival to reduce death with graft function. The effects of factors on the outcomes of living kidney donor transplantation on living donors and recipients to increase the number of successful transplants. Models of organ donation used in other countries, and whether they could be applied in the UK and Scotland to reduce waiting times. The most effective methods for approaching relatives of deceased donors to gain consent for organ donation. Reasons behind the disparity in organ donation rates among different ethnic groups and strategies which could be implemented to resolve lower rates among ethnic minorities. Methods of living kidney transplantation including kidney paired donation. "England donor cards, 1971-1981" by Science Museum, London, Wellcome Images is licensed under CC by 4.0 This site was made by a group of University of Edinburgh medical students (see contributions) who studied this subject over 10 weeks as part of the SSC (SSC web pages). This website has not been peer reviewed. We certify that this website is our own work and that we have authorisation to use all the content (e.g. figures / images) used in this website We would like to thank Dr Paul Phelan and Dr Eoin O'Sullivan for their guidance throughout this project. Total word count: 10,612 Word count minus Contributions page, References page, Critical Appraisal Appendix, Information Search Report and Word Version appendix: 5,907 Header photo from the 20th U.S. edition of Gray's Anatomy of the Human Body, originally published in 1918 and therefore lapsed into the public domain. Gray1121. Next> Introduction Over the past 24 years 15,480 patients, who have developed Endstage renal disease (ESRD), have been registered to the Scottish Renal registry (SRR)1 -of which 10,613 are now deceased. These figures are a microcosm of the severity of the problem not only seen in Scotland, but also globally such as in the USA where waiting times can exceed 5 years2. The donation of kidneys has two possible sources: living and deceased donors. Within Scotland, there has been no net increase in the number of deceased donors since 1993 as can be seen from the graph below. This is despite an increase of those starting Renal Replacement Therapy by 56% over the same 20 year period. However, living donations have continued to increase since the inception of records in 19601. A bar chart showing the frequency and donor type for kidney transplants in Scotland between 1960 and 2011. (CLICK TO ENLARGE). Source: ISD Scotland. Available from: http://www.srr.scot.nhs.uk/Publications/PDF/scottish-renal-registry-report-2013web.pdf?2 (Page 29) Different countries have tried different methods to increase their source of kidneys with varying success. These methods can be studied to highlight potential strategies to improve kidney donation rates in Scotland and the UK. Spain has been internationally singled out as having an extremely successful deceased donor program for organ retrieval3. There are also a number of ideas to increase living donor donation, such as “dominos”4, which aim to further increase the number of viable kidneys for transplant. Kidneys from living donors offer significant advantages such as better results and less aggressive immunosuppressive courses following transplantation5. By maximising the number of transplants, people can be taken off dialysis sooner. This increases both the life expectancy and the quality of life of the patient6, which highlights the importance of striving to improve the number of kidneys donated and the project we have chosen. In addition to increasing donation rates, the criteria used to match donors and recipients could be more effective. This would prevent the wasting of possibly viable kidneys for transplant, as well as matching kidneys to suitable recipients, to reduce the likelihood of returning to the waiting list. By examining the various methods of how the organ transplantation system works within a variety of healthcare settings, we can assess their benefits and drawbacks. We also assess if they would be successful in increasing the number of renal transplants within Scotland and the UK. < Previous Next> Criteria involved in kidney transplantation from deceased donors Deceased donor kidneys are either from donation after brain-stem death (DBD) or donation after circulatory death (DCD). DBD refers to donors who are pronounced dead using neurological criteria generally in an Intensive Care Unit; cardiac circulation and ventilation is maintained by medical intervention1. DCD describes organ retrieval following death due to heart or circulatory failure. DCD is becoming more common, and has attributed to the 11% increase in deceased donor renal transplantation in 2013-142. DCD kidneys are associated with a greater risk of delayed graft function (the need for dialysis within the first week posttransplantation) and primary non-function, making them suboptimal3. However, they show little difference in 5-year patient and allograft survival compared with DBD kidneys and importantly, increases the donor pool1. Furthermore, donor kidneys are assessed by quality and are categorized as standard-criteria donors (SCDs) or expanded-criteria donors (ECDs). ECDs refer to donors over 60 years of age or aged 50-59 with two of the following features: history of hypertension, terminal serum creatinine >1.5mg/dl (indicating renal insufficiency) or death via cerebrovascular cause. These characteristics indicate a 70% greater risk of graft failure compared to SCD kidneys 1. SCD kidneys have none of the characteristics of ECD kidneys and are from DBD only. The ECD category indicates the significance of factors, such as donor age and comorbidities, on the clinical outcomes of renal transplantation such as acute rejection, delayed graft function and patient and allograft survival1. Other key donor kidney assessments include HLA typing (of HLA-A, B and DR antigens), blood group matching and serology tests for presence of transmissible infections such as HIV or Hepatitis C. In the UK, allocation of kidneys is based on points system for patient waiting time, HLA matching and sensitization3. However, investigations of suboptimal kidney transplantation suggest scope for broadening the criteria. Every year in the UK many available deceased donor kidneys are rejected despite critical demand4. Age is a key reason for kidney discard. Kidneys from donors over 65 years have a higher risk of graft loss and mortality, and there is generally a longer cold ischemic time. The likelihood of comorbidities and obesity is generally higher in kidneys of aged donors, reducing the quality of the kidney4. However, research shows that short-term graft survival is similar to that of younger organs, and there are improvements to the recipient's quality of life compared with remaining on dialysis. Of particular note, the study by Chavalitdhamrong et al concluded that the relative risk of patient death was less when older ECD kidneys were transplanted into recipients over 60 years, compared with younger recipients 5. This retrospective cohort study had a relatively large sample size so the likelihood of chance affecting the results is limited. However, the follow up period was short (5 years) so long term outcomes remain to be seen. The study suggests that transplantation of older kidneys could have better outcomes if recipient age parameters were adopted; further supported by other research6. This use of elderly donor organs can be seen in Spain, a country well recognised for its successful organ transplant system, where 40% of total renal transplants are from donors aged over 60 years3. The presence of active HIV disease is a contraindication for renal transplantation in the UK3. Recent research into the use of HIV+ donor kidneys has shown promising outcomes of good short-term patient and allograft survival7. Given that appropriate tests are carried out, the recipients would face no additional risks. A South African study showed HIV+ donor kidneys transplanted into HIV+ recipients resulted in good graft function and no need for dialysis at 12 months8. Current classifications of “suboptimal” kidneys may be too restrictive; Hwang et al. found that long-term differences in patient and graft survival and mean glomerular filtration rate between grafts from ECD and SCD transplants were not statistically significant9. Although the incidence of delayed graft function was significantly higher in ECD kidneys, this was not a risk factor for graft survival in a multivariate model. However, the study was conducted at a single centre so it may not be widely representative. In conclusion, further development of approaches to modify and broaden listing criteria will help to reduce organ shortage and waiting list mortality, and also improve long-term outcomes after transplantation. < Previous Next> Matching kidney quality to patients' predicted survival rates Maximising the use of each kidney donated can reduce the waiting list for kidney transplants so patients either return to the list at a later date or do not return at all. To do this measures must be taken to prevent death with graft function (DWGF) which is one of the ways in which a transplanted kidney can fail- one study reported DWGF to account for 42.5% of all graft loss1. This study highlighted two other studies with similar findings reinforcing its reliability. DWGF could be reduced by matching better quality kidneys with patients that have a better survival prospect for the future. For example, consider there are two patients, one with a much higher life expectancy than the other and two kidneys, one of which is in a much better condition. The kidneys are allocated randomly, and the patient with the lower life expectancy, by chance, receives the kidney in the better condition. He subsequently dies with graft function and the second patient outlives his kidney and has to be added to the waiting list for a second kidney, increasing the list’s size. Whereas, if the first patient had received the worse kidney, they would have died at a similar point to that when the graft failed and the second patient would have had his kidney for longer and potentially not had to go on to the waiting list again. To carry out this matching process there has to be a way of categorising kidney quality which is affected by the criteria mentioned in the previous section and also a method of categorising recipients in relation to their survival prospects. A potential classification is the Kidney Donor Risk Index (KDRI). It uses ten donor factors to predict failure of graft function which include age, height, weight, ethnicity, history of hypertension or diabetes, cause of death, serum creatinine, hepatitis C serology and donation after cardiac death 2 . The study to determine these factors was carried out on a large population of 69,440 patients which reduced the influence of chance. The study also used stratification in the statistics to minimise the impact of confounding. The KDRI can then be used to generate the Kidney Donor Profile Index (KDPI) which is the KDRI of a kidney relative to a reference point which is the median donor of the year before3. The KDPI is an improved scale as it uses more variables to make a more accurate assessment and it separates the kidneys into percentiles to allow for better matching. On the other hand, it still is not a perfect system as it does not take into account all factors which have an influence on the length of time of graft function, such as trauma to the kidney and HLA mismatches. The KDPI system can therefore not be used independently. Recipients also have to be assessed for their likely long-term survival to determine whether they are suitable. One quantification of survival is the Estimated-Post Transplant Survival score (EPTS). This score is based upon the candidates age, dialysis duration, prior solid organ transplant and diabetes status4. An example of the patient matching is that those in the top 20th percentile EPTS score are given kidneys with a KDPI of less than 20%. When using KDPI and EPTS to match kidneys to patients in the US it was simulated to result in an increase in the average projected median lifespan after transplantation and would increase the time spent with a functional allograft4. For 11,000 transplants, the prediction was that there would be an increase of 9,130 life-years of patient survival and 2,750 years of allograft survival. In conclusion, the KDRI and KDPI is a possible method of quantifying the quality of kidneys being donated. Along with the EPTS for classifying potential candidates there can be appropriate longevity matching, meaning that fewer kidneys would fail due to death with a functional graft. This could therefore be used in Scotland and the UK as a method of maximizing longevity of the allograft for an individual patient and increasing utility of the transplant on a societal level. < Previous Next> Living kidney donation Living kidney donor transplantation (LKDT) offers superior patient outcomes compared with deceased donor kidney transplantation and allows a wider range of patients to receive and benefit from a kidney transplant. It is a highly progressive area of donation and transplantation, having trebled in number from 2000 to 2010 and increased by 4% from 2013-20141 in the UK. There is potential to increase the number of donors and recipients viable for LKDT. The reduced risk of allograft failure from LKDT prevents the wasting of donated kidneys, contributing to decreasing the demand of organs and waiting times. The development of expertise in immunology and blood group matching has enabled planned LKDT to be a treatment of choice for complex recipients. A single-centre study evaluated rates of survival after LKDT in 211 consecutive patients with donorspecific anti-HLA antibody after undergoing desensitisation. The study concluded that this provided a significant survival benefit compared with matched control subjects who were waiting for a compatible kidney2. However, one limitation is that the follow up time was less than 3 years for half of the patients. A US study comparing patients who underwent live-donor ABO incompatible (ABOi) transplantation with ABO compatible-matched controls concluded there is long-term patient and graft survival for ABOi recipients; confounding factors may have affected the results3. These factors can expand the number of suitable patients for kidney transplants, decreasing the waiting times for organ transplantation. It is vital donors are informed of the potential health risks of donation to ensure their welfare and safety is protected. Two prospective studies in the US4 and Norway5, with large cohorts, compared the risk of living donors developing ESRD after donation with nondonors. The general population is unscreened and are at a much higher risk of developing end-stage renal disease (ESRD) than living donors, who are free of contraindications before donation. Therefore, healthy cohorts of nondonors with an equally low risk of renal disease and free of contraindications to live donation were used to avoid unreliable comparisons. Both studies concluded that kidney donors had a small increased risk of developing ESRD compared with the matched healthy donors. The presence of a potential genetic predisposition to kidney disease among related donors may have caused bias in the results. A retrospective, matched-cohort study in Canada compared the risk of gestational hypertension and preeclampsia in living kidney donors and nondonors, concluding it is more likely to be diagnosed in donors, although the risk of serious maternal and foetal outcomes remain low. This study may have been distorted by racial information not recorded, a factor which contributes to the risk of hypertension6. Although there are associated risks for living donors, they are likely to be outweighed by the benefits of LKDT when a potential living donor is considering donation. One study investigated the psychological impact of donation on the donor and found the donors showed positive perceptions about donation with a decrease in depression scores7. Only biologically related living donors were studied and therefore it is not representative for living unrelated donors. Increasing the awareness of the small magnitude of risks involved with LKDT may encourage potential living donors to consider donation. The introduction of laparoscopic living donor nephrectomy (LLDN) in 1991 is believed to have had a causal effect on the increase in LKDT, now the standard approach for donor nephrectomies across the world8. Studies have found an association of LLDN with a reduction in the size of incision, length of hospital stay and magnitude of convalescence9. This reduces the surgical risks to the living donor, a possible deterrent to donation. A retrospective matched-pair comparison between LLDN and laparo-endoscopic single site surgery (LESS) suggested a possible association between quicker convalescence and LESS donor nephrectomy10. This could encourage an increase in living donors. Due to a limitation in time, only single-centre studies on the effect of surgical techniques on living donor motivation have been conducted. Advancements in surgical technique of nephrectomies could improve prognosis for donors and encourage an increase in donors. Considering the effects of factors on the outcomes of LKDT for living donors and recipients is vital to maximise the number of successful LKDT. Further research and advancements into the recruitment of living donors can increase the number of LKDTs, contributing to the donor pool and decreasing the waiting list. < Previous Next> Models of organ donation The current model for Scotland is an opt-in system requiring consent from relatives for organ donation to occur. There is a Specialist Nurse for organ donation in some centres to coordinate the process, however, asking for consent primarily is by physicians1. Every current model for organ donation has its advantages and disadvantages and the Spanish model is upheld as an exemplary model world-wide for deceased donor donation with a kidney transplant rate of 46.3 per million population (pmp) compared to a UK rate of 34.2 pmp in 20132. The Spanish model has achieved such high rates through a proactive approach performed by welltrained transplant coordinators working at a national, regional and hospital level, using a “soft” opt-out system where families must give consent3. The opt-out system is sometimes presented as the reason for higher donation rates in Spain, but the requirement for consent from families cannot allow this conclusion to be drawn4. This integrated approach has been aided by adequate management of mass media relations which has helped to create a positive social atmosphere. This has been key to the success of the Spanish model as it enables the transplant teams to openly discuss organ donation with families, leading to low levels of refusal (15.9%) compared to the high rate of refusal in Scotland (40%)5. Creating an atmosphere where talking about organ donation is normal is essential to achieving a higher rate of organ donation in Scotland. A diagram showing the variation in rates of kidney transplants from deceased donors across Europe (CLICK TO ENLARGE). Altered from an image on Wikimedia Commons by Michael Bennett with data from the International Transplant Newsletter(2). Original image is licensed under the CC Attribution-Share Alike 3.0 Unported license. Similarly, the American model for organ donation exemplifies the importance of a proactive approach, with Organ Procurement Organisations actively seeking consent. The ‘Required Request’ system makes it illegal, immoral and irresponsible to turn off ventilatory support without considering organs for donation6. However, these Organisations are not as successful as the Spanish Model because the Organisations are external to hospitals, and so there is an absence of in-hospital coordinators; even small Spanish hospitals have a coordinator in house 7. This highlights the need also for an integrative approach with responsibility given at each level. As mentioned previously, the opt-out system is unlikely to be the sole reason for Spain’s success, however Austria have a ‘harder’ form of presumed consent. In Austria, organ recovery is standard unless an objection was made by the patient or family before death which resulted in a 5 fold increase in organ donation over 5 years8. While such systems have had some increase in overall organ donation rates, they haven’t been nearly as successful as Spain. However, there exist worries that this 'harder' model could polarise public opinion, be ethically impermissible or even be open to successful legal challenge4. The Iranian model uses paid living donation which has resulted in the renal waiting list being entirely eliminated. A paper by Ghods explores the model’s significant ethical implications9.The author helped develop the model which may have skewed the paper toward the benefits of the system. One of the successes is that organ donation has been available irrespective of income. This is done through government funding of treatments, gifts from wealthy recipients, or charities where the recipient is poor. Donors are also provided with life-long health insurance after donation. One of the ethical problems is that 84% of donors are poor. Despite this over half the recipients are also poor, and commercial transplantation is prohibited which would open the system to abuse poorer donors. While this model has been successful at eliminating the waiting list in Iran, implementing these changes in the UK for ethical purposes would be challenging. Reimbursing any expenses from donation is recommended by the WHO and currently takes place in the UK10. <Previous Next> Methods to improve familial consent rates in a clinical setting One of the greatest challenges facing organ shortages is relative consent rates where medical professionals ask for consent. Over 4 in 10 families in the UK refuse consent for organ donation, one of the highest rates world-wide, and improving this rate is seen as imperative to shortening the waiting list in Scotland1. Studies have examined factors which influence rates of donation. A qualitative study by Sanner found that only physicians with a prodonation approach to organ donation were able to achieve consent2. This study had a novel method combining both narratives of relatives and physicians which was particularly strong, however, a small sample size may make it unrepresentative. This was consistent with a larger study by Djong et. al. which showed that if the benefits of organ donation were made aware to families (prodonation), a much higher rate of consent was achieved (68 to 92%)3. Other studies4,5 showed that higher rates of consent were achieved when relatives felt they were given enough information. However, these studies may have had a confounding factor; where consent was refused, it would be unlikely for further information to be given. Sanner also found that a non-donation response was a ‘nondecision’ – a way of avoiding having to make a decision in a time of grief2. Another qualitative paper in 2014 concluded “inviting them [relatives] to reconsider their initial refusal will lead to a more stable decision6.” Other studies followed similar themes with consent rates being significantly increased if death and organ donation are decoupled3,7,8,9. All these studies were retrospective and observational so they are unable to find causative data, only associations. The study by Niles et al. had particularly interesting results, showing consent rates were highest (62%) if the family was asked before death, as opposed to at the time of death (25%). Ensuring donation is requested at the correct time and inviting patients to reconsider a no-response should improve consent rates. Ensuring brain stem criteria of death is understood by relatives is essential for achieving high rates of consent as found by DeJong, Rodrigue and Jenkins with increases of 20%, 31% and 27% respectively when comparing families who understood brain death compared to those who didn’t3,6,10. Once again all three were retrospective but all methods of the studies were rigorous with medium sample sizes. Lastly, the person who asks for consent greatly influences the refusal rate, particularly their training level. A Norwegian study found a severe deficit in training in especially with communication with over half reporting difficulty relating to relatives. Many also failed to adhere to recommended practice which led to lower consent rates11. In the UK the only form of training given is a DVD. A further study of 1,137 relatives found that when trained organ procurement specialists approached relatives there was a 69% consent rate compared to a physician consent rate of 49%12. Introducing a Specialist Nurse for Organ Donation (SNOD) with relevant training would improve consent rates. The study also showed that use of translators reduced the consent rate, but a confounding factor (ethnic minorities are less likely to donate) may explain this. In conclusion, ensuring doctors asking for consent have a prodonation attitude, who are highly trained in obtaining consent would improve consent rates. Training should be given on how to approach relatives decoupling the death and organ donation, giving adequate information to relatives of patients about brain stem death and ensuring enough time is given to relatives to come to a decision. We would also recommend allowing patients to reconsider their decision (avoiding the premature ‘No’) and the introduction of a SN-OD in every hospital so potential donors are not missed. < Previous Next> Variation in rates of organ donation between different ethnic groups and how they could be improved In the UK, it is estimated that 10.8% of the population are from Black, Asian and Minority Ethnic (BAME) communities1. However, they represent 27% of those on the waiting list and only 5% of organ donors2. The under-representation of organ donors is partly due to higher refusal rates when consent is required for relative’s organs – 66% among BAME families compared to 43% for the rest of the population3. Variation in organ donation is further highlighted by a large prospective cohort study in the UK which found that white patients who died in a critical care setting were more than 5 times more likely to become kidney donors than Asian patients4. The reason for these differences is not due to one specific barrier but rather due to wider negative attitudes to organ donation caused by multiple problems. These include: distrust (for example worries that the organs may be used for medical research), the feeling that registering as a donor is like ‘tempting fate’, concern that medical teams will not try as hard to save their life, and many others 5,6. While these concerns are significantly greater among ethnic minorities, they are also expressed to a lesser degree by the White population5. Therefore addressing these barriers would increase donation rates across all ethnic groups. However, it is important to note that one of the studies cited (5) was conducted in South London – an ethnically mixed area with high levels of social disadvantage and unemployment. This is a possible source of confounding as there is evidence suggesting that the negative attitudes of disadvantaged ethnic minorities are a result of feelings of marginalisation and lack of belonging7,8. In areas such as South London it may therefore be necessary to address these underlying feelings alongside the issues that have been identified such as trust. Interestingly, a common barrier to organ donation among ethnic minorities is the feeling that it is against their religion5. This is despite the fact that there are no religious faiths which object completely to organ donation, but rather see it as an individual choice9,10. This means that with suitable interventions and work at the local level within the community, it should be possible to eliminate any variations in organ donation which are due to religion. Lastly, there have been many studies which have found ethnic minorities to be significantly less willing to discuss organ donation with family members5,11. Discussion within the family is very important as family consent rates are much higher when a preference for organ donation is known12,13. This may partly explain the higher refusal rates in BAME families as discussed previously. In conclusion, the lower donation rates among BAME communities are a result of many different issues and not one major barrier. Reflecting this, while there may be no one easy solution, each issue could be addressed individually. For example, encouraging family discussion to reduce refusal rates or engaging people in the community to help reduce feelings of marginalisation are simple measures which could have big impacts. Furthermore, staff requesting organ donation must be familiar with different cultural and religious views regarding death so that they can more appropriately approach discussion with families and thus increase consent rates14. Almost all of the barriers which affect ethnic minorities also affect the White population and so addressing them will be beneficial in increasing organ donation rates across all ethnic groups. < Previous Next> Methods of kidney paired donation Kidney paired donation (KPD) is a promising area for maximising the number of kidney transplants from living donors and reducing waiting lists. The predicted success of implementing KPD is influenced by factors including the organ pool size, geography, and further logistics. As a result, investigation into the practicalities of participating in KPD and whether it can be applied in Scotland is necessary. The main methods of KPD are paired exchanges, domino-paired donation (DPD), and non-simultaneous extended altruistic donor (NEAD) chains. Paired exchange is the simplest method. Two incompatible pairs are invited to exchange organs, with donor A donating to recipient B and vice versa1. It allows patients who have a willing but incompatible donor a shorter waiting time and a guaranteed living donor transplant (LDT)2. The practicality of paired exchange is influenced by geographical barriers. In many situations both pairs will live in different locations and asking donors to travel to recipients’ transplant centres would impose financial and social difficulties3. Another option is to transport the kidney. Simpkins et al researched the effect of cold ischaemic time (CIT) on the outcome of LDTs via a retrospective cohort study of 56,341 recipients. A 4.3% increase was seen in DGF but no significant impact was found on long-term outcomes with CITs <8 hours4. The study’s reliability was increased by using a large sample to minimise chance. However, confounding may influence the results due to use of different surgical procedures, which could affect transplant outcomes. In DPD a non-directed donor (NDD) donates a kidney to an incompatible pair. The donor of the first pair goes on to donate to another incompatible pair or a patient on the waiting list1. Thus at least two transplants can be achieved through one altruistic donor’s gift. A study found, on average, a 20% increase in the number of transplants facilitated when NDDs participated in DPD/NEAD chains, compared to NDDs donating to patients on the deceased donor waiting list5. A mathematical model was used with simulated rather than actual donor-recipient data which reduced validity. Although taking into account factors including varying rates of reneging when analysing the results does improve its reliability. Diagram illustrating the steps of domino paired donation (DPD) NEAD chains are similar to DPD but occur on a larger scale, facilitating more transplants. A chain is initiated by a NDD donating to an incompatible pair, there is no donating to the waiting list. Therefore, the chain can expand exponentially. In contrast to the previous methods the transplants are not carried out simultaneously, instead chains take place as matches are found. The final donor in the chain is reserved as a ‘bridge donor’ to restart the chain at a later date rather than donating to the waiting list, as in DPD1. This introduces a greater risk of reneging as the bridge donor may not be contacted to donate their organ for months after the other half of their pair has received a transplant5. In 2012 the UK created a National Living Donor Kidney Sharing Scheme. Within this scheme paired exchanges and DPDs are performed. Compatible pairs seeking an improved match are also eligible to participate. Matching runs are carried out quarterly to detect possible exchanges amongst registered candidates. During 2013-2014, 10 paired exchanges took place in Scotland and 62 in the rest of the UK. An increase from 4 and 51 respectively in 201220136. Research has shown that larger pool sizes correlate with increased transplant rates and improved matches7. Therefore, national KPD programs are estimated to be more beneficial than single-centre schemes. Eurotransplant is the organisation which coordinates the allocation of organs in eight European countries, excluding the UK8. Consequently, the pool size is expanded leading to more transplants. Scotland could benefit from registering with Eurotransplant due to the limited population size. At present, Eurotransplant only utilises deceased donors and has potential to improve transplant rates by introducing KPD. For example, the US launched a KPD Pilot Program (KPDPP) in 2010, with 61% of US kidney transplant programs signing up. However, the pool mainly consists of ‘hard-to-match’ pairs, including highlysensitised recipients9. For KPDPP to be successful, every US transplant program must participate and be willing to register all of their incompatible pairs, not only those who are ‘hard-to-match’. In conclusion, the UK’s KPD program is still in the early stages of development, but has great potential based on the success of similar schemes in other countries. With appropriate planning and infrastructure a European KPD scheme could be implemented. Therefore, increasing the pool size to maximise the number of LDTs, improve quality of matches, and decrease waiting times. < Previous Next> Conclusion Many ideas have been explored throughout this literature analysis of different methods to reduce waiting times for kidney transplantation. Some ideas have been extremely successful in their unique healthcare setting, such as in Iran where people are paid for their organs1 . There are many ethical and moral issues that mean that it would be challenging to implement this method within Scotland although reimbursement of medical expenses should be to reduce economic barriers to patients receiving a transplant. Providing training for medical professionals or creating a specific role within the NHS, such as transplant coordinators used in Spain2, would enable an empathetic approach providing clear explanations to families with relatives who could possibly become donors. This training could also be applicable to living donors and with our increasing understanding of the effects of living donation to the donor, medical professionals can provide accurate and reliable information helping the potential donor to make an informed decision3. Both of these methods would help to increase the number of available kidneys, subsequently reducing the waiting list by increasing familial consent rates for deceased donors and increasing the number of living donors. Training should also address the different approaches of cultural and religious groups to death, which would help medical professionals, reassure these groups and gain consent4. An opt-out rather than the current opt-in system may seem like a quick fix, however, without the appropriate training of professionals and changing the current perceptions about organ donation within the public this would ultimately be unsuccessful. Kidney paired donation allows for the utilisation of willing but incompatible donors, such as in the situation where a family member wants to donate to a relative but is not a match6. Looking to join a larger paired donation network could increase the likelihood of people receiving transplants. This may be difficult to create on a large scale7, due to geographical restrictions8, but the concept should be explored. Adequate matching of a kidney’s Kidney Donor Profile Index to a recipient’s Estimated-Post Transplant Survival score could maximise the use of each kidney, which would reduce the rate of recipients returning to the waiting list, which has begun to be used within the USA9. A possible area we could have examined is ways in which to prevent graft failure once the kidneys has been transplanted. Clinical medicine is still continuing to understand what causes graft failure within recipients9, so as our understanding changes our approach will too change. Our project aimed to establish changes to the system itself, which will hopefully create changes on a permanent basis. It would be beneficial for further prospective studies to be conducted to explore various ways of obtaining consent to reduce bias and confounding factors. This could allow for the creation of a standardised and effective method of gaining consent from families. The long term effects of having an extended criteria kidney could also be further investigated as current studies have short-term follow-ups. Overall our project has demonstrated how contrasting countries approaches are to kidney donation and transplantation, emphasising how there is no single solution to this problem. By instigating changes at a national, regional and hospital level then the changes can be extensive and thorough. By using a combination of several methods, a complete and holistic approach to this issue can be created and this will aid in reducing the waiting list for renal transplant within Scotland and the UK. <Previous Contributions Michael Bennett researched the current model of organ donation in Scotland and statistics relating to the current state. He also wrote the introduction and conclusion. He further organised the critical appraisal. Alisha Khanna researched current criteria for kidney donation, particularly for kidneys from deceased donors. She wrote the section on criteria for deceased donor transplantation. She also organised the meetings with our tutor on behalf of the group. Mark McBrien researched KDPI. He wrote the section on Matching kidneys’ predicted graft survival rates to patients’ predicted survival rates. He further compiled everyone's pages and was involved in formatting the webpage and the word version appendix. Sarah Atkinson wrote the section on living kidney donation. She researched living kidney donation and factors that effect the outcomes of livedonor kidney transplantation on donors and recipients. Jordan Fitzpatrick researched models of organ donation and collaborated with Nicklas Brown in writing the Models section. He further researched and wrote about reasons Ethnic minorities are less likely to be donors. He also verified copyright permission for and inserted the bar graph in the introduction. Nicklas Brown researched models of organ donation and collaborated with Jordan Fitzpatrick in writing the Models section. He further researched and wrote about methods to improve consent rates in a clinical setting. He organised the contributions page and the search report. Sarah Jack researched kidney paired donation and living donor pools. She wrote about ways these could be implemented in the UK and Scotland. Sarah also produced a diagram explaining domino paired donation. Critical Appraisal> Critical Appraisal In the past examination of the risk to living kidney donors of developing End-Stage Renal Disease (ESRD) has been examined against the risk to the general population. The general population offers an unsuitable comparison as they are unscreened and many morbidities are present which make them unable to donate. This study aims to compare the risk of ESRD in those which have donated against those that could have donated but did not. The cohort study used a sample of 96,217 Kidney donors; every live kidney donor from 1994-2011 in the USA. The non-donors were selected from Third National Health and Nutrition Examination Survey (NHANES III), of which there were 9,364 participants that had no contraindications to living kidney donation and could have been live kidney donors. The large sample size makes the results arising by chance less likely. Using every kidney donor in the USA from 1994-2011 makes it representative of the entire population. The study used statistical analysis with significant p values and 95% confidence intervals, acknowledging chance could exist. The NHANES lll study was carried out from 1988-1994. It is possible that non-donors might experience a higher rate of ESRD if taken from a modern sample, as the general rate of ESRD has increased since this survey. It could be argued, however, that this rate is within the general population. As this cohort is considered to be healthier than the general population it is quite possible that the relative risk has not increased, making this survey and these people still applicable. Those that donated kidneys, at the time of donation, had a higher BMI, systolic blood pressure and the chance of them being smokers was twice as likely. This could lead to confounding, as these factors are associated with an increased risk of developing ESRD. The majority of the cases where ESRD developed in donors occurred in transplants between relatives. The cause of ESRD in the donors and non-donors is absent in this study. If the cause is immunological, then there is a possibility of a genetic factor which would lead to a greater predisposition to developing ESRD and once again confounding. A wide range of clinical variables were taken into account and each cohort was matched by age, sex, race, educational status, BMI, blood pressure and smoking history. This reduces the risk of confounding and allows for a causal link to be established. The study followed each group for a maximum of 15 years. A longer follow up period would allow for a more comprehensive understanding of the long term prognosis, although 15 years gives a good idea of problems. In younger donors the issues that arise after the follow up period may not be seen until many years afterwards. The large sample sizes allows for more confident inferences to be made, especially that surrounding race and ethnicity. It also allows for the production of an estimated lifetime risk for ESRD for donors and non-donors. Overall this report is of good scientific quality despite issues of confounding, bias and chance addressed earlier. The study has a large sample size which is taken from across the USA, making it very representative and useful within this area, although it may not be applicable to other nations due to cultural and healthcare differences. Continuing to monitor these populations will help to ascertain more accurate results. This study offers improvements over past studies as it uses a better comparison than the unscreened general population and reaffirms existing knowledge. This allows for doctors to give evidence-based information to patients which will importantly aid in informed decision making. < Contributions Information Search Report> Information Search Report Recognising the information gap: After our initial meeting we individually researched an area involved with kidney donation and fed back to the group our research in that given area. In addition we received papers by our tutors which helped us direct our searches. This allowed us to gauge the literature depth and breadth in various areas of organ donation. Distinguishing ways of addressing the information gap: We initially used google scholar and review articles to find research papers. This allowed us to form the areas which we wished to develop further which led to the titles of our main sections based on what was missing in the UK with organ donation. Constructing strategies for locating the information: Having established the 7 topic areas we wished to research we used bibliographic databases (e.g. PubMed) to search for relevant literature on our chosen topics. Using keywords related to the respective sections and using AND or OR, let us narrow down our searches to relevant information. Locating and accessing the information: Often databases such as PubMed only provided abstracts to papers. Using institutional access we followed links to other sites with full papers on them. Otherwise using Edinburgh University library we were able to find most papers. Most members of the group used Mendeley to save relevant PDF files they had found for future reference and for writing their sections. < Critical Appraisal References> References Introduction 1. National Health Service Scotland, Scottish Renal Registry Report 2013 (2013). http://www.srr.scot.nhs.uk/Publications/PDF/scottishrenal-registry-report-2013-web.pdf?2 (Online Publication). This publication used data from all kidney transplants in Scotland from 1960, which allows the data collected to be both comprehensive and representative of Scotland. 2. Davis A, Mehrotra S, McElroy L, Friedewald J, Skaro A, Lapin B, Kang R, Holl J, Abecassis M and Ladner D. (2014). The Extent and Predictors of Waiting Time Geographic Disparity in Kidney Transplantation in the United States. Transplantation, 97(10), pp.1049--1057. (Journal article) 3. Organizacion Nacional de Transplantes, Newsletter TransplantInternational figures on donation and transplant. (2014). http://www.ont.es/publicaciones/Documents/NEWSLETTER %202014.pdf (Online Publication) 4. Gentry, S., Montgomery, R., Swihart, B. and Segev, D. (2009). The roles of dominos and nonsimultaneous chains in kidney paired donation. American Journal of Transplantation, 9(6), pp.1330-1336. (Journal article) 5. Karam, G., Kalble, T., Alcaraz, A., Aki, F., Budde, K., Humke, U., Kleinclauss, F., Nicita, G., Olsburgh, J. and Susal, C. (2012). Guidelines on renal transplantation. EAU guidelines. http://www.uroweb.org/gls/pdf/Renal%20Transplantation%202010. pdf (Online Publication). Criteria involved in kidney transplantation from deceased donors 1. Panduranga SR, Akinlolu O. The alphabet soup of kidney transplantation: SCD, DCD, ECD—fundamentals for the practicing nephrologist. Clinical Journal of the American Society of Nephrology. 2009: 4(11) 1827-1831. http://cjasn.asnjournals.org/content/4/11/1827.long (Review Article) Provides an excellent background to the terminology in renal transplant and general implications of kidney quality on clinical outcome 2. NHS organ donation. Section 5 - Kidney Activity Activity Report 2013-2014. 2014: 29- 31 http://www.organdonation.nhs.uk/statistics/transplant_activity_re port/current_activity_reports/ukt/activity_report_2013_14.pdf. (Onlin e Publication) 3. Karam G, Kalble T, Alcaraz A, Aki F, Budde K, Humke U, Kleinclauss F, Nicita G, Olsburgh J, Susal C. (2013) Guidelines on renal transplantation. Arnhem, the Netherlands: European Association of Urology (EAU) 2013: 2943.http://www.uroweb.org/fileadmin/tx_eauguidelines/2009/Full/Ren al_Transplant.pdf (Online publication) 4. Callaghan CJ, Harper SJF, Saeb-Parsy K, Hudson A, Gibbs P, Watson CJE, Praseedom RK, Butler AJ, Pettigrew GJ, Bradley JA The discard of deceased donor kidneys in the UK. Clinical Transplantation 2014: 28(3) 345-353 http://onlinelibrary.wiley.com.ezproxy.is.ed.ac.uk/doi/10.1111/ctr.12 319/full. (Journal article) 5. Chavalitdhamrong D, Jagbir G, Steve, T, Bhaskara RM, Yong WC, Tariq S, Suphamai B. Patient and graft outcomes from deceased kidney donors age 70 years and older: an analysis of the Organ Procurement Transplant Network/United Network of Organ Sharing database. Transplantation 2008: 85(11) 15731579. http://ovidsp.tx.ovid.com/sp3.13.1a/ovidweb.cgi?T=JS&PAGE=fulltext&D=ovft&AN=00007890200806150-00016&NEWS=N&CSC=Y&CHANNEL=PubMed. (Primary Research Article) 6. Giessing M, Fuller TF, Friedersdorff F, Deger S, Wille A, Neumayer H, Schmidt D, Budde K, and Liefeldt L. Outcomes of transplanting deceased-donor kidneys between elderly donors and recipients. Journal of the American Society of Nephrology. 2009: 20(1) 37-40. (Primary Research Article) 7. Mgbako O, Glazier A. Blumberg E, Reese PP. Allowing HIV‐Positive Organ Donation: Ethical, Legal and Operational Considerations. American Journal of Transplantation. 2013: 13(7) 1636-1642. (Review Article) 8. Muller E, Kahn D, Mendelson MD, Renal Transplantation between HIV-Positive Donors and Recipients. The New England Journal of Medicine 2010: 362(24) 2336-2337 (Journal Article) 9. Hwang JK, Park SC, Kwon KH, Choi BS, Kim JI, Yang CW, Kim YS, Moon IS. Long-Term Outcomes of Kidney Transplantation From Expanded Criteria Deceased Donors at a Single Center: Comparison With Standard Criteria Deceased Donors. Transplantation proceedings. Elsevier, 2014: 46(2) http://ac.elscdn.com.ezproxy.is.ed.ac.uk/S004113451301275X/1-s2.0S004113451301275X-main.pdf?_tid=fda372f0-6d5c-11e4-90fb00000aacb35e&acdnat=1416120868_6b6cdf389fb3bb89605cfa47c 8c9c16c. (Primary Research Article) 31 grafts from ECDs and 164 grafts from SCDs were followed, good follow up period (10 year) but the study was conducted at a single centre so it may not be widely representative. Matching kidneys’ predicted graft survival rates to patients’ predicted survival rates to reduce the kidney transplant waiting list 1. Ojo AO, Hanson JA, Wolfe RA, Leichtman AB, Agodoa LY, Port FK. Long-term survival in renal transplant recipients with graft function. Kidney Int. International Society of Nephrology; 2000 Jan;57(1):307–13. http://dx.doi.org/10.1046/j.15231755.2000.00816.x (Primary Research Article) 2. Rao PS, Schaubel DE, Guidinger MK, Andreoni KA, Wolfe RA, Merion RM, et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation. 2009 Jul 27 ;88(2):231– 6. http://www.ncbi.nlm.nih.gov/pubmed/19623019 (Primary Research Article) A large study of 69,440 donor transplants adequately assessing the factors that influence death or graft failure. 3. Lee APK, Abramowicz D. Is the Kidney Donor Risk Index a step forward in the assessment of deceased donor kidney quality? Nephrol Dial Transplant . 2014 Oct 4 ;0:16. http://ndt.oxfordjournals.org/content/early/2014/10/04/ndt.gfu304.l ong?hwshib2=authn:1414580318:20141028%3A74f8c73b-2a2b46e2-bc8933cb993419d9:0:0:0:DfqFLUt7rHIQ9u3XI7Hc+w== (review article) A useful review article summarising the use of KDPI and EPTS. 4. Israni AK, Salkowski N, Gustafson S, Snyder JJ, Friedewald JJ, Formica RN, et al. New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am SocNephrol . 2014 Aug 15; 25(8):1842– 8. http://www.srtr.org/publications/pdf/Israni_New_national_allocatio n_policy_for_deceased_donor_kidneys_Online.pdf (primary research article) A study simulating the benefits of using KDPI in conjunction with the EPTS. Living kidney donor criteria 1. NHS: Blood and Transplant. (2014) Kidney Activity- Organ Donation. http://www.odt.nhs.uk/pdf/LKDT_2020_strategy.pdf (NHS Strategy Summary) 2. Montgomery R, Lonze B, King K, Kraus E, Kucirka L, Locke J et al. Desensitization in HLA-Incompatible Kidney Recipients and Survival. New England Journal of Medicine. 2011;365(4):318326. http://www.nejm.org.ezproxy.is.ed.ac.uk/doi/full/10.1056/NEJM oa1012376 (Primary Research Article) A single-centre study evaluating rates of survival after LKDT in 211 consecutive patients with donor-specific anti-HLA antibody after undergoing desensitisation compared with matched control subjects on a kidney-transplant waiting list. A standardised protocol was used. Baseline characteristics of patients were skewed. The study has a short follow up time. 3. Montgomery J, Berger J, Warren D, James N, Montgomery R, Segev D. Outcomes of ABO-Incompatible Kidney Transplantation in the United States. Transplantation. 2012; http://ovidsp.tx.ovid.com.ezproxy.is.ed.ac.uk/sp3.13.1a/ovidweb.cgi?&S=ABAIFPGNIBDDOININCLKOCIBEEJGAA 00&Link+Set=S.sh.27%7c1%7csl_10 (Primary Research Article) A retrospective US study comparing patients who underwent live-donor ABO incompatible transplantation with ABO compatible-matched controls. A large population is used however confounding may be present due to characteristics not measured. 4. Krishnamurthi V. Risk of End-Stage Renal Disease Following Live Kidney Donation. Yearbook of Urology. 2014;2014:1921. http://jama.jamanetwork.com/article.aspx?articleid=1829682 (Pr imary Research Article) A prospective cohort study in US, comparing the risk of endstage renal disease in kidney donors with matched healthy nondonors at an equally low risk of renal disease. Large sample sizes were used and clinical and demographic variables were considered. Follow up time may have limited the understanding of the effects on ESRD and secular trends may have attributed to the results. 5. Mjøen G, Hallan S, Hartmann A, Foss A, Midtvedt K, Øyen O et al. Long-term risks for kidney donors. Kidney International. 2013;86(1):162-167. http://www.nature.com.ezproxy.is.ed.ac.uk/ki/journal/v86/n1/full/ki2 013460a.html(Primary Research Article) A single centre prospective cohort study in Norway with a long follow up time and large cohorts compared the long-term allcause mortality, cardiovascular mortality, and risk for ESRD in kidney donors with a selected control group screened for eligibility for live-kidney donation. No donors were lost to follow up. There was missing data on confounding factors. 6. Garg A, Nevis I, McArthur E, Sontrop J, Koval J, Lam N et al. Gestational Hypertension and Preeclampsia in Living Kidney Donors. N Engl J Med 2011; 365:318326 http://www.nejm.org/doi/full/10.1056/NEJMoa1408932 (Primary Research Article) A retrospective, matched-cohort study in Canada compared the risk of gestational hypertension and preeclampsia in living kidney donors and non-donors. high level of health surveillance was used for both cohorts. Data for some confounding factors including racial information were not considered. 7. Frade I, Fonseca I, Dias L, Henriques A, Martins L, Santos J et al. Impact Assessment in Living Kidney Donation: Psychosocial Aspects in the Donor. Transplantation Proceedings. 2008;40(3):677681. http://www.sciencedirect.com.ezproxy.is.ed.ac.uk/science/articl e/pii/S0041134508001450 (Primary Research Article) 8. Segev D. Innovative strategies in living donor kidney transplantation. Nat Rev Nephrol. 2012;8(6):332-338. http://www.nature.com.ezproxy.is.ed.ac.uk/nrneph/journal/v8/n6/full/ nrneph.2012.82.html (Review) 9. Fan X, Lin T, Xu K, Yin Z, Huang H, Dong W et al. Laparoendoscopic Single-Site Nephrectomy Compared with Conventional Laparoscopic Nephrectomy: A Systematic Review and Meta-analysis of Comparative Studies. European Urology. 2012;62(4):601612. http://www.sciencedirect.com.ezproxy.is.ed.ac.uk/science/articl e/pii/S0302283812006392 (As reviewed in Clayman RV1, Kavoussi LR, Figenshau RA, Chandhoke PS, Albala DM. Laparoscopic nephroureterectomy: initial clinical case report. 1991 Dec;1(6):34310. Canes D, Berger A, Aron M, Brandina R, Goldfarb D, Shoskes D et al. Laparo-Endoscopic Single Site (LESS) versus Standard Laparoscopic Left Donor Nephrectomy: Matched-pair Comparison. European Urology. 2010;57(1):95101. http://www.sciencedirect.com.ezproxy.is.ed.ac.uk/science/articl e/pii/S0302283809007702 (Primary Research Article) A retrospective matched-pair comparison study compared the convalescence in living donors for LESS-DN and LLDN. Baseline demographics were comparable between groups used. Small sample sizes of cohorts within a short time frame were selected. Models of organ donation *N.B for this section, it was particularly hard to find relevant and recent primary research articles as the majority of papers were simply reviewing models" 1. Organ Donation and Transplantation. NHS: Blood and Transplant. 2014. http://www.organdonation.nhs.uk/statistics/transplant_activity_repor t/current_activity_reports/ukt/activity_report_2013_14.pdf (Report) 2. Organizacion Nacional de Transplantes, Newsletter TransplantInternational figures on donation and transplant. (2014). http://www.ont.es/publicaciones/Documents/NEWSLETTER %202014.pdf (Online Publication) 3. Matesanz R, Dominguez-Gil B. Strategies to optimize deceased organ donation. 2007. Transplantation Reviews. 21(4), pp.177188. doi:10.1016/j.trre.2007.07.005 (Review) A good review of the Spanish model which highlights and discusses the success of the integrated approach taken by Spain. 4. The potential impact of an opt out system for organ donation in the UK. UK Organ Donation Taskforce. 2008. http://www.odt.nhs.uk/pdf/the-potential-impact-of-an-opt-outsystem-for-organ-donation-in-the-UK.pdf (Report) 5. Taking Organ Transplantation to 2020; A detailed strategy. NHS: Blood and Transplant. 2013. http://www.nhsbt.nhs.uk/to2020/resources/nhsbt_organ_dono r_strategy_long.pdf (NHS Strategy Summary) 6. Organ Donation Consultation. Royal College of Nursing. 2009. http://www.nhsbt.nhs.uk/to2020/resources/nhsbt_organ_dono r_strategy_long.pdf (Policy Briefing) 7. Traino HM, Alolod GP, Shafer T, Siminoff LA. Interim Results of a National Test of the Rapid Assessment of Hospital Procurement Barriers in Donation (RAPiD). Am J Transplant. 2012; 12: 3094– 3103. doi: 10.1111/j.1600-6143.2012.04220.x (Primary Research Article) 8. Abadie A, Gay S. The impact of presumed consent legislation on cadaveric organ donation: a cross-country study. J Health Econ. 2006; 25: 599. http://www.sciencedirect.com/science/article/pii/S0167629606 00004X (Primary Research Article) 9. Ghods AJ, Savaj S. Iranian model of paid and regulated livingunrelated kidney donation. Clinical Journal of the American Society of Nephrology. Clin J Am Soc Nephrol. 2006 Nov;1(6):113645. http://cjasn.asnjournals.org/content/1/6/1136.full (Review) A good review but it could be biased as one of the authors, Ajad J. Ghods, helped to develop the model for Iran. 10. Rudge C, Matesanz R, Delmonico F, Chapman J. International practices of organ donation. BJA. 2011; 108: pp.i48-i55. http://bja.oxfordjournals.org/content/108/suppl_1/i48.full (Review) Methods to Improve familial consent rates in a clinical setting 1. NHS: Blood and Transplant. (2013) Taking organ transplantation to 2020; A detailed strategy. http://www.nhsbt.nhs.uk/…/nhsbt_organ_donor_strategy_long.pdf (Accessed 22/11/14) (NHS Strategy Summary) 2. Sanner MA. Two perspectives on organ donation: experiences of potential donor families and intensive care physicians of the same event. (2007) J Critical Care. 2007;22:296– 304 http://www.ncbi.nlm.nih.gov/pubmed/18086400 (Primary Research article) This article was most effective at demonstrating the effects of the approach of doctors to consent rate, particularly with respect to pro-donation attitudes. It had a novel qualitative methodology combining interviews of physicians with relatives to produce narratives. However there was a relatively small sample size. 3. DeJong W., Franz H.G., Wolfe S.M., Nathan H., Payne D., Reitma W. & Beasley C. (1998) Requesting organ donation: an interview study of donor and nondonor families. American Journal of Critical Care 7(1), 13– 23 http://www.ncbi.nlm.nih.gov/pubmed/9429679 (Primary research Article – Abstract only. Could not access article) 4. Rodrigue JR, Cornell DL, Howard RJ (2006) Organ donation decision: Comparison of donor and non-donor families. Am J Transplant 6: 190– 8 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2365918/ (Primary Research Article) Good qualitative article with a multifactorial approach to asking for consent. Large sample size and interviews conducted soon after death which was not the case in many other papers. 5. Siminoff LA, Lawrence RH (2002) Knowing patients' preferences about organ donation: does it make a difference? Journal of Trauma-Injury Infection & Critical Care 53: 754-60. (As reviewed in Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ. 2009;338:b991. http://www.ncbi.nlm.nih.gov/pubmed/19383730) 6. Groot J, Vernooij-Dassen M, Vries A, Hoedemaekers C, Hoitsma A, Smeets W, van Leeuwen (2014) E. Intensive care staff, the donation request and relatives’ satisfaction with the decision: a focus group study. BMC Anesthesiology 2014, 14:52 http://www.biomedcentral.com/1471-2253/14/52 (Primary Research Article) Small study with focus groups had interesting results. It talked about the experience from families and then drew conclusions on their emotional response to improve consent rates) 7. Niles PA, Mattice BJ (1996) The timing factor in the consent process. Journal of Transplant Coordination 6: 84– 7 http://natco.metapress.com/content/r51w123x42715130/ (Primary Research Article - abstract only) Medium sized study with which demonstrated large falls of consent when death and organ donation were coupled 8. Gortmaker SL, Beasley CL, Sheehy E, Lucas BA, Brigham LE, Grenvik A. et al. (1998) Improving the request process to increase family consent for organ donation. J Transpl Coord. 1998;8(4):210– 217. http://www.bumc.bu.edu/len/files/2009/03/improving-therequest-process-to-increase-family-consent-for-organ-donation1998.pdf (Primary Research Article) Large retrospecitive study which focused on decoupling and the role of a coordinator in the request process. 9. von Pohle W, Linda L. (1996) Obtaining organ donation: Who should ask. Heart Lung. 1996;25:304– 9. http://www.ncbi.nlm.nih.gov/pubmed/8836746 (Abstract – Full text not available) 10. Jenkins, Donald H; Reilly, PM; Shapiro, MB; Russell, MW; Frankel, HL; Lee, SY; Hawthorne, RV; Alavi, A; Schwab, CW. (1998)Effect of Rapid Brain Death Determination on Organ Donation Rates: A preliminary Report. Critical Care Medicine: January 1998 - Volume 26 - Issue 1 - p 31A (As reviewed in Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ. 2009;338:b991. http://www.ncbi.nlm.nih.gov/pubmed/19383730) 11. Eide H, Foss S, Sanner M, Mathisen JR. (2012) Organ donation and Norwegian doctors' need for training. Tidsskr Nor Laegeforen 2012;132:1235-8. http://tidsskriftet.no/article/2271448 (Primary Research Article) Large questionnaire based study. Found that many doctors lack sufficient training and that doctors should keep to standard practice when asking for consent. 12. Ebadat A, Brown CV, Ali S et al (2014) Improving organ donation rates by modifying the family approach process. J Trauma Acute Care Surg 76(6):1473–1475 http://www.cedarssinai.edu/Patients/Programs-and-Services/Surgery/SurgicalEducational-Programs/Documents/SICU-Articles/Improving-organdonation-rates.pdf (Primary Research Article) Large retrospective study with a very large multi-factorial approach to asking consent. Very good article. Reasons behind the variation in rates of organ donation between different ethnic groups and how to improve them 1. Black, Asian and Minority Ethnic Organ Donation and Transplantation data. NBTA. 2013 July. http://www.nbtauk.org.uk/wp-content/uploads/2013/08/NBTA-Organ-data-reportupdate-July-2013.pdf (Report) 2. Taking Organ Transplantation to 2020; A detailed strategy. NHS: Blood and Transplant. 2013. http://www.nhsbt.nhs.uk/to2020/resources/nhsbt_organ_dono r_strategy_long.pdf (NHS Strategy Summary) 3. NHSBT. Black, Asian and Minority Ethnic communities. http://www.organdonation.nhs.uk/how_to_become_a_ donor/black_and_other_minority_ethnic_communities/ (Webpage) 4. Summers DM, Johnson RJ, Hudson AJ, Collett D, Murphy P, Watson CJE, Neuberger JM, Bradley JA. Standardized deceased donor kidney donation rates in the UK reveal marked regional variation and highlight the potential for increasing kidney donation: a prospective cohort study. Br J Anaesth. 2014; 113(1): 83– 90. doi:10.1093/bja/aet473 (Primary research article) The findings of this recent paper are reliable as the study was very large (27,482) and p-values were significant. This paper is therefore useful in highlighting the clear influence of ethnicity on organ donation. 5. Morgan M, Hooper R, Mayblin M, Jones R. Attitudes to kidney donation and registering as a donor among ethnic groups in the UK. J Public Health (Oxf). 2006; 28(3): 226– 34. http://jpubhealth.oxfordjournals.org/content/28/3/226.long (Prim ary research article) Relatively large study (1,606) and high participation rates (however participation rates were significantly lower among ethnic minorities, possibly skewing the data). The questionnaire was adapted from previous studies and interviews meaning that it was very relevant. While the data was adjusted was age, sex and level of education, it could have been adjusted for more factors to reduce the possibility of confounding. 6. Karim A, Jandu S, Sharif A. A survey of South Asian attitudes to organ donation in the United Kingdom. Clin Transplant. 2013; 27(5), 757–63. doi:10.1111/ctr.12189 (Primary research article) 7. Morgan M, Adams OP, Seed PT, Jones R. Ethnicity and attitudes to deceased kidney donation: a survey in Barbados and comparison with Black Caribbean people in the United Kingdom. BMC Public Health. 2010; 10, 266. http://www.biomedcentral.com/content/pdf/1471-2458-10266.pdf (Primary research article) 8. Morgan M, Mayblin M, Jones R. Ethnicity and registration as a kidney donor: the significance of identity and belonging. Soc Sci Med. 2008; 66(1): 14758. http://www.sciencedirect.com/science/article/pii/S02779536070 0456X (Primary research article) A well conducted study which collected data from a small number of participants through in-depth interviews. These interviews were important in identifying deep and underlying issues involving identity and belonging. Larger and less in-depth studies would not have been as useful. 9. Randhawa G, Brocklehurst A, Pateman R, Kinsella S, Parry V. “Opting-in or opting-out?”--the views of the UK’s faith leaders in relation to organ donation. Health Policy (Amsterdam, Netherlands). 2010; 96(1): 36– 44. http://www.sciencedirect.com/science/article/pii/S01688510090 03364 (Primary research article) 10. Randhawa G, Brocklehurst A, Pateman R, Kinsella S, Parry V. Religion and organ donation: the views of UK faith leaders. J Relig Health. 2012; 51(3): 743751. http://link.springer.com/article/10.1007/s10943-010-93743?no-access=true (Primary research article) Only 17 interviews but the paper is trying to assess the views of ‘UK faith leaders’ and gather views on organ donation from a wide range of leading faith and belief organisations. 11. Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the U.K.: a synthesis of quantitative and qualitative research. Ethn Health. 2013; 18(4): 367– 90. doi:10.1080/13557858.2012.752073 (Review) An extensive and useful review which synthesises information from many different studies. These studies ranged significantly e.g. 12 participants vs 6080 participants. 12. Sims JM, Kenten C, Deedat S, Randhawa G, Morgan M. Better Health Briefing Paper 25, Overcoming barriers to registering as an organ donor among minority ethnic groups. Race Equality Foundation. 2012 November. http://better- health.org.uk/sites/default/files/briefings/downloads/Overcoming%2 0barriers%20to%20registering%20as%20an%20organ%20donor% 20among%20minority%20ethnic%20groups_0.pdf (Review) 13. Hourigan CS. Registering organ donor preferences - a third way? The British Journal of General Practice. 2005; 55(519): 805. http://bjgp.org/content/55/519/805 (Journal Article) 14. Randhawa, G. Death and organ donation: meeting the needs of multiethnic and multifaith populations. Br J Anaesth. 2012; 108(S1): i88i91. http://bja.oxfordjournals.org/content/108/suppl_1/i88.long (Revi ew) Methods of Kidney Paired Donation 1. Wallis CB, Samy KP, Roth AE, Rees MA. Kidney Paired Donation. Nephrol Dial Transplant. 2011;26(7): 2091– 9. http://ndt.oxfordjournals.org.ezproxy.is.ed.ac.uk/content/26/7/209 1 (Journal Article) An excellent article for establishing background knowledge; explaining the methods of kidney paired donation and the logistics of their implementation. 2. Segev DL, Gentry SE, Warren DS, Reeb B, Montgomery RA. Kidney Paired Donation and Optimizing the Use of Live Donor Organs. JAMA. American Medical Association; 2005;293(15): 1883– 90. http://jama.jamanetwork.com.ezproxy.is.ed.ac.uk/article.aspx?ar ticleid=200729 (Primary Research Article) 3. Gentry SE, Montgomery RA, Segev DL. Kidney paired donation: fundamentals, limitations, and expansions. Am J Kidney Dis. 2011;57(1): 144–51. http://www.sciencedirect.com/science/article/pii/S02726386100143 93 (Primary Research Article) 4. Simpkins CE, Montgomery RA, Hawxby AM, Locke JE, Gentry SE, Warren DS, et al. Cold ischemia time and allograft outcomes in live donor renal transplantation: is live donor organ transport feasible? Am J Transplant. 2007;7(1): 99–107. http://www.ncbi.nlm.nih.gov/pubmed/17227561 (Primary Research Article) A retrospective cohort study with a large sample of 56,341 live kidney transplant recipients, which found no negative long-term effects on kidney outcomes with cold ischaemic times less than eight hours. 5. Gentry SE, Montgomery RA, Swihart BJ, Segev DL. The roles of dominos and nonsimultaneous chains in kidney paired donation. Am J Transplant. 2009;9(6): 1330–6. http://www.scopus.com/inward/record.url?eid=2-s2.066249109591&partnerID=tZOtx3y1 (Primary Research Article) A mathematical model study researching participation of nondirected donors in dominos or chains as a way of expanding kidney paired donation. 6. Statistics and Clinical Studies, NHS Blood and Transplant. Organ Donation and Transplantation; Activity Report 2013/2014. 2014 p. 28-44. http://www.organdonation.nhs.uk/statistics/transplant_activity_repo rt/current_activity_reports/ukt/activity_report_2013_14.pdf (Report) 7. Gentry SE, Segev DL, Montgomery RA. A comparison of populations served by kidney paired donation and list paired donation. Am J Transplant. 2005;5(8):1914–21. http://www.ncbi.nlm.nih.gov/pubmed/15996239 (Primary Research Article) 8. Eurotransplant International Foundation. Annual Report 2013. https://www.eurotransplant.org/cms/mediaobject.php?file=AR2013 5.pdf (Report) 9. OPTN/UNOS KPD Work Group. The State of the OPTN/UNOS KPD Pilot Program. 2014. http://optn.transplant.hrsa.gov/ContentDocuments/KPD_Report.pdf (Report) < Information Search Report Word Version>