Infection Prevention and Control OHSU EMERGING

Infection Prevention and Control
OHSU EMERGING COMMUNICABLE DISEASE RESPONSE PLAN: Ebola Virus Disease, version 10/03/2014
The Response Plan represents current knowledge and subject to change as the situation evolves.
[note: it is recommended that this plan be used electronically, to ensure direct access to all embedded CDC links throughout this document. Links are provided so that the most current recommendations are followed]
For All Suspected and Confirmed Cases:
Patient Screening ED
Ambulatory Clinics
JBT Health and
Wellness Center
(Student Health
Center)
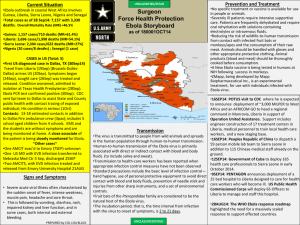
Ebola Virus Disease Case Definitions
TBD
At Triage, EPIC-embedded triage questions will be utilized, which includes symptoms and travel history triggers.
Current list of affected countries: http://www.cdc.gov/vhf/ebola/resources/distribution-mapguinea-outbreak.html#areas
Symptoms: http://www.cdc.gov/vhf/ebola/symptoms/index.html
Upon patient check-in desk, patients will be asked screening questions from a check list
Screening questions will be posted in reception area.
PPE kits will be available at ambulatory sites.
One or more person will be the PPE trainer at each clinic; train-the-trainer model will be utilized.
If an Ebola suspect is identified, the Ambulatory Clinic will notify Infection Prevention and
Control immediately
Testing a Patient for Ebola Virus
Infection: Specimen Collection (blood),
Transport, Testing and Submission
Case definitions are critical in effective communication with other providers, Infection
Prevention and Control Department, and the health department. These include Person Under
Investigation (PUI), Probable vs Confirmed Cases, and the different levels of exposure risk:
http://www.cdc.gov/vhf/ebola/hcp/case-definition.html
ALL Ebola testing must be done in collaboration with the state health department. The infection control department can assist coordination with health department.
Patient specimens will be walked directly to the lab testing area, handed to lab personnel and
1
Infection Prevention and Control
Infection Control
Measures
Patient Placement
Isolation
Precautions and
HCW PPE note in EPIC (that is, “Jane Doe delivered specimen to lab and gave it to Bob Brown”).
Do not send specimens through the tube system.
Do not ship for weekend delivery unless instructed by CDC.
The most updated recommendations are on CDC website, which includes guidance about preferred specimen (blood), specimen storage, and shipping:
http://www.cdc.gov/vhf/ebola/hcp/interim-guidance-specimen-collection-submissionpatients-suspected-infection-ebola.html#update2
Private room with private toilet; for ICU rooms, use commode (dispose in hopper)
Prioritize Airborne Isolation room with an ante-room whenever possible
Use only a mattress and pillow with plastic or other covering that fluids cannot penetrate
Do not place patients in carpeted rooms
Remove all upholstered furniture and decorative curtains from patient rooms before use
Duration of precautions should be determined on a case-by-case basis, in conjunction with local, state, and federal health authorities
Personnel providing patient care will be provided scrubs. Scrubs that are soiled will be discarded in tied double biohazard bags.
2
Infection Prevention and Control
For general care
PPE for the Ebola Response Plan
For potentially splashgenerating procedures
Face Shield or Goggles
N95 Mask
Gown
Gloves
Additional HCW
Requirements
Leg & Shoe Covers
Airborne + Contact + Standard Precautions:
N-95 respirator or PAPR
Fluid impermeable gown
Disposable gloves
Eye protection (Face shield or goggles; googles are preferred)
When blood, vomit or other body fluids present add:
Double gloving
Disposable leg and shoe covers
PPE disposal: Have trash can near area where doffing (removal of PPE) will occur
The number of persons entering the room should be minimized, and include only those providing essential care to the patient (i.e. students or other learners are prohibited). This will minimize the number of potential exposures, and minimize non-essential use of PPE supply.
Each HCW must sign a log upon EACH room entry and exit
3
Infection Prevention and Control
Patient Equipment
Room Monitor
Phlebotomy and
Laboratory
Services
Potential aerosol-generating procedures
Each HCW must review training about correct donning and doffing of PPE prior to room entry
(one training only, unless recommendations change. If recommendations change, all HCW must repeat new training at least once).
Equipment: Dedicated medical equipment for duration of patient hospitalization, preferably disposable, when possible.
A dedicated, high-quality age-appropriate stethoscope should be used and stored in the anteroom in between use. The stethoscope should be properly disinfected after each use.
All non-dedicated, non-disposable equipment used for patient care will be cleaned and disinfected according to manufacturer’s instructions.
A room monitor must be present at room entry at all times:
1.
Maintain room entry/exit log
2.
Ensure each HCW has completed donning/doffing education prior to room entry
3.
Ensure each HCW is wearing appropriate PPE prior to room entry
4.
Observe HCW doffing procedures and hand hygiene compliance
5.
Ensure that stethoscope (and other equipment) are properly disinfected after use.
6.
Limit room entries to essential personnel only.
All laboratorians and other healthcare personnel handing specimens for Ebola testing should be aware of current CDC guidance for collecting specimens correctly, transporting and testing specimens from patients with suspected or confirmed Ebola virus disease:
http://www.cdc.gov/vhf/ebola/hcp/interim-guidance-specimen-collection-submissionpatients-suspected-infection-ebola.html
Limit the use of needles and other sharps as much as possible.
All needles and sharps should be handled with extreme care and disposed in puncture-proof, sealed containers.
Phlebotomy, procedures, and laboratory testing should be limited to the minimum necessary for essential diagnostic evaluation and medical care.
Avoid aerosol-generating procedures when possible
Although there are limited data available to definitively define a list of aerosol generating procedures, procedures that are usually included are those planned ahead of time, such as
bronchoscopy, sputum induction, elective intubation and extubation; and some procedures that often occur in unplanned, emergent settings and can be life-saving, such as cardiopulmonary resuscitation, emergent intubation, and open suctioning of airways
If performing aerosol-generating procedures, perform in a private room, in an Airborne
Isolation room, and wear a fit-checked N95 respirator or PAPR
4
Infection Prevention and Control
Environmental
Cleaning
Conduct environmental surface cleaning following procedures (see section below on environmental infection control).
If re-usable equipment or PPE (e.g. Powered air purifying respirator, elastomeric respirator, etc.) are used, they should be cleaned and disinfected according to manufacturer instructions and hospital policies.
Collection and handling of soiled re-usable respirators must be done by trained individuals using PPE as described above for routine patient care.
Once the patient vacates a room where aerosol generating procedures were conducted, unprotected individuals, including HCP, should not be allowed in that room until sufficient time has elapsed for enough air changes to remove potentially infectious particles.
This link provides a table that can be used to estimate the time necessary to clear the air of airborne pathogens after the aerosol-generating procedure is complete: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5417a1.htm?s_cid=rr5417a1_e#tab1
The patient room will clean at least daily and more often if needed by EVS personnel. Trash must be removed regularly and double bagged in biohazard bags and tied closed. The biohazard bags must be held in ridged containers and burned.
EVS personnel will be trained in PPE donning and doffing prior to being assigned to clean
Environmental Services must review and be aware of the most updated guidance from the
CDC: http://www.cdc.gov/vhf/ebola/hcp/environmental-infection-control-in-hospitals.html
Environmental services staff must wear required PPE, including, at a minimum, disposable gloves (double glove), gown (fluid resistant/ impermeable), goggles or face shield, and N-
95respiratorto protect against direct skin and mucous membrane exposure of cleaning chemicals, contamination, and splashes or spatters during environmental cleaning and disinfection activities
Additional barriers (e.g., leg covers, shoe covers) should be used as needed. If reusable heavyduty gloves are used for cleaning and disinfecting, they should be disinfected and kept in the room or anteroom.
Contaminated equipment is disposed of as regulated medical waste
Use a U.S. Environmental Protection Agency (EPA)-registered hospital disinfectant with a label claim for a non-enveloped virus (e.g., norovirus, rotavirus, adenovirus, poliovirus) to disinfect environmental surfaces in rooms of patients with suspected or confirmed Ebola virus infection
Avoid contamination of reusable porous surfaces that cannot be made single use.
To reduce exposure among staff to potentially contaminated textiles (cloth products) while
5
Infection Prevention and Control
Notification
Responsibilities
Visitors
Postmortem
Attending
Physician
Infection
Prevention &
Control Dept
Other
Notifications, and
Determination of
EOC activation
OHSU Strategic
Communications laundering, discard all linens in double bagged, tied biohazard bags.
Restrict all visitors except in extenuating circumstances. Exceptions must be approved by the
Infection Prevention & Control Department
Prior to first entry, visitors must review training about correct donning/doffing training
Visitors must log in and log out of the room
CDC guidance on postmortem precautions should be reviewed by affected staff prior to handling: http://www.cdc.gov/vhf/ebola/hcp/guidance-safe-handling-human-remains-ebolapatients-us-hospitals-mortuaries.html
The patient’s attending physician will notify and provide details to:
1.
The County Health Department (the county where patient’s resides): https://public.health.oregon.gov/providerpartnerresources/localhealthdepartmentresources/ pages/lhd.aspx
Note: If the County Health Dept cannot be contacted in a timely fashion, the State Health
Department’s Acute and Communicable Disease Program can be contacted (971-673-1111, 24 hrs a day)
2.
Infection Prevention and Control Department
Infection Prevention and Control will notify:
1.
AOD
2.
Logistics
Infection Prevention and Control will notify the Manager(s) and Medical Director(s) of the impacted area(s). The AOD will arrange an urgent meeting to determine next steps (including whether activation of the Emergency Operations Center (EOC) is needed). The meeting participants should include:
1.
Administrator on Duty (AOD)
2.
Administrator on Call (AOC)
3.
Infection Prevention and Control
4.
Occupational Health (during business hours) or Healthcare Human Resources on-call Manager
(after hours)
5.
Risk Management
6.
Strategic Communications
Notify PIO of (1) Oregon State Health Dept, (2) Multnomah County Health Dept and (3) County Health
Dept of the patient’s origin (if different than MCHD)
6
Infection Prevention and Control
EOC Activation vs
Convening a
Smaller
Emergency
Planning Group
Logistics
Occupational
Health and
Human
Resources
Supplies and
Equipment
Employee
Exposure
Exposed
If it is determined that activation of the EOC is indicated, the AOD activates the EOC using the Incident
Command paging group. The EOC (or smaller emergency planning group, if EOC not activated) should consider representation from the following:
1.
AOD
2.
AOC
3.
Infection Prevention & Control
4.
Occupational Health (during business hours) or Healthcare Human Resources on-call Manager
(after hours)
5.
Joseph B. Trainer Student Health Services
6.
Risk Management
7.
Strategic Communications
8.
Laboratory Services
9.
Pharmacy
10.
Logistics
11.
Emergency Department
12.
Inpatient unit(s) and/or ambulatory clinic(s)
13.
Professional services (Radiology, Respiratory Therapy, etc.)
14.
Facilities
15.
Environmental Services
16.
Transportation
Maintain supply chain and inventory
Provide regular supply updates (e.g. every 48 hrs, or more frequently as needed) to Infection
Control and EOC (if active).
Confirm with other local hospitals regarding access issues
Assist with messaging and education to hospital staff and employees about supply issues, as needed (e.g. guidance and instructions about proper re-ordering, prevention of supply hoarding/stealing )
CDC provides some recommendations: http://www.cdc.gov/vhf/ebola/hcp/infectionprevention-and-control-recommendations.html
Guidance will be provided on a case-by-case basis in collaboration with OHSU and health department
CDC provides some recommendations: http://www.cdc.gov/vhf/ebola/hcp/infection-
7
Infection Prevention and Control
Employees who become ill
External Communications
Internal Communications
External patient referral to OHSU
(from public health or a referring healthcare provider) prevention-and-control-recommendations.html
Guidance will be provided on a case-by-case basis in collaboration with OHSU and health
Guidance will be provided on a case-by-case basis
Refer to OHSU Conscientious Objection Policy: https://ohsu.ellucid.com/documents/view/147 department
Employee-work concerns (e.g. refusal to care for a patient with suspected of confirmed disease)
OHSU employees returning from epidemic counties
The following guidance should be followed for returning employees: http://www.cdc.gov/vhf/ebola/hcp/monitoring-and-movement-of-persons-withexposure.html
Early recognition is critical to controlling the spread of Ebola virus. Health care providers
(including Occupational Health) should be alert for and evaluate any patients with symptoms consistent with EVD and potential exposure history
Occupational Health should (1) implement immediate isolation precautions, (2) report to
Infection Prevention & Control Department and (3) county health department of any returning employee with illness that might be Ebola virus disease.
All public/media communications will be managed by Strategic Communications
Strategic Communications will assist in creating and providing messaging to employees, staff, visitors, and public in various methods (e.g. EPIC homepage, Staff News, email, e-STAT). To assure access to the most current information, topics with direct links to the Centers for Disease Control and
Prevention (or state health department) should be utilized whenever possible.
Overview for healthcare providers: http://www.cdc.gov/vhf/ebola/hcp/index.html
Ebola virus disease care and treatment: Clinical guidance: http://www.cdc.gov/vhf/ebola/hcp/clinician-information-us-healthcare-settings.html
Public Health or any external provider/hospital, should they become aware of a patient needing medical evaluation, should contact the ED at 503-494-7911 and request to speak with the ED attending through the OHSU Transfer Center.
The AOD and Infection Prevention & Control Medical Director should be conferenced into the telephone discussion.
8