this HAI Learning Resource - NHS Education for Scotland
advertisement

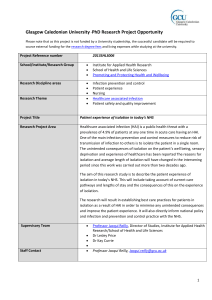
Welcome to this HAI Learning Resource In April 2015 two national conferences were hosted by NHS Education for Scotland (NES). Their aim was to raise awareness of HAI prevention and control among acute and nonacute frontline staff across health and social care. The content developed for these conferences has been used to create this HAI Learning Resource for use by local HAI trainers. The resource is organised into three sections: Engage, Inform and Interact. There are also short questionnaires to check how your learners are doing. Figure 1 Exhibition Hall, Glasgow An indication of how much time each activity might take is provided at relevant points throughout the resource. Over all, it should take you between 2.5 and 3 hours to complete (depending on size of group and the amount of additional HAI information you provide). 1. First Questionnaire (ice breaker) 2. Engage: This section helps learners to reflect on the human costs of HAIs. The personal experience of Helen, a woman who contracts a surgical site infection, is examined with reference to the global consequences of antimicrobial resistance. 3. Inform: This section provides key messages from four different areas relevant to HAI prevention and control: Antimicrobial prescribing and stewardship: continuity across health and social care settings. National Infection Prevention and Control Manual: what does this mean in practice? Implementing the Manual: three Examples from Practice o Scottish Ambulance Service o NHS Greater Glasgow and Clyde o NHS Grampian HAI Standards: applying in the real world 4. Second Questionnaire (checking knowledge) 5. Interact: This section helps learners to identify their learning and plan action to improve HAI practice in their local area. 6. Third Questionnaire (what next) 2 First Questionnaire (Ice Breaker) These questions were designed to capture demographic information at the conferences. Instruction to Trainers: Following your own introduction to your session, use these questions to help gather information about your learners. Feel free to replace them with ice breaker questions that better suit your audience and purpose (3 mins) 1. What would you rather have? 1. A glass half full 2. A glass half empty 3. A glass with a straw 4. No glass at all 2. Which job role describes you best? 1. Social Care Staff 2. Healthcare Support worker 3. Nurse/ Midwife 4. Medical staff 5. Dental staff 6. Allied Health Professional 7. Ambulance Staff 8. Student 9. Care Home Manager/ Care Home Staff 10. Other Figure 2 Response from Glasgow Conference 3. Where in Scotland do you work? 1. The Islands 2. Highlands 3. North East 4. North West 5. Central Belt 6. South East 7. South West 8. Other 4. How familiar are you with the Standard Infection Control Precautions (SICPs)? 1. Very Familiar 2. Familiar 3. Not familiar 4. Have never heard of them 5. How easily can you access information locally regarding Infection Prevention and Control? Give a score on a scale of 1-4, where 1 is Very Easy, and 4 is Very Difficult 3 ENGAGE The Experience of HAI Dr Esther Walker, Tess Allen, Forum Interactive Ltd Instruction to Trainer: use the information below to introduce the story to your learners (5 mins) “Helen’s Story” is designed to set the scene by placing the complex issues around HAI prevention and control in a practical, human context. The dramatized story highlights the human cost of HAIs, encouraging the learner to make a personal connection with this aspect of patient safety and to consider what HAI prevention and control means in the context of their own role. ‘Helen’ goes into hospital for a routine surgical procedure. What happens to her in the following days and weeks was drawn up in consultation with different professional experts. Figure 3 Dr Esther Walker Helen will tell learners some of what happened to her. But this story is very much from her perspective. We don’t hear from any of the professionals involved in her care. Neither do we hear about any of the conversations that she may have had with any of the health care professionals she encountered. That is intentional. What we want is to leave things open for learners to use their own knowledge, experience and skill to imagine that side of the story and to think about the issues or questions it raises about infection prevention and control. The Story The story moves backwards and forwards in time. It begins with Helen talking about her experience of HAI one year on. Instruction to Trainers: o Show learners the film Helen’s Story (25 mins) o Ask them the questions below. If numbers allow, ask them to work in small groups and then discuss all together (20 mins) o You may like to supplement this list with your own questions. Figure 4 Tess Allen as 'Helen' 4 Questions 1. What strikes you as important about what you’ve heard in this story? 2. What issues/questions does the story raise for you about infection prevention and control? 3. What do you make of the conversation between Helen and her friend Pam? Was Helen ‘unlucky’ or is there more that health and social care staff can do to prevent infections? 4. What do you want to learn from today’s session about HAI prevention and control? Extension Activity Learners have heard part of Helen’s Story, the part that she chose to tell and that was revealed through the skyped conversations. Another part of the story is the detail of what happened to her in terms of her changing healthcare needs and the clinical care she received in response. Instruction to Trainers: Take a look at the sequence of events referred to above (see Appendix I). Instruct the group to use this information to identify the possible points in Helen’s journey of care where something may have gone wrong, leading to her contracting the HAI. Ask them to use their own knowledge and experience to fill in the gaps. Again, if numbers allow, ask them to work in small groups and then discuss all together (20-30 mins) 5 INFORM Instruction to Trainers: use the information in the following presentations from the conference to supplement the content that you would usually provide in your HAI training sessions. (approx. 60 mins) Antimicrobial prescribing and stewardship: continuity across health and social care settings Professor Dilip Nathwani, Consultant in Infectious Diseases, NHS Tayside Antibiotic prescribing: 80% of all antibiotics are prescribed in the community with the remaining 20% prescribed in hospitals. Between 30-50% of these prescriptions can be inappropriate or unnecessary. Overuse and misuse of antibiotics in human health is a key driver for antibiotic resistance. Figure 5 Professor Dilip Nathwani “The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily under dose himself and, by exposing his microbes to non-lethal quantities of the drug, educate them to resist penicillin.” Sir Alexander Fleming, Nobel Lecture 1945 “…hip replacement. Currently, prophylaxis is standard practice, and infection rates are about 0.5-2%, so most patients recover without infection, and those who get an infection have it successfully treated. We estimate that without antimicrobials, the rate of postoperative infection is 40-50% and about 30% of those with an infection will die.” R Smith & J Coast BMJ 2013 Antibiotic stewardship: Stewardship is a core evidence based strategy to improve the quality of antibiotic prescribing across the health care communities. With the relative paucity of new antibiotic development we need to preserve the durability of this precious resource. “We have watched too passively as the treasury of drugs that has served us well has been stripped of its value. We urge our colleagues worldwide to take responsibility for the protection of this precious resource. There is no longer time for silence and complacency.” Jean Carlet et al Lancet April 2011 6 Reference to antimicrobial nurse stewardship. Infection prevention teams: Infection prevention teams, antimicrobial management teams and clinical or care teams need to work closely to effectively deliver better infection prevention and management. The role of measurement and feedback through routinely collected informatics is fundamental to measuring and driving success. Figure 6 Priority actions to address AMR 7 INFORM National Infection Prevention and Control Manual: what does this mean in practice? Lisa Ritchie, Nurse Consultant Infection Control, Health Protection Scotland The National Infection Prevention and Control Manual for Scotland was published on the 13th January 2012, under CNO (2012) to be adopted by all NHS staff. The Manual aims to align evidence based practice with monitoring assurance, quality improvement and scrutiny by providing a straightforward practice guide based on an assessment of the extant professional literature. Chapter 1 covers Standard Infection Control Precautions (SICPs), the basic infection prevention and control measures necessary to reduce the risk of transmission of infectious agents, to be used by all staff, in all care settings at all times, for all patients Figure 7 Lisa Richie Chapter 2 covers Transmission Based Precautions (TBPs), the additional precautions (to SICPs) required to be used when a patient is known or suspected to be infectious. The Manual promotes the application of evidence based (not ritualistic) care processes. The literature reviews are separate from the practice guide, they summarise the available evidence that underpin and informs the practice guide, and highlight implications for further research. The Manual complements national improvement programs and provides a focus for the development of local measurement plans to achieve sustained practical implementation of a small number of critical activities into everyday practice (making the right thing easy to do for every patient every time). The Manual provides an example quality improvement data collection tool which contains a critical elements checklist can be used as an aide memoire to monitor SICPs practice. 8 A new National Infection Prevention and Control Manual website is under construction and will be available soon – watch this space. Meanwhile, the manual can be accessed here. Accessing the HAI Standards Figure 8 Opportunities to break the chain of infection “Good prevention control practices break the chain of infection: Infection prevention, unlike short-term control measures used in outbreak situations requires ongoing consistent best practice at each and every stage of every patient’s care, from hand hygiene, to insertion of intravenous lines to routine cleaning of the environment and patient equipment.” Lisa Ritchie 9 INFORM Implementing the National Infection Prevention and Control Manual The Scottish Ambulance Service: Travelling from Strength to Strength Sharon Doyle, HAI Quality Improvement Facilitator, Scottish Ambulance Service Background: The Ambulance Service undertakes about 2 million journeys per year, half a million of which are emergency journeys. We have about 150 service locations including ambulance stations, air ambulance and special operation response teams. We have over 4,000 staff. What did we do? It was identified that SICP's (Standard Infection Control Procedures) needed to be improved from many different audits and data feedback we identified two improvement projects to embed SICPs to the service and raise knowledge, awareness and confidence among staff of using and implementing the guidance. Figure 9 Sharon Doyle Figure 10 Two projects for SICPs integration 10 Cleanliness champions (n=1000) designed and implemented an improvement project relevant to their local area. Outcomes: Enhance SICPs knowledge in trial locations Renewed enthusiasm Vehicle cleaning records completion improved We will continue with these small tests of change and the ultimate goal is to spread these throughout the service. Academy Education we revised the presentation for the infection control and prevention course to make sure that SICPs was fully embedded. Outcomes: • • SICPs being considered in clinical scenarios Students have more confidence around SICPs 11 INFORM Implementing the National Infection Prevention and Control Manual NHS Greater Glasgow and Clyde: A Quality Improvement Approach to reduce Catheter Associated Urinary Tract Infection (CAUTI) Gillian Mills, Healthcare Associated Infection: Quality Improvement Facilitator, Glasgow Royal Infirmary. Urinary Tract Infection (UTI) is the leading cause of healthcare associated infection (HAI) in NHS Scotland, with around 50% of UTIs being associated with an indwelling urethral urinary catheter (UUC). Alternatives to UUC should be considered prior to inserting a UUC. If a UUC is the only option for your patient, it should be removed as soon as possible to reduce the risk of catheter associated urinary tract infection (CAUTI). Figure 11 Gillian Mills Asymptomatic bacteriuria (ASB) is the presence of bacteria in the urine without clinical signs and symptoms of UTI. ASB are commonly treated in patients with indwelling UUCs despite the patient having no clinical signs and symptoms of CAUTI. Inappropriate treatment of ASB can increase the patient’s risk of developing clostridium difficile and can have an impact on antimicrobial resistance. Symptomatic UTI cannot be differentiated from ASB on the basis of a urine dipstick test. DO NOT use urine dipstick test in diagnosis of UTI in people with indwelling catheters. 12 Figure 12 Improvement and Patient Outcomes of CAUTI project Figure 13 The range of stakeholders involved in CAUTI project 13 INFORM Implementing the National Infection Prevention and Control Manual NHS Grampian: The Who, When, how and What of Equipment Decontamination Catherine Mitchell, HAI Quality Improvement Facilitator & Scott Arnot, Domestics Training Manager, NHS Grampian NHS Grampian received negative press as result of a Healthcare Environment Inspection. In response, a short-life working group was set up with representation from stakeholder groups. What has been achieved so far? The Figure 14 Glasgow Conference group has reviewed and improved the NHS Grampian A-Z guide for the Decontamination of Near Patient Healthcare Equipment to include: Crib sheets Top tips for cleaning Clarification of responsibility Updated information on manufacturers’ instructions. Figure 15 Example of Crib Sheet 14 Figure 16 Example of Top Tips Patient Feedback “It‘s priceless to have a clean environment – it means the world to me. I came in with a condition and want to be cured, not go home with something else” A.D. “I feel comfortable and more at ease knowing I am being cared for in a clean room. I have complete confidence in the staff’s abilities” K.M. 15 INFORM HAI Standards: applying in the real world Alastair McGown, Senior Inspector, Healthcare Environment Inspectorate The Healthcare Environment Inspectorate focusses on infection prevent and control and inspects against HAI standards and associated guidance. Themes from HAI Inspections Hand hygiene Safe management of blood and body fluid spillages Safe disposal of waste Cleaning of the ward and patient equipment Emergency trolley beds and time to clean Figure 17 Alastair McGown The need for robust assurance systems Hospitals need to better use data they gather from audits to help them identify areas where improvement is needed. Information allows you to identify what you are doing well and what needs to improve. If the information is not robust then it can lead to: false assurance, failure to target appropriate areas for improvement, attracting further scrutiny, potential impact on reputation with users. Figure 18 the positives from HAI inspection reports Data to drive improvement Data that reflects practice will be more useful in identifying areas for improvement. Good communication of information to staff will enable them to act. By demonstrating self-regulation hospitals have less need for external scrutiny Self-regulation delivers better outcomes for service users. New HAI Standards are now in place (2nd May 2015) and apply to all healthcare organisations. NHS Boards are required to demonstrate that they have adopted the HAI standards as part of the HEI inspections. Inspections against these new standards begin June 2015. 16 Second Questionnaire (checking knowledge) These questions were designed to capture knowledge acquired by those attending the conference. Instruction to Trainers: use these questions to get a snapshot of how much your learners have taken in so far. Make the quiz more relevant to your content (and learners) by adding in your own questions. (3 mins) 1. What should antibiotics be used for: 1. Treat coughs and colds 2. Treat flu symptoms 3. Treat bacterial infections 4. Treat viral infections 5. All of the above Figure 19 Result from Glasgow Conference 2. When performing hand hygiene, do you ever miss any of the World Health Organisation (WHO) five moments? 1. I often miss a hand hygiene opportunity 2. I rarely miss a hand hygiene opportunity 3. I never miss any hand hygiene opportunity 4. I don't work with patients. 5. I don't know what the WHO Five Moments of Hand Hygiene are 3. What is the annual cost of Healthcare Associated Infections in NHS Scotland? 1. £8 million 2. £18 million 3. £83 million 4. £183 million Figure 20 Result from Glasgow Conference 17 INTERACT Your role in ‘strengthening our defences’ Mark Johnston, Training and Research Officer for Patient Safety, NHS Education for Scotland This section is to help learners to digest what they’ve learned from today and use it to plan action that will improve infection prevention and control in their area. Instruction to Trainers: Help learners to reflect on their learning by asking them this question – “What are the 3 most important things that you’ve learnt from this session so far?” Ask them to think about this on their own and then share responses with the whole group (5-10 mins) Figure 21 Mark Johnston Instruction to Trainers: Use the following information to introduce learners to the concept of Human Factors and to think about what influences their own behaviour (10 mins). Human Factors refer to environmental, organisational and job factors as well as human and individual characteristics which influence behaviour at work in a way which can affect health and safety. Making errors is a normal part of being human. Errors occur due to system design and how those systems influence behaviour. The system we work with may be set up to ensure we fail “every system is perfectly designed to achieve the results it gets.” Peter Senge As the following video shows, we can all be wise in hindsight. https://www.youtube.com/watch?v=opfXmYlTotc Access the video at Figure 22 Captain Hindsight video 18 It is important to plan what we are going to do and try to anticipate the unexpected. However, in real time we need to adapt that plan to the situation and circumstances we find ourselves in. To be effective, systems need to be designed to take account of real work situations – when things are chaotic as well as when things are calm. ‘We cannot change the condition of those who do the work, but we can change the conditions within which they work’ J Reason So if we want people to behave differently then we need to change the circumstances in which they work. In particular, we need to take into account the factors that influence human behaviour. Instructions to Trainers: Ask learners to consider what they could do in their local area that would improve infection prevention and control practice. It is important that they identify something that it is in their power to influence and that is relatively easy for them to achieve. Use these three questions below to help learners to plan that action (20 mins). My barrier – What barrier is there to your practice in Infection Prevention and Control? My action – What action can you take to improve practice in this area? My support need – What support do you need to do that? At the conference, delegates wrote their mini action plan up on postcards that were then displayed on a ‘Wall of Commitment’. Your learners might like to do something similar with colleagues or they could use the action planning template (see Appendix II). Figure 23 Postcards on the 'Wall of Commitment' 19 Third Questionnaire (next steps) These questions were designed to provide a quick evaluation of the conference. Instruction to Trainers: use these questions to evaluate the learning session. Make the quiz more relevant to your content (and learners) by adding in your own questions. (3 mins) Which of today’s themes had the biggest impact on you personally? 1. Understanding the personal impact of an infection 2. Awareness and concern of antibiotic resistance 3. The importance of Standard Infection Control Precautions 4. Understanding my contribution to infection prevention 5. Other Figure 24 Result from Glasgow Conference After today’s event how familiar are you now with the Standard Infection Control Precautions (SICPs)? 1. Very Familiar 2. Familiar 3. Not Familiar 4. Don’t know Figure 25 Result from Glasgow Conference 20 Appendix I Helen’s Story: Sequence of Events Helen’s perspective – what she knows and understands about what’s happening to her. Helen’s expectations of what this procedure would involve (this is routine). Helen had been having problems with gall stones for number of years. What happened? Notes Questions raised? PRE-OP Surgical removal of the gall bladder is one of the most common operations performed by the NHS. More than 60K gallbladders are removed each year. Was Helen screened properly prior to surgery? Referral to surgeon. Recommended keyhole surgery. MRSA screening performed 3 weeks prior to surgery at prescreening clinic. Clinical risk assessment. Informed consent sought. She was told there’s always risk of infection and that the care management may change depending on the individual’s disease condition and other risk factors. Day 1 operation Woke up with a wound across stomach. IN THEATRE SSI bundle was implemented. She had some a prophylactic antibiotic premedication as part of her induction to theatre. When surgeon attempts key-hole surgery he finds that her gall bladder is inflamed and adhered to bowel. Has to open up to have good look round. Laparoscopic (keyhole) cholecystectomy. Open cholecystectomy (gall bladder removed through incision in abdomen) What about her expectations? Did she properly understand that the MRSA screening was just for MRSA? Was anything else missed at this stage? SSI made up 18.6% of HAI's based on the last Scottish Point Prevalence survey, 2011 [15.9% in 2007]. Was the SSI bundle properly implemented? What could have been missed or gone wrong at this stage? Was ventilation system operating properly? Inserting the drain creates another ‘wound’ – how might this have increased risk of infection? Was it done properly? Drain inserted to remove excess fluid. 21 Day 2 HDU Day 3 discharged. Helen given Melolin (low adherent absorbent dressing) which she is to change daily herself. Day 6 Helen notices redness on wound. She does nothing - decides to wait (why?) Day 7 Wound sore. She phones GP Practice and the DN comes out. Day 8-9 Helen feeling sick; develops thrush. Day 11 results come back POST-OP She was in HDU for observation post operation due to inflammation (24 hours). DISCHARGE Wound checked by nurse on ward. It looks clean and dry. Discharge letter sent electronically to GP practice. DN makes home visit and notices wound red. Takes swab. Phones GP who writes prescription. Helen picks that up and starts treatment. GP phones to say that the lab results show that the bacteria she has includes a resistant organism (MRSA meticillinresistant staphylococcus aureus). The antibiotic she’s taking won’t be affective. Writes new prescription. What did the post op monitoring reveal? Was it done effectively? Charge nurse on ward – good audit for hand hygiene, all procedures followed (their audit result 93%) The information leaflet should be given to patient along with a conversation by the nurse to make sure she understands how to take care of her wound, what signs to look for that all is not well, what action to take, hand hygiene training. It would be routine and reasonable for GP to prescribe antibiotic that is most likely to be effective. GP prescribes flucloxacillin. Was the infection contracted on the ward? What about cleanliness/ environmental audits? What about Standard Infection Control audit (which would include hand hygiene)? Did Helen understand how to self- care following discharge? What might have gone wrong with communication from hospital to GP practice? She’s been prescribed antibiotic but if this isn’t the right antibiotic then she’s taking them for nothing. Why did Helen delay in contacting GP practice? Problem in communicating postoperative information? If infection picked up earlier would this have made a difference? New antibiotic will take 48 hours to kick in – too little, too late? Consider longer term impact of taking antibiotics. Did she get further advice from the DN? If so, then what would that have been? 22 Day 12-13 Wound continues to feel sore. Helen waits a couple of days for antibiotic to take effect. Day 14 wound starts to open Wound leaking, feeling feverish, shaking, temperature 38.5. Abdominal pain and pus coming through wound. Phones NHS24. The antibiotics make her feel ill, sick. The new antibiotic won’t start taking effect for 48 hours. Helen doesn’t get new antibiotic (vancomycin?) in time and so she gets sick. RE-ADMISSION TO HOSPITAL While at A&E she’s assessed & diagnose with sepsis. (Signs of systemic infection.) Sepsis 6 is a full series of interventions: Administer high flow oxygen Take blood cultures Give broad spectrum antibiotics Give intravenous fluid challenges Measure serum lactate and haemoglobin Measure accurate hourly urine output. Then admitted to emergency receiving ward. CT scan showed deep seated infection. Over the last few days the pressure has been mounting from the deep infection and its now seeping through the wound. So the SSI s not located in the wound itself (surface) but in the abdomen, where the surgery took place. Within hour she receives IV antibiotics. Decision to take her back to theatre, reopen wound, wash it out, put in drain to remove pus. After 3 days (day 17) she fails to progress. She’s diagnosed with hospital acquired pneumonia. She’s given oxygen and other antibiotics. She ends up in ITU on a ventilator for 2 days. A few days later, when it looks as if she’s improving she develops diarrhoeal symptoms. She’s diagnosed quickly with Start off with broad spectrum and then specify once they’re clearer what the bacteria is. As a result of broad spectrum antibiotics (a combination of antibiotics to kill lots of bacteria) is Clostridium Difficile. This occurs naturally in the gut and when other bacteria are killed off by the antibiotics, it allows the Cdiff to develop. In mild forms, the best treatment is to stop using antibiotics so that the natural balance of bacteria in the gut can be restored. The problem does beyond the SSI itself, to the additional risks created by all the interventions: e.g. more surgery exposing patient to risk of anaesthetic, possible contraction of further infection, being immobile so risk of clots in legs, risks of being in theatre, hospital acquired pneumonia. So not just about wound management. Antibiotics are all toxic so there are side effects and you don’t want to be on them for longer than necessary. A person’s risk of contracting an infection increases with every admission to hospital and for what duration. Hence, the ‘domino effect’. The alternative antibiotics used for resistant organisms are more toxic. Was there a full antibiotic review with a microbiologist? Was the PVC IV bag inserted, maintained and removed correctly? Was everything documented correctly? 23 Cdiff and is placed in isolation lab. After a further two weeks in hospital she goes home to recover. In total she was in hospital for 4 weeks. Discharged home without antibiotics. Home recovering for a further 6 weeks. Why is the infection resistant? Use of antibiotics – if you’re given the wrong antibiotic to start with then you’re using it unnecessarily (it isn’t going to help you). What information might the GP receive from the hospital (and when)? GP’s priorities/concerns? What questions might Helen have asked her GP about what happened to her? How might the GP respond? 24 Appendix II Strengthening our Defences HAI Awareness Event - Action Plan Name: _____________________________________ Date: ______________________________________ As part of the above event you have thought about barriers, actions and support needs in your workplace relating to HAI and associated Standard Infection Control Precautions. This may influence your practice or may provide an educational opportunity for you and your colleagues. Please complete the following template to use as a record of your barrier(s), action(s) and support need(s) and record the outcome or impact on care. Barrier – (What barrier is there to your practice in Infection Prevention & Control?) Action – (What action can you take to improve practice in Infection Prevention & Control?) Support Need – (What support do you need to improve practice in Infection Prevention & Control?) 25 Please tick the Standard Infection Control Precaution/s associated with your action(s) (select all the apply) Hand Hygiene Personal Protective Equipment Respiratory and Cough Hygiene Patient Placement Management of Blood and Body Fluid Spillage Management of Care Equipment Control of the Environment Safe Management of Linen Safe Disposal of Waste Occupational Exposure Management Other aspect of HAI practice- please state Post event – Implementing your action plan in practice What did you do to implement a change in practice? Who was involved? 26 Were you successful or unsuccessful in implementing your action(s)? Why? What has happened as a result of your action(s)? Is there evidence of positive impact in patient care or outcome? Please keep this template of your activity as evidence for your personal development and for discussion with your manager at your development review. 27 For further information: Dr Gill Walker Sarah Freeman Programme Director, HAI NHS Education for Scotland Westport, 102 Westport, Edinburgh, EH3 9DN E-mail: gill.walker@nes.scot.nhs.uk Direct dial: 0131 656 3375 Educational Projects Manager, HAI NHS Education for Scotland 2 Central Quay, 89 Hydepark Street Glasgow, G3 8BW E-mail: sarah.freeman@nes.scot.nhs.uk Direct dial: 0141 223 1436 This resource may be made available, in full or summary form, in alternative formats and community languages. Please contact us on 0131 656 3200 or e-mail altformats@nes.scot.nhs.uk to discuss how we can best meet your requirements. NHS Education for Scotland Westport 102 Edinburgh EH3 9DN www.nes.scot.nhs.uk May 2015 © NHS Education for Scotland 2015. You can copy or reproduce the information in this document for use within NHSScotland and for non-commercial educational purposes. Attribution to NES as the copyright holder must be made. Use of this document for commercial purposes is permitted only with the written permission of NES. 28